Systemic Therapy for Advanced Hepatocellular Carcinoma: ASCO Guidelines
In the past 3 years, the FDA has approved 7 novel drugs, either given alone or in combination, to help treat patients with hepatocellular carcinoma.
Renuka Iyer, MD

In the past 3 years, the FDA has approved 7 novel drugs, either given alone or in combination, to help treat patients with hepatocellular carcinoma (HCC).1
Although there are more medications now than ever before, no head-to-head comparisons of them were done in clinical trials, said Renuka Iyer, MD, in an interview with Targeted Therapies in Oncology. Many were studied versus placebo, explained Iyer, who is codirector of the Liver and Pancreas Tumor Center at Roswell Park Comprehensive Cancer Center in Buffalo, New York. Therefore, understanding how to best treat a patient based on the rapidly evolving data is not clear.
“There have been multiple changes over the last few years, so it’s necessary to provide some general guidance to have something that clinicians can go to for the specific questions surrounding systemic therapy,” said William P. Harris, MD, an associate professor in the Division of Oncology at the University of Washington School of Medicine in Seattle.
Iyer and Harris served on an expert panel assembled by the American Society of Clinical Oncology (ASCO) that outlined key guidelines for systemic therapy for advanced HCC, which were published in the Journal of Clinical Oncology.2
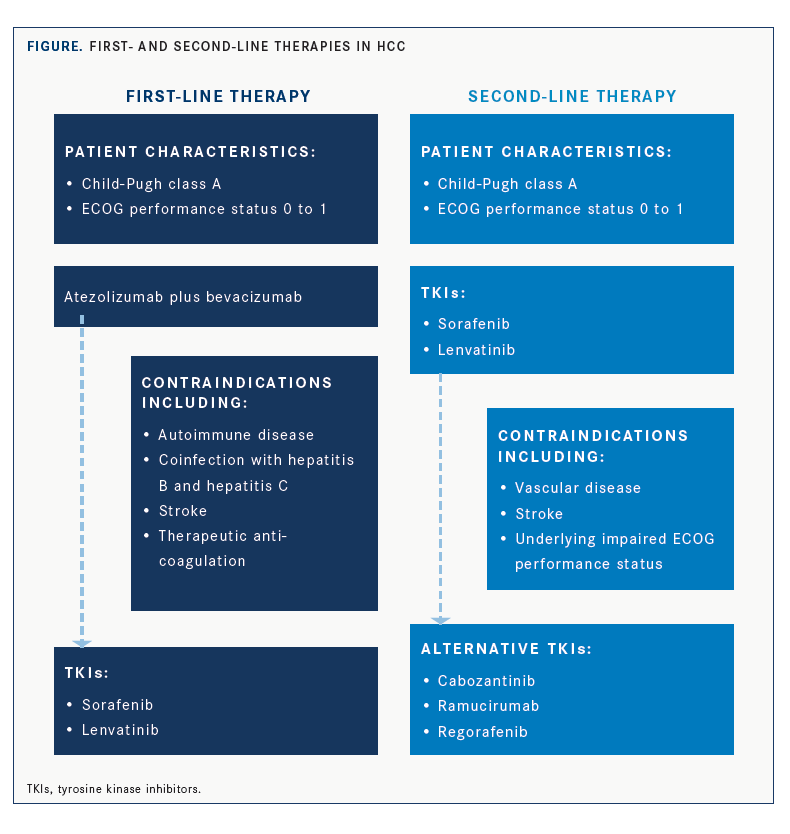
Updates to first- and second-line treatments were detailed with considerations to Child- Pugh classification and ECOG performance status (FIGURE). Targeted therapies, such as bevacizumab (Avastin); tyrosine kinase inhibitors (TKIs), such as sorafenib (Nexavar) or lenvatinib (Lenvima); and the immune checkpoint inhibitors atezolizumab (Tecentriq), pembrolizumab (Keytruda) and nivolumab (Opdivo) were all included as potential treatment options. The panel was able to establish a new, preferred first-line regimen that can be reinforced to make sure patients are considered for it upfront.
“Having more options will impact [patients’] ability to access these treatments, which weren’t available, and potentially have longer survival than they would have without them,” Iyer said. “It’s encouraging to see that several of these agents are giving sustained radiographic response and are well tolerated.”
First-line Therapy
Most patients with advanced HCC may be given the combination of atezolizumab and bevacizumab upfront if they have Child-Pugh class A liver disease and an ECOG performance status of 0 to 1. In addition, this regimen may be offered following management of esophageal varices, when present, according to the ASCO guidelines.2
This recommendation was based on the interim analysis of the randomized phase 3 IMbrave150 clinical trial (NCT03434379), whose results demonstrated that atezolizumab plus bevacizumab was superior to sorafenib, the prior standard of care for advanced HCC.3
“This should be the preferred regimen at this time point for most patients with HCC in the first-line setting,” Harris said. “[Sorafenib] remains reasonable. But, in the absence of a contraindication, atezolizumab plus bevacizumab has the best efficacy data from any randomized phase 3 study, and that’s what drove this recommendation.”
In addition, Iyer discussed the study’s compelling data for overall survival (OS), which at 12 months was 67.2% (95% CI, 61.3%-73.1%) with atezolizumab and bevacizumab and 54.6% (95% CI, 45.2%-64.0%) with sorafenib.3 “The hazard ratio for OS was 0.58 [95% CI, 0.42-0.79; P = .0006],…an over 40% improvement over established therapy that had held its ground for more than a decade in this patient population,” she said. “[Adding to this], quality of life and the toxicity profile was quite modest.”
