Trifluridine-Tipiracil, Bevacizumab Continue to Show Survival Benefits in mCRC
Real-world research show the tolerability and effectiveness of trifluridine and tipiracil combined with bevacizumab for the treatment of patients with refractory metastatic colorectal cancer.
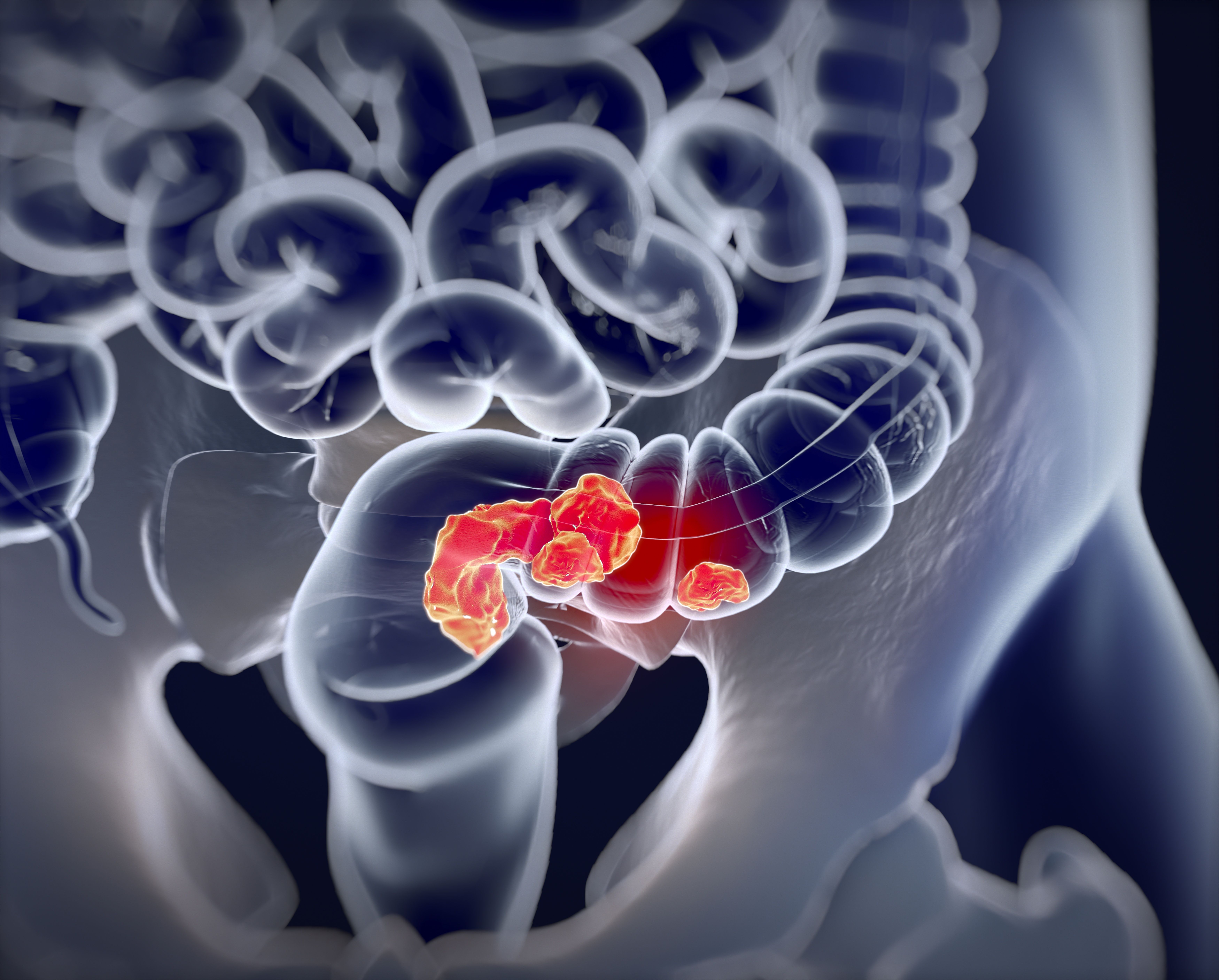
Findings from a real-world, retrospective, open-label phase 2 trial provided further evidence that the combination of trifluridine and tipiracil (Lonsurf) plus bevacizumab (Avastin) was well tolerated and effective in Western patients with refractory metastatic colorectal cancer (mCRC). Investigators reported that the objective response rate (ORR) was 3% and the disease control rate was 71%. After a median follow-up of 8 months (range, 2-39), the median progression-free survival (PFS) was 6 months (95% CI, 3.1-8.9) and the median overall survival (OS) was 14 months (95% CI, 10.1-17.8).1 The combination showed promising activity and safety in prior clinical trials in patients who were refractory or intolerant to or ineligible for 5-fluorouracil– based combination treatment.1
Thirty-one patients received the trifl uridine- tipiracil and bevacizumab regimen, which consisted of trifl uridine-tipiracil administered orally at a dose of 35 mg/m2, delivered twice daily on days 1 through 5 and 8 through 12 in a 28-day cycle. Bevacizumab was administered intravenously at a dose of 5 mg/kg, delivered every 2 weeks in a 28-day cycle.
