Updated Guidelines Recommend Adding Pembrolizumab to Neoadjuvant Chemotherapy in TNBC
The ASCO’s expert panel released updated recommendations of pembrolizumab in combination with neoadjuvant chemotherapy for patients with stage II or stage III early triple-negative breast cancer
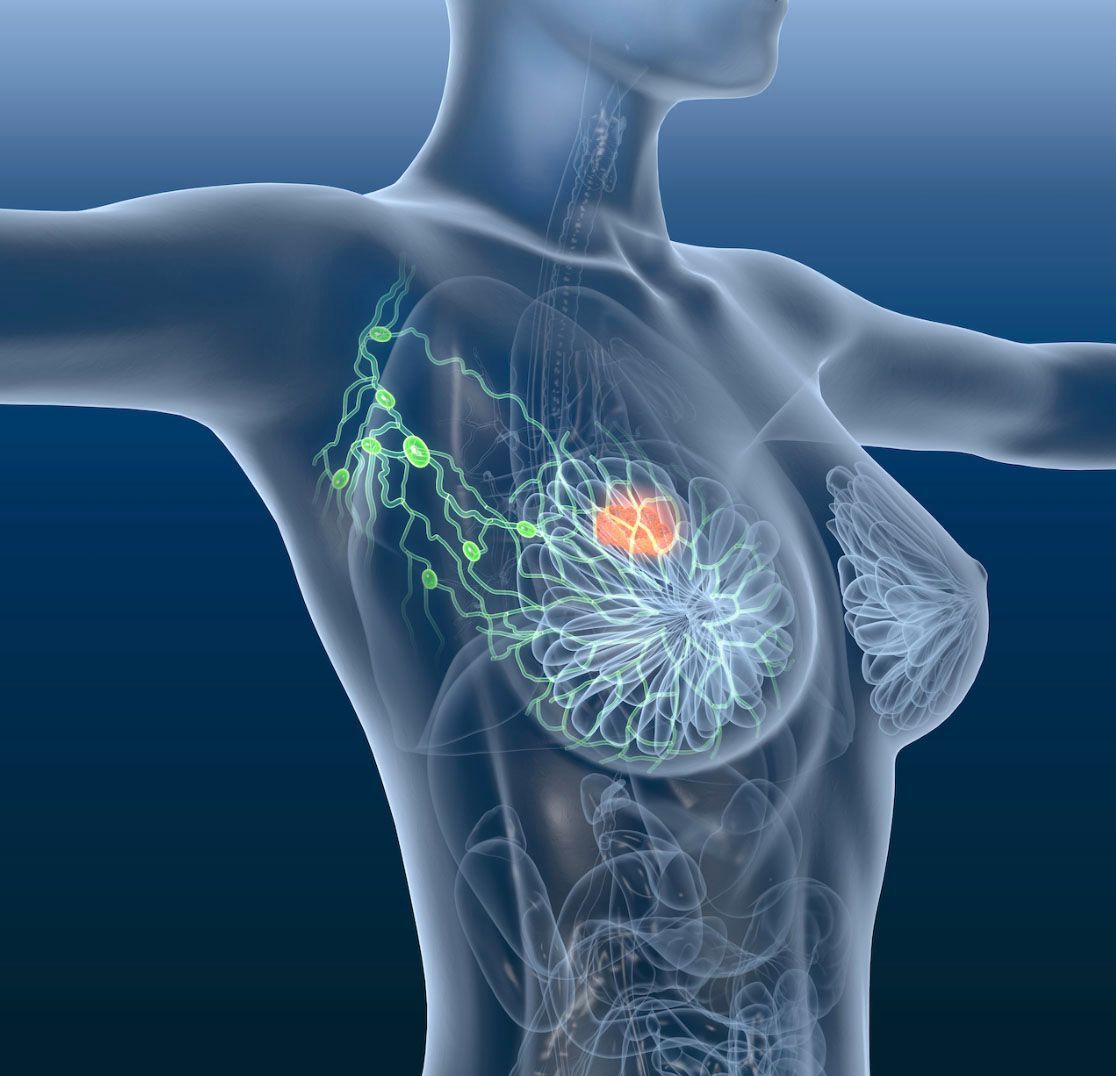
The American Society of Clinical Oncology (ASCO) released an updated recommendation for the use of pembrolizumab (Keytruda), an immune checkpoint inhibitor, in combination with neoadjuvant chemotherapy, followed by adjuvant pembrolizumab, for patients with stage II or stage III early triple-negative breast cancer (TNBC).
