Roundtable Discussion: Participants Review the Potential Toxicities of Hedgehog Inhibitors in Basal Cell Carcinomas
Meredith McKean, MD, MPH, moderated a Case-Based Roundtable discussion about a 88-year-old patient with Basel cell carcinoma.
Meredith McKean, MD, MPH
Meredith McKean, MD, MPH, a medical oncologist, Tennessee Oncology and Sarah Cannon Research Institute, moderated a Case-Based Roundtable discussion about a 88-year-old patient with Basel cell carcinoma.
MCKEAN: [When] looking at [a basal cell carcinoma] tumor and the location of it, the NCCN [National Comprehensive Cancer Network] guidelines1 divide out low risk versus high risk in the different features: low risk being on the trunk, extremities, less than 2 cm, borders are well defined, [the tumor] is not at a site of prior radiation therapy, and then the subtypes are sub-nodular and superficial. Some of the high-risk features then are certain areas of the face. If this has been growing quickly, if it’s involving some of the nerves.
These risk factors, while they’re now being incorporated into some clinical trials, this ends up being important information for all of you. So, I don’t know if any of our radiation oncologists wanted to weigh in about what does the low vs high risk mean to you, and how does that help when you see these patients?
WILLIAMS: Radiation oncologists, think kind of like surgeons, but we don’t have knives; that’s the difference. So, when you look at the tumor on someone’s face, you look at it the way a surgeon would look at it—where it is, what’s around it.
Two things popped up in my mind. One, [with] it being on the nasal ala, if you do surgery there you can just take out the entire side of the right nose, which would be disfiguring and probably prone to all kinds of problems. Then the second thing is that the patient is 88 years old, so they’re going to have thin skin that takes longer to heal.
So, at some point you could include radiation in this patient’s care, obviously not upfront, but it’s better for radiation than for surgery, I would say, ultimately.
MCKEAN: [Considering] this patient’s high risk for recurrence, leading into Dr Williams’ point, what are the treatment options? [Starting] with the radiation and surgery discussion first, as Dr Williams was alluding to. I don’t know if you had another thought there on some of the local therapy options for this patient?
WILLIAMS: The sheer size of it and the fact that it’s already ulcerated means that going through radiation would be very difficult. From the size of it and the fact that it’s already ulcerated, I would favor a systemic option to shrink this thing down, because it’s too nasty for radiation right now.
JONES: It’s a reasonable thought, to echo and talk about those risk factors a little more. Probably many of us have worked in markets where the subspecialty trained surgeons with some very creative reconstructive options, we’ve seen them take on cases such as this, but they’re not realistically available in most of our communities. I can’t say I’ve overlapped on a case like this in Nashville where I’ve seen surgeons attempt an approach like this.
Those high-risk factors, though, seeing that we don’t have pure basal-specific literature on a lot of those, but they help
us know if we have one resected—like the immunocompromised [have] a higher risk of recurrence. Perineural invasion is like bread and butter for a radiation oncologist. Upfront there’s not really guidelines on imaging in evaluating this patient, but if they had worrisome clinical symptoms, we’d get an MRI, probably to look for perineural invasion. If we found that on time of surgery, that would lead us to offering adjuvant [therapy].
As Patrick said, this would be gnarly to go with definitive radiation upfront, but if surgery was refused, it’d have to be part of the discussion.
MCKEAN: So, the NCCN guidelines—if we’re looking at systemic therapy for these patients with locally advanced disease where we know surgery and radiation are going to be challenging, the options are Hedgehog pathway inhibitors. The NCCN guidelines [are even] prefacing the challenges. So, due to frequency of intolerable [adverse events (AEs)] associated with Hedgehog pathway inhibitors, drug holidays or alternatives to daily dosing can be used.