Despite promising OS findings, adverse events were greater in the atezolizumab and bevacizumab arm, with a risk of bleeding complications with bevacizumab.3 Because of this, the expert panel urged caution when applying the results to patients with more advanced liver disease. Harris explained that within 6 months of beginning therapy, patients should undergo an esophagogastroduodenoscopy, which may not be in an oncologist’s routine patient flow.
Patients with contraindications, including autoimmune disease, coinfection with hepatitis B (HBV) or hepatitis C (HCV), or stroke, or those receiving therapeutic anticoagulation, should skip atezolizumab and bevacizumab and begin therapy with a tyrosine kinase inhibitor (TKI). Either sorafenib or lenvatinib would be appropriate, the panel noted.2
Second-line Therapy
Should a patient’s disease progress on atezolizumab and bevacizumab, and they are Child- Pugh class A and have an ECOG performance status of 0 to 1, they may be given either sorafenib or lenvatinib as second-line therapy.2
“This is an extrapolation of data and is basically not based upon randomized data at this point,” Harris said. “But this is a consensus from the expert panel, and these are the situations where we think we need to provide guidance to clinicians as to what to do when there is an absence of randomized data. The data have been moving so quickly that the trials have not caught up.”
Although age is not a factor when considering who can receive TKI therapy, comorbidities need to be integrated, he added. For instance, in patients who have significant vascular disease or underlying impaired ECOG performance status, or in those who have had a stroke, clinicians should exercise caution.
Additional options for second-line treatment would be to use another TKI, such as cabozantinib (Cabometyx), ramucirumab (Cyramza), or regorafenib (Stivarga). “We know there is robust randomized data in phase 3 trials to support the use of multiple agents in that setting,” Harris said. “Regorafenib applies to patients who have previously tolerated sorafenib but subsequently progressed.4 Ramucirumab has only proven to be effective in patients who have an alpha-fetoprotein [level] of 400 ng/mL or higher in the second-line setting.5 And then there are less restricted agents like cabozantinib.6 All these agents were studied in patients with relatively intact hepatic functions.”
Iyer added, “These [agents] could all be considered as equivalents as recommended for second-line therapy following atezolizumab and bevacizumab. [However,] the quality of the evidence [after] studying all these agents… is not high because they were not all studied following [the combination].”
The expert panel also addressed the idea of returning to some of these TKIs should a patient progress on one over the other. Further, immune checkpoint inhibitors may also play a part in second-line therapy for patients with advanced HCC. The panel suggested the use of pembrolizumab or nivolumab in patients who have contraindications for atezolizumab and bevacizumab or who cannot tolerate TKIs.2
“There are data that are very close to being positive but just missed statistical significance for a variety of reasons. [However], the panel agreed that there is clear efficacy to these agents,” Harris explained. “There remains a role for checkpoint-based therapy, either PD-1 inhibitors or potentially combination immunotherapy, in the second-line setting.”
Data are evolving on the use of nivolumab and ipilimumab (Yervoy) in patients with good performance status and Child-Pugh class A in the second-line setting. At some time in the future, there could also be a role for these agents.7
Are Combinations the Future?
Despite an abundance of agents, many unanswered questions remain, according to Harris. Looking to the future, he hopes that experts can optimize the data with clinical trials to help sort out the ideal sequence of drugs. “Although we provide recommendations, it is going to be important to continue to do trials to show what is the relative benefit of 1 second-line agent versus another,” he said.
Along those lines is the idea of exploring adjuvant therapy in this space. “For the patients who can undergo resection, can we actually prevent recurrence with adjuvant therapy?” Harris asked.
The need for new agents remains important, too. “There are at least 3 major first-line clinical trials that are near completion and should be released over the next year,” Harris said. “These are investigating other combinations that could be equivalent [to] or potentially supplant frontline therapy.” The trials include combinations of immunotherapy plus TKIs, such as cabozantinib with atezolizumab versus sorafenib in patients with advanced disease who haven’t received prior systemic therapy, or combinations of PD-1 or PD-L1 plus a CTLA-4 inhibitor.8-10
Phase 1 clinical trials are also examining T-cell therapies and combinations of local therapy plus systemic therapy in patients with HCC. An example is catheter-based interventions in combination with systemic therapy, so either chemoembolization or radioembolization plus or minus systemic therapy, Harris explained.
It will also be crucial to look at subgroups of patients to see which may do better, he continued; this may be based on comorbidities or what drove the cancer to begin with. “We have to consider that there are many patients who have contraindications or relative contraindications to drugs that inhibit vascular endothelial growth factor and these immunotherapy-specific combinations, but even more so in that subgroup of patients.”
Specifically, the panel commented on the need for more data to support treatment benefit in patients with a Child-Pugh class B score.2
Iyer addressed the unmet need for genetic and biomarker understanding to also help guide treatment decisions in advanced HCC. Although a subset of patients with HCC were found to have FGF19, a targetable driver, and there have been some early data on the development of FGFR4 inhibitors, the panel commented that the efficacy and appropriate context of their use is yet to be determined.11
A Multidisciplinary Approach
“In terms of when a medical oncologist meets a patient with HCC, there are now new important things they need to know to determine whether it’s a safe choice…like incorporating variceal screening with an upper endoscopy more routinely into patient flow when they identify a patient with HCC,” Harris said. “That’s going to be an important step to expedite therapy for patients.” This means that changes to medical practice may be needed.
A remaining critical component in the care of patients with HCC is making sure they are evaluated by a multidisciplinary liver tumor clinic.
“While this blessing of [many treatment options] is a wonderful thing, [we] are also given the responsibility of using it wisely, and that I think is something we are hoping to learn from each other, prospective data, and clinical trials,” Iyer said.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More