The ASCO’s expert panel recommends 200 mg of pembrolizumab once every 3 weeks or 400 mg once every 6 weeks in combination with neoadjuvant chemotherapy, followed by adjuvant pembrolizumab in this case. Additionally, adjuvant pembrolizumab may be given either concurrently with or after completion of radiation therapy.
Evidence for this recommendation was determined from findings from the KEYNOTE-522 study (NCT03036488), which followed 1174 patients with TNBC treated with neoadjuvant chemotherapy plus pembrolizumab (n = 784) vs those who were treated with placebo (n = 390). At a median follow-up of 39.1 months, event-free survival (EFS) in the pembrolizumab arm was 84.5% compared with 76.8% found among patients in the placebo arm (HR, 0.63, 95% CI, 0.48-0.82; P < .001).
In an interview with Targeted Therapies in OncologyTM, Praveen Vikas, MBBS, clinical assistant professor at the University of Iowa Hospitals & Clinics and medical oncologist and a member of ASCO’s expert panel said, “We knew from before that [observing] pembrolizumab in the adjuvant setting significantly improves the pathological complete response. But what came out of this interim analysis was that it not only improves the pathological complete response, but it actually improves long-term outcome such as event-free survival. That resulted in a lot of excitement. And this is the first approval of any immunotherapy agent in early stage triple-negative breast cancer.”
A targeted electronic literature search was conducted to identify phase 3 clinical trials pertaining to the recommendation on immune checkpoint inhibitors in this patient population with stage II or stage III early TNBC. The original expert panel from the previous recommendation reconvened to review the key evidence from KEYNOTE-522 and to approve the revision to the recommendation.
The estimated overall survival (OS) rate at 36 months for the pembrolizumabchemotherapy group was 89.7% (95% CI, 87.3%-91.7%) compared with the estimated OS rate for the placebo-chemotherapy group at 86.9% (95% CI, 83.0%-89.9%). Mortality rates slightly favored pembrolizumab treatment with chemotherapy as 80 (10.2%) of these patients died vs 55 patients (14.1%) in the placebo-chemotherapy group (hazard ratio for death, 0.72; 95% CI, 0.51-1.02). Follow-up is ongoing to further explore OS data.
Grade 3 or higher treatment-related adverse events (TRAEs) occurred across the trial in 77.1% of the pembrolizumab plus chemotherapy arm and in 73.3% of the placebo plus chemotherapy arm. Investigators observed that most adverse events occurred in the neoadjuvant treatment phase compared with the adjuvant phase. The most commonly occurring grade 3 or higher TRAEs were neutropenia, decreased neutrophil count, and anemia in both arms.
Grade 3 or higher were similar across both arms. For example, neutropenia affected 34.5% of patients in the pembrolizumab arm and 33.4% of patients in the placebo arm; neutrophil count decrease affected 18.6% of patients in the treatment arm and 23.1% of patients in the placebo arm; and anemia affected 18.0% in the pembrolizumab group and 14.9% in the placebo group. TRAEs were linked to 4 deaths in the pembrolizumab plus chemotherapy group and 1 death in the placebo plus chemotherapy group.
TRAEs led to treatment discontinuation in 27.7% of patients in the pembrolizumab plus chemotherapy group and in 14.1% of patients in the placebo plus chemotherapy group. Grade 3 or higher immune-mediated adverse events occurred in 12.9% and 1.0% of patients in the pembrolizumab plus chemotherapy and placebo plus chemotherapy groups, respectively.
“When we see a benefit of this magnitude early on in aggressive cancer like triple-negative breast cancer, most likely this benefit is going to hold up,” Vikas added. “Things may change when overall survival data are reported in maybe a year or two from now…regarding this drug pembrolizumab. There are many other immune checkpoint blockers that have been undergoing trials and have had some early data come out. It’s possible that in the future, there will be data from atezolizumab (Tecentriq) and durvalumab (Imfinzi). Based on how [these trials] report on their long-term outcome, there could be further updates in these ASCO guidelines.”
REFERENCE
Korde LA, Somerfi eld MR, Hershman DL; Neoadjuvant Chemotherapy, Endocrine Therapy, and Targeted Therapy for Breast Cancer Guideline Expert Panel. Use of immune checkpoint inhibitor pembrolizumab in the treatment of high-risk, early-stage triple-negative breast cancer: ASCO guideline rapid recommendation update. J Clin Oncol. 2022;40(15):1696-1698. doi:10.1200/JCO.22.00503

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More