So, the excitement this year was that approved immunotherapy has now come to basal cell carcinoma. In February, the FDA approved cemiplimab [Libtayo] for patients with locally advanced basal cell carcinoma.2 In the label it does say for patients previously treated with a hedgehog pathway inhibitor, or for whom a Hedgehog pathway inhibitor is not appropriate. So, granted accelerated approval for cemiplimab for metastatic patients previously treated, or for whom a Hedgehog inhibitor is not appropriate.
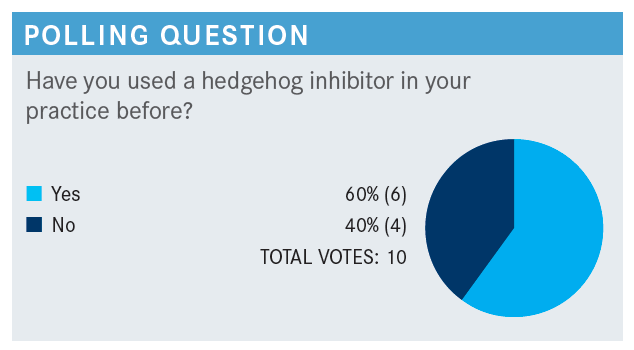
MCKEAN: Anyone that said yes have some initial thoughts of your experience and what that has looked like for your patients?
KHASAWNEH: I did use it in 1 case with basal cell. I was really on the bandwagon for immunotherapy for cutaneous cancer early on, and I did approach our radiation oncologists about the use of immunotherapy in cutaneous cell cancer after I saw promising and encouraging early data for the use of immunotherapy in skin cancer.
On top of that, our radiation oncologists actually have a lot of cutaneous cancer [cases] that my other medical oncology colleagues did not feel comfortable using immunotherapy. I agree with our radiation oncologists who answered earlier that in those patients, the problem is the location of most of the cutaneous cancers are in areas where you cannot deliver high doses of radiation, or the patient prefers not to use radiation.
I’ve had good luck with immunotherapy. Hedgehog inhibitors, I have previous experience [with them] in acute leukemia, and I did see the horrible AEs. I had a patient, actually, with advanced basal cell cancer that I had to use the hedgehog pathway, and that patient could not tolerate more than 3 weeks of the hedgehog pathway inhibitor, and I had to take him off of that.
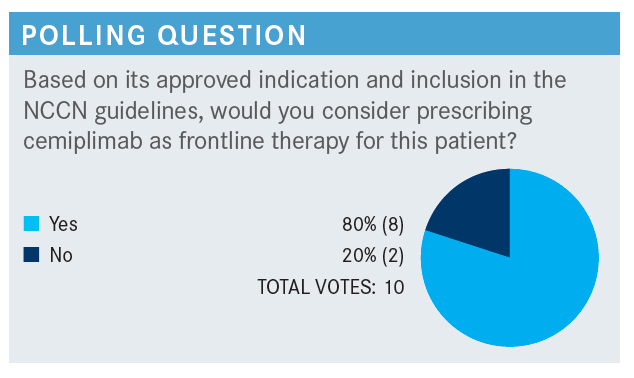
MCKEAN: Anyone want to jump in there and discuss if these are the patients that we see, so if there was a patient like this that came into your clinic, what would prompt you to start with cemiplimab for that patient?
SHEPARD: I’m a general medical oncologist. I guess it really hinges on that phrase of “not a good candidate for Hedgehog inhibitor treatment.” Knowing that the hedgehog inhibitors are not well tolerated, and also have to have drug holidays and things like that.
My experience of giving it to 1 patient who had 2 separate basal cell [cancers] on the trunk, on the shoulders, had a good response, and says they took it every day for 3 months, as prescribed. I’m not 100% sure about that. He had a good response and then was planning to have a holiday of several months, and then was kind of lost to follow-up. Not sure what happened with that patient.
But, an elderly patient over 80, you worry about their ability to tolerate predictable AEs from that. Obviously, there’s catastrophic AEs from immune checkpoint inhibitors too, but I think I would consider doing that.
