TRIO Recommendations Standardize Benefits, Risks for Immunotherapy Agents
ASCO and SITC released a joint statement that outlines new recommendations for reporting data from immuno-oncology clinical trials.
Michael A. Postow, MD
The American Society of Clinical Oncology (ASCO) and the Society for Immunotherapy of Cancer (SITC) released a joint statement that outlines new recommendations for reporting data from immuno-oncology (IO) clinical trials. The Trial Reporting in Immuno-Oncology (TRIO) statement detailing these recommendations was recently published in both the Journal of Clinical Oncology and the Journal for ImmunoTherapy of Cancer. This statement outlines 12 recommendations for reporting clinical trial data that consider the unique efficacy and toxicity characteristics of immuno-therapy treatment.
“The IO field is moving so fast with many agents in development,” said senior author Michael A. Postow, MD, of Memorial Sloan Kettering Cancer Center. “The TRIO guidelines are intended to help standardize our understandings of the benefits and risks of each agent in the published literature.”
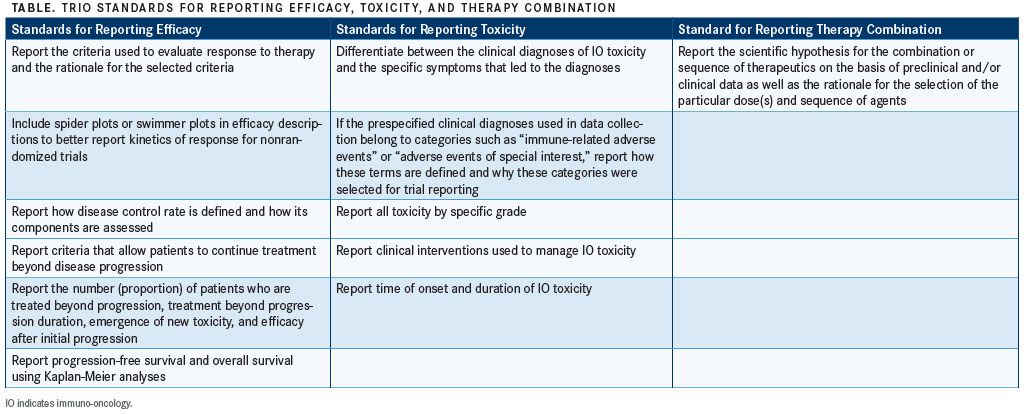
The recommendations were developed by a 2016 working group from members of ASCO and SITC that consisted of medical oncologists, clinical researchers, biostatisticians, and immunologists, as well as government and industry members. The 12 recommendations can be grouped under efficacy data, toxicity information, or details about combination therapies. The following 3 sections reflect this grouping, and the TRIO recommendations are listed verbatim both as bullet points and in the TABLE.
Standards for Efficacy Reporting
• Report the criteria used to evaluate response to therapy and the rationale for the selected criteria
Most clinical trials use the Response Evaluation Criteria in Solid Tumors (RECIST) standards to categorize the efficacy of oncology drugs. Although these specifications have been sufficient for the evaluation of other types of chemotherapy, IO therapies have unique early tumor responses that may be misinterpreted as disease progression. To address this challenge, new criteria have been developed by multiple groups. Although these new criteria are all designed to improve the evaluation and optimize the benefit of IO therapies, no single set has been universally adopted.
The working group does not recommend 1 particular set of criteria, instead stating that it is critical to clearly state which response criteria were used for evaluation and if the criteria were specified before the study was done. There is also a recommendation for investigators to discuss why the chosen criteria were selected. For consistency and comparability across all clinical trials, the recommendations suggest continuing to report the RECIST criteriabased evaluation along with the chosen IO-specific analyses.
• Include spider plots or swimmer plots in efficacy descriptions to better report kinetics of response for nonrandomized trials
Waterfall plots are often used to display trial efficacy data, but the workgroup argues that these types of figures leave out key temporal data that can be important for evaluating the efficacy of a therapeutic. Spider plots show tumor burden over the course of treatment for each patient in a trial. Swimmer plots are useful because they show the duration and onset of response in relation to the time of treatment administration (FIGURE).