The median age was 69 years (range, 38-82), 39% were men, and all patients had an ECOG performance status of 0 or 1. Regarding tumor location, 77% of patients had left-sided tumors and 54% had synchronous presentation. Regarding mutation status, 35% had a RAS mutation a nd 3% had a BRAF mutation. Fifty-eight percent had known microsatellite instability (MSI), with 16.7% (3 of 18) displaying an MSI-high profile. Regarding disease spread, 96% of patients had 3 or fewer sites involved, 64% had liver metastases, 55% had lung metastases, and 23% had peritoneal involvement.
Univariate analysis revealed that a longer median PFS was associated with patients who were 65 years or older (8 months vs 5 months; HR, 0.61; P = .29) and were men (8 months vs 5 months; HR, 0.49; P = .17). Shorter median PFS was associated with RAS mutation status (5 months vs 8 months; HR, 1.1, P = .85), the presence of liver metastases (5 months vs 9 months; HR, 1.64; P = .33), right primary tumor (5 months vs 6 months; HR, 1.82, P = .34), and more than 3 lines of previous treatment (3 months vs 8 months; HR 1.33; P = .56). However, the investigators noted that none of these differences were statistically significant.
Regarding safety, adverse events of any grade were reported in 58% of patients, and the most common grade 3/4 toxicities reported were neutropenia (19%) and anemia (6%). Thirty-five percent of patients required dose delays or dose reductions. Granulocyte colony-stimulating factor was given to 19.3% of patients (6 of 31) as primary prophylaxis, and the growth factor was given as secondary prophylaxis in 16.1% (5 of 31) of patients. Sixty percent of the patients who discontinued treatment eventually received 1 or more lines of subsequent therapy, with 8 of 12 (66.7%) receiving regorafenib (Stivarga).
Investigators reported that despite the small sample size and lack of statistical significance, subgroup analysis led to hypothesis generating research and was consistent with previously reported studies.2,3 The investigators wrote that the combination appeared to be well tolerated and was an effective option in pretreated patients with mCRC, “especially those with RAS wild-type, left-sided tumors.” Stronger benefit was observed in patients without liver metastases, and earlier implementation of the regimen in the continuum of care also demonstrated benefit.
In the refractory setting, current treatments that are available include regorafenib and trifluridine-tipiracil as single-agent therapies. Grothey et al4 reported that regorafenib monotherapy resulted in an ORR of 1% and median PFS and OS of 1.9 months and 6.4 months, respectively. Median OS was 6.4 months in the regorafenib group vs 5.0 months in the placebo group (HR, 0·77; 95% CI, 0.64-0.94; 1-sided P = .0052).
REFERENCES:
1. Arrichiello G, Perrone A, Napolitano S, et al. Real-world activity and safety of trifluridine-tipiracil plus bevacizumab therapy in patients with refractory metastatic colorectal cancer. Target Oncol. 2022;10.1007/s11523-022-00916-8. doi:10.1007/s11523-022-00916-8
2. Kuboki Y, Nishina T, Shinozaki E, et al. TAS-102 plus bevacizumab for patients with metastatic colorectal cancer refractory to standard therapies (C-TASK FORCE): an investigator-initiated, open-label, single-arm, multicentre, phase 1/2 study. Lancet Oncol. 2017;18(9):1172-1181. doi:10.1016/S1470-2045(17)30425-4
3. Kotani D, Kuboki Y, Horasawa S, et al. Retrospective cohort study of trifluridine/tipiracil (TAS-102) plus bevacizumab versus trifl uridine/ tipiracil monotherapy for metastatic colorectal cancer. BMC Cancer. 2019;19(1):1253. doi:10.1186/s12885-019-6475-6
4. Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):303-312. doi:10.1016/S0140- 6736(12)61900-X