WASELENKO: I wanted to ask: response rate as a single agent in locally advanced is about 30%. So, are there data that look at combining this with radiation therapy? Is there a radiation-sensitizing effect? So, is there some synergy? Would there be any excess toxicity with the combination?
MCKEAN: Well, I know there’s ongoing studies, but I’m sure our radiation oncologists have some experience.
JONES: Cemiplimab itself has been reported very rarely, I think. There’s a couple small papers, small sample size, describing studies that had done it concurrently [where] it didn’t seem to add toxicity. We have been on our radiation oncology side exploring retrospectively patients who had received concurrent immunotherapy of various forms, similarly structured drugs, without detecting increased toxicity there.
We’re a mixed bag, I think, in radiation oncology and medical oncology, of people who believe in that hopeful synergy of the 2, and how do you time it. [With radiotherapy], you’re releasing some of these antigens for the immunotherapy to help the body identify, you deliver it at the same time. I don’t think we’ve teased out all that.
I wouldn’t be worried about added toxicity. From everything we’ve learned from the other immunotherapies, even though some of that has been not widely reported concurrently, that’s a great question, and that’s the concern I think every time of what is the response rate of cemiplimab with squamous [cell], with basal, and are we going to take that chance and potentially miss our window for our definitive option as it grows to where it’s terrible?
WILLIAMS: One thing that I meant to say earlier is that in the very beginning if this mass was bothering the patient you could consider like a 3- or 4-day course of palliative radiation to get it to stop bleeding and oozing, and then move on to cemiplimab.
But yeah, as far as studies, usually it’s phase 1 is the first step, which is, is it safe, not so much is it effective. So, maybe 10 years from now we’ll be looking at is it synergistic; that kind of occurs later.
MCKEAN: I think those are all great points, because I think right now it does feel very siloed that we have these different therapies, but how to best use them, combine them, sequencing—I think there’s still a lot to learn there.
MCKEAN: So, for how long would you treat this patient?
SHEPARD: I guess not having a huge amount of experience with it, it’s easy to gauge response because it’s right there for the world to see, so I would re-do best response and then maybe 3 weeks past best response, if possible, and then re-assess the possibility of doing a definitive course of radiation, if that’s possible. I would stop the drug during radiation.
MCKEAN: No, I think that’s great. And Shepard, to your point, saying you don’t have much experience, I think that’s the challenge with basal cell, that these patients present to every clinic, and everyone sees a few, so it’s just learning from everyone’s experience. So, I think you’re right. I think with the Hedgehog inhibitors, one strategy that a lot of people are adapting is saying, “Hey, let’s try this for 2 or 3 months, see the best response, how you’re tolerating.” Any other thoughts? Any other patient experiences?
JONES: I’ll tell you what; if it’s a case like this [that is], as far as we can tell not metastatic, if a radiation oncologist hasn’t seen the patient yet, you could document on imaging before starting drug therapy so we know the original extent that we can cover that full area if they have an excellent response. That helps us for sure, vs the piecemeal clinic or cell phone pictures, which we at times have to use to gauge where do I need to cover my treatment.
MCKEAN: And is there a preferred imaging modality?
JONES: All are available. MRI is wonderful in soft tissue extended disease, but CT for that one would probably work out just fine. We’d take either.
MCKEAN: For example, a patient that’s saying, hey, I’m having numbness or tingling across my cheek, those patients in particular, [have to make] sure that imaging is done. I’ll say, I’ve sat at focus groups with other academic center skin cancer experts, and there’s no consensus [on schedule]. Some will say, well, if I make changes there’s no consensus. So, regardless if you’re treating 1 per year or 20 per year, there’s different strategies. I think it ultimately just comes down to each patient.
MCKEAN: So, what are some of the expected AEs of this medication? How do you manage these toxicities?