One limitation that is noted for the use of spider plots is that data from trials with large numbers of patients can result in plots that are difficult to interpret. Because of this, spider plots are specifically recommended for displaying the results of smaller trials. Additionally, these plots can be useful for displaying interesting results within a subset of patients from a larger trial. Spider plots are recommended for use in addition to waterfall plots.
• Report how disease control rate is defined and how its components are assessed
Composite endpoints, such as “disease control” and “clinical benefit,” can be determined using variable, nonstandardized criteria. To ensure the clarity of the trial methods and the correct interpretation of data, the criteria for these endpoints must be clearly described, including the timing and methods used to assess the criteria. This includes specifically stating the definition of “baseline,” what criteria designate an “event,” and what information is considered to be censored.
• Report criteria that allow patients to continue treatment beyond disease progression
Pseudoprogression is a phenomenon that has been observed in patients receiving IO treatment. In these cases, a patient’s tumor response manifests as an initial increase in lesion number that is followed by a clinical response. Although typical clinical trials cease treatment if a patient exhibits progressive disease, because of the potential for pseudoprogression, patients in IO clinical trials are often permitted to continue receiving therapy despite initial disease progression.
In most cases, patients in IO trials with progressive disease can continue to receive treatment if they exhibit improved clinical condition and are not suffering from significant AEs, but there are no universal guidelines dictating this decision. To accurately depict the instances of pseudoprogression, it is necessary to thoroughly document these cases. There are no universally accepted protocols for reporting pseudoprogression data, so the work group recommends reporting both the criteria used to determine whether a patient should continue to receive treatment as well as the outcomes of treatment following progression.
• Report the number (proportion) of patients who are treated beyond progression, how long the treatment beyond progression lasts, emergence of new toxicity, and efficacy after initial progression
In addition to clearly stating the criteria used to determine whether a patient could proceed with treatment after disease progression, the outcomes of treatment continuation should be reported. The recommendations suggest reporting the number of patients who experienced a response following postprogression treatment and those patients who ultimately experienced progression. Other details surrounding postprogression treatment should also be reported, including the time of treatment until discontinuation. If any new toxicities emerge or existing toxicities worsen, they should be reported. These reports are key to understanding pseudoprogression and will improve patient care.
• Report progression-free survival and overall survival using Kaplan-Meier analyses
The use of Kaplan-Meier analysis allows investigators to evaluate the correlation of progression-free survival or overall survival with therapeutic response. The value of this method is that survival over time can be computed despite the occurrence of censored observations. Censored observations should be reported, and progression should be reported from the earliest observation.
Whereas Kaplan-Meier survival curves for IO trials can exhibit features that are distinct from those of other trials, this recommendation stands for all types of clinical trials. As with the other recommendations, any statistical methods employed in a study should be clearly stated and thoroughly described.
Standards for Toxicity Reporting
• Differentiate between the clinical diagnoses of IO toxicity and the specific symptoms that led to the diagnoses
In some cases, initial patient symptoms can culminate in a diagnosis of IO toxicity. These data can be confusing if it is not made clear that the symptoms and the diagnosis are part of the same event. When reporting data from these patients, investigators must clearly and separately describe both the symptoms and the clinical IO toxicity diagnosis. The criteria used to determine IO toxicity should also be described. The standard for IO toxicity reporting has been outlined by the National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE). The CTCAE guidelines describe the symptoms and reporting requirements for diagnosing IO toxicity in patients.
• If the prespecified clinical diagnoses used in data collection belong to categories such as “immune-related adverse events (AEs)” or “AEs of special interest,” report how these terms are defined and why these categories were selected for trial reporting
Often, immune-related AEs are reported separately from other AEs as IO toxicities. In these cases, the criteria for differentiating the 2 categories should be clearly stated, and the toxicities included in either category should be listed. Both the criteria and the categorization choices should be explained.
