Roundtable Discussion: Krishnan Debates the Rationale For Various Therapies in Multiple Myeloma
During a Targeted Oncology™ Case-Based Roundtable™ event, Amrita Krishnan, MD, discussed with participants their choice of therapy for a patient with multiple myeloma who relapsed after receiving bortezomib, lenalidomide, and dexamethasone followed by autologous stem cell transplant and 2 years of lenalidomide maintenance.
Amrita Krishnan, MD (Moderator)
Director of the Judy and Bernard Briskin Center for Multiple Myeloma Research
City of Hope
Duarte, CA

CASE SUMMARY
A 60-year-old White woman was diagnosed with stage II multiple myeloma. She has a history of being a heavy smoker, with a gain (1q21) of cytogenetics and an ECOG performance score of 0. At the time, she was treated with bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone (VRd) induction therapy, followed by autologous stem cell transplantation. She achieved a complete remission with VRd and transplant and was minimal residual disease negative, then placed on lenalidomide maintenance therapy.
At a follow-up after 2 years on lenalidomide maintenance, the patient reported having severe fatigue and pain in her back and legs, which was disrupting her ability to continue working full time. A PET scan shows vertebral fracture at L1, lesions in both femurs, and an ECOG performance score of 1. Her current lab levels are now the following:
- M protein, 1.98 g/dL (rapid increase from prior bloodwork)
- λ free light chain increased from 47.5 mg/dL to 136.7 mg/dL
- Hemoglobin: 9.8 g/dL
- White blood cell counts and platelets: within normal limits
- Creatinine: 1.4 mg/dL (range, 0.59-1.04 mg/dL)
- eGFR: 45 mL/min/1.73m2
- Creatinine clearance: 40 mL/min
KRISHNAN: We have [a case here] with a biochemical and clinical progression.
Some of the [factors] to talk about are [whether] they are early vs late relapse, and [whether] that influences your decisions in terms of therapy?
CHHABRA: I tend to think patients who receive lenalidomide [Revlimid] maintenance, if they progress less than 36 months, [are considered an] early relapse patient. If they did not receive maintenance, then 18 months [is when I would consider them an early relapse patient]. That’s been my rule of thumb.
Although I’ve also heard that 24 months is a good cutoff between early and late relapse. My preferred second-line regimen is not influenced by early vs late relapse, because I’ve been using daratumumab [Darzalex]-based therapy, typically in combination with carfilzomib [Kyprolis] and dexamethasone [DKd]. If I have a clinical trial that is specifically for patients in the high-risk category, early relapse [is considered] less than 18 months—such as the allogeneic transplant trial, [with patients who] had less than 18 months from transplant.
KRISHNAN: Let’s see [whether] every-one else agrees with you in terms of [the following]: (1) early relapse and (2) it sounds like you’re a big DKd fan. Dr Lashkari, are you on the DKd bandwagon for first relapse?
LASHKARI: I would certainly recognize this as being a more aggressive relapse in a patient. I think you’re right, [that] if this patient were treated initially, we would consider giving a daratumumab-based induction therapy, but she did very well, which is interesting. She had a complete response, and one can argue that if someone became [minimal residual disease] negative, it almost doesn’t matter how you get there if you get there, because that in and of itself tends to portend a good prognosis. Considering someone relapsing within a couple years; invariably, this patient relapsed within 2 years because we see an M spike of 1.98 g.
Biochemical progression would have been defined as having greater than 0.5 g/dL, and that may have developed within a year from time of transplant. I would consider this patient to be an early relapse with aggressive clinical features, but I would certainly rebiopsy them to see what other clones are present.
In terms of treatment options, it’s interesting to get the information to come back. I don’t know [whether] we can guide based on the information that comes back necessarily, unless perhaps they had an 11;14 translocation, in which case you can consider a venetoclax [Venclexta]-based treatment. I probably wouldn’t even consider that for such a patient if they haven’t received a CD38 antibody. DKd is reasonable, and another option would be to go to daratumumab, pomalidomide [Pomalyst], and dexamethasone [DPd] as another option.
KRISHNAN: [Are there] any other takers for DPd instead? It sounds like everyone would agree with daratumumab, but it’s really what the partner would be. Would anyone pick DPd?
CHAND: I tend to use more DPd compared [with] DKd, because in my experience, scheduling and monitoring is a little easier on this regimen. It tends to work well in patients who are refractory to lenalidomide. I just find it more tolerable. The cytopenias are a little bit less compared [with] the DKd, too.
AMBIKA: I tend to use more DPd, too—for the same reasons as [others mentioned]—and use carfilzomib, cyclophosphamide, and dexamethasone [KCd] as the next-line [treatment], like carfilzomib plus cyclophosphamide. I went through that route in a few patients and they did OK.
DEKKER: I typically use carfilzomib. [Patients] come to [the] infusion center already, so they will get carfilzomib as well. Plus, carfilzomib is a potentially more powerful agent, and I use it once a week. If [patients] develop cardiac toxicities [within the first 2 or 3 weeks], I back off. If they don’t, they typically would do well and tolerate it for a long time.
CHAUDHARY: Myelosuppression is less with DPd, in my experience, if you dose reduce the pomalidomide.
KRISHNAN: It sounds like we’re pretty much split [between] DPd and DKd, both being valid regimens in that early 1- to 3-[year] relapse setting. What I’m hearing from people is to pick your adverse events [AEs], as well, and I’m guessing [that] if someone had prior cardiac history, more clinicians would [choose to use] DPd. But let me ask a more challenging question. I’ve not heard a single person say IPd [isatuximab-irfc (Sarclisa), pomalidomide, dexamethasone] or IKd [isatuximab, carfilzomib, dexamethasone]. Is anyone using isatuximab?
MURAD: That’s our preferred drug, but that’s