I can say, I had a patient, she was probably about 70 that started the medication. I felt like we had counseled her well, and she ended up having severe reflux that she hadn’t mentioned to us, but it was so severe she thought she was having a heart attack. So, next thing I knew she was in the hospital for a cardiac workup. They ruled her out with troponins, but it was so unfortunate because I thought, “we’ve talked about this, she understands there’s GI [gastrointestinal] AEs, change in taste, let us know.” And in talking with her, I think she knew that those AEs were from treatment, but she wanted so desperately to stay on treatment because the plan was to go to surgery. So, even when patients know the AEs, they still want to try to push through, or don’t really call in and let us know despite our best efforts.
KHASAWNEH: Each one of us get those patients. The gentleman I treated was 88 with basal cell cancer, and he had significant muscle spasm when I put him on [Hedgehog pathway inhibition], and a lot of GI AEs, mostly nausea and vomiting.
MCKEAN: Did you end up ending treatment earlier than you had hoped to because of the AEs?
KHASAWNEH: Yeah, he was admitted twice for pain after 4 weeks, and the second admission was after we held the drug, and he decided that he doesn’t want to get any systemic treatment [anymore].
MCKEAN: And I think that’s a real issue. I think once they’ve had a bad experience then even if you try to explain that we have a completely different type of treatment, it can be hard to convince them that they want to do any treatment, especially at that age.
MCKEAN: So, for this patient, what would you do next?
Any other triggers for you that [would make you want to] switch from a Hedgehog inhibitor?
KANDRA: How about topical 5-FU? Is it still being used?
MCKEAN: Great question. So, there aren’t any approved topical therapies, but I haven’t tried it. I don’t know if others have had success or have seen that used.
WILLIAMS: A lot of the patients I see will be prescribed that by their dermatologist, and it’s funny, they use it the way you would use a steroid. They use it on an as-needed basis. Like [if it starts] growing, they’ll dab it on for a couple weeks and be like, “yeah, it’s changing in size, so I think it’s cancer.” But for a big ulcer, I haven’t seen anyone using it.
MCKEAN: That’s really interesting, thanks.
KHASAWNEH: I treated over 20 patients with cutaneous cancers with cemiplimab, and 2 of them actually had severe, severe joint pain—one at cycle 2, and one at day 1 of cycle 3. One of them required about 4 mg of hydromorphone to control his pain and one did not want to proceed anymore with immune therapy because of the severity of their pain.
The first patient when this happened, I kind of dodged the bullet and said let’s try to continue with the next cycle, and when this happened again, the patient was adamant about stopping the drug. Have you had such severe arthralgia in your practice?
MCKEAN: Yeah, it’s interesting, I think arthritis can be tricky because it can be hard to pick up on, I guess. I had one older patient with skin cancer that’s off of treatment because of arthritis. So, I’ve definitely seen that, and I wonder if some of your experience with cemiplimab is to some extent [in an] older population. So, interested to hear some others’ thoughts, but when I’ve had patients that have had immune systems kind of light on fire with one dose of immune checkpoint inhibitor, they’ve been older patients, a patient that gets one dose and just has severe toxicity.
KHASAWNEH: I know, but these patients are perfectly fine as far as arthritis pain or joint pain, but 10, 15 minutes into the infusion they had the worst pain. And the same experience with both patients, but after we give them opioids, literally within half an hour they’re back fine, and no recurrence of the pain with those patients. Similar experience with 2 patients.
MCKEAN: Oh, interesting. So, it’s actually during the infusion that you’ve had this?
KHASAWNEH: During the infusion, 10 to 15 minutes, and even the second patient with whom I re-challenged him, similar. Just diffuse pain, he said, through shoulders, to the back, to the hips. And the same thing happened when we tried the infusion again. So, we had to stop it, actually, in 2 patients, just because of the severe pain 10 to 15 minutes into the infusion.
MCKEAN: Interesting. Has anyone else had a patient experience like that?
SHEPARD: I will say, I’ve treated hundreds of patients with PD-1 inhibitors of different flavors for different diseases, and any kind of immediate infusion reaction that’s severe enough to stop treatment is 1%, maybe, or less. I can only think of maybe 1 patient out of probably more than 100.
There are very few patients that’s I’ve actually treated with cemiplimab, probably 3 or 4 total, and they’ve tolerated it fine with no infusion reactions. The inflammatory arthritis, like rheumatoid or autoimmune arthritis that can happen weeks later, I’ve seen a few people with that, but it’s rarely been severe enough to stop treatment.
MCKEAN: Interesting. And I think on the studies, in the label, the infusion reactions are a little bit more common, seem to be anyways, [with] the PD-1 inhibitors.
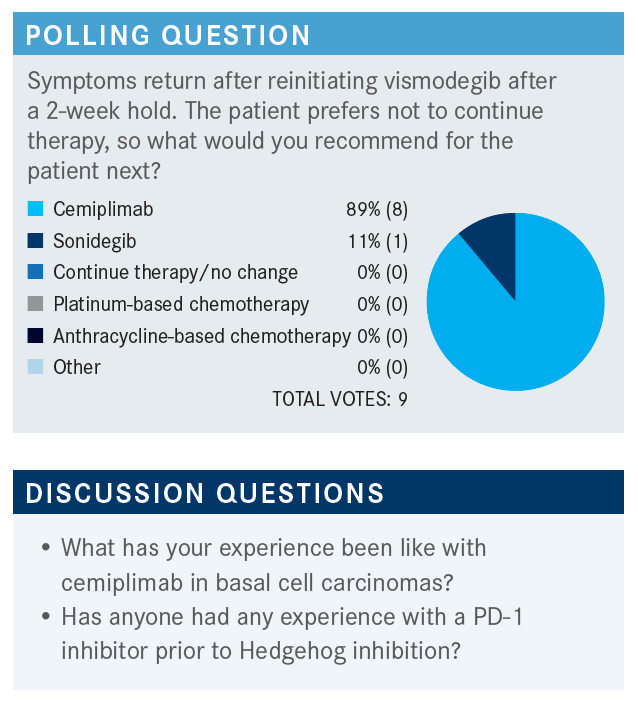
And then, let’s see. What do we know about patients who received a PD-1 inhibitor prior to Hedgehog inhibitor? Do you have any experience with this? I’m guessing it’s a little too early, but maybe there is someone that’s treated a patient with PD-1 first, and then gone to a Hedgehog inhibitor for those patients that didn’t respond. Anyone with experience on that?
SHEPARD: I don’t, but I can’t think of any scientific or mechanism basis that there would be any particular interaction. I almost think the response rates would be the same either way. Am I right about that? Is there some [way that a PD-1] inhibitor [would] down-regulate the hedgehog pathway in some way that you might think it wouldn’t work later on? I don’t know.
MCKEAN: Yeah, I’m not aware of that. Is there something with immune infiltration that would change things? But ultimately, it’s probably the patients that aren’t responding that you’d be using the Hedgehog inhibitor after, but I think we’re going to see a lot more of this. Right? You’re going to want to try immune therapy upfront, and then if they don’t respond, then rescue with a Hedgehog inhibitor later.
WASELENKO: Are there any data, preclinical data, to suggest that Hedgehog inhibitor might increase or decrease PD-L1 expression?
MCKEAN: I imagine there’s going to be more real-world data to come out looking at the Hedgehog inhibitors after PD-1 to see, but would that change peoples’ minds if hedgehog inhibitor responses dropped to 20% afterwards? Would you be more likely to then use a hedgehog inhibitor upfront because the response rates are higher, versus after? I don’t know.
And I guess the other challenge with that is you might be selecting for different disease as well in those patients that have just blown through PD-1. But, great question, and I think a lot more data to be determined there.
REFERENCES
1. NCCN Clinical Practice Guidelines in Oncology. Basal cell skin cancer, v2.2021. Accessed August 5, 2021. https://bit.ly/3xGF8B
2. FDA approves cemiplimab-rwlc for locally advanced and metastatic basal cell carcinoma. FDA. February 9, 2021. Accessed August 5, 2021. https://bit. ly/3wWMhgM