• Report all toxicity by specific grade
There are important differences between each toxicity grade, particularly in the case of IO toxicities. Despite the common practice of only reporting grade 3 and 4 toxicities separately, the working group recommends individually reporting the grade of each observed toxicity. A suggested method for reporting this information in a chart is by placing events in separate columns that correspond to the event severity.
This point is important because for many therapeutics, grade 2 or higher toxicities require withholding treatment. Yet many trials have not independently reported grade 2 toxicities. Amending this practice will increase the available information describing important IO toxicities and will add important details to what is known about the toxicities associated with different IO therapies.
• Report clinical interventions used to manage IO toxicity
In addition to reporting the criteria for diagnosing IO toxicity events, investigators should indicate how the most common events were managed. In cases of significant or unexpected toxicities, study authors should discuss how the reported IO toxicities were treated.
As multiple organizations have released guidelines for managing IO toxicities, investigators should discuss whether the management strategy employed in a study adhered to any specific set of guidelines.
• Report time of onset and duration of IO toxicity
Temporal information is a key component of a compound’s toxicity profile and should be included in toxicity reports. Both the time of onset and the duration of the toxicity event are important to understanding how patients respond to IO therapeutics.
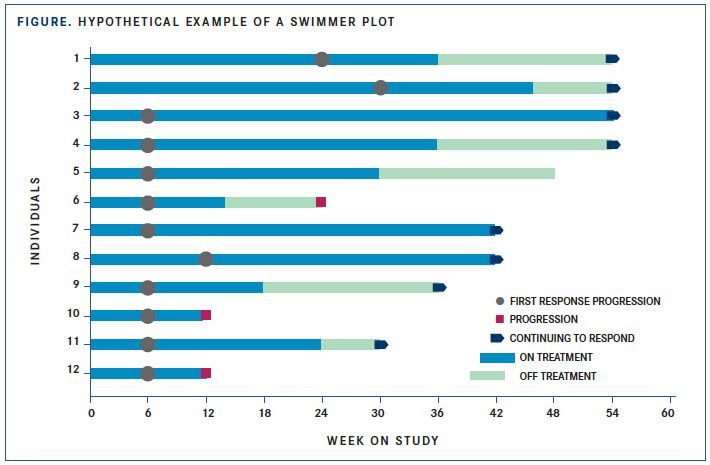
In particular, this information will be informative for evaluating combination therapies, into which IO therapies are often incorporated. Toxicity profiles may look similar between monotherapy and combination therapy, but the time of onset or duration of a toxicity event may be compounded when the therapeutics are combined, for example, in the form of an earlier onset or longer duration of toxicity. These important changes in patient response to therapy are lost if time is not reported. The work group recommends including this information in the form of modified swimmer plots or other plots that convey toxicity onset and duration.
Standards for Reporting Therapy Combination
• Report the scientific hypothesis for the combination or sequence of therapeutics on the basis of preclinical and/or clinical data as well as the rationale for the selection of the particular dose(s) and sequence of agents
When evaluating combination therapies, it is critical to provide justification supporting the tested combination. Supporting data should be used to make a strong argument for the hypothesis that the combined therapies will produce a synergistic, beneficial effect. Significant consideration should be put into the dosage selection for combination therapies, as well as the sequence of administration. These decisions should be thoroughly described; the working group recommends summarizing the dosage, sequencing, and temporal treatment information within a figure.
These recommendations were developed in consideration of the unique characteristics of IO therapy treatment regimens and seek to improve the quality of data reported from IO clinical trials. By publishing more complete reports detailing patient responses to IO therapies and the criteria used to evaluate those responses, more useful data will be made available. This additional information will provide deeper insight into the risks, benefits, and clinical outcomes of treatment with these therapies, leading to a better understanding of patient responses and an increase in the quality of patient care.
Reference:
Tsimberidou AM, Levit LA, Schilsky RL, et al. Trial reporting in immuno-oncology (TRIO): an American Society of Clinical Oncology-Society for Immunotherapy of Cancer statement. J Clin Oncol. 2018;6(1):108. doi: 10.1186/s40425-018-0426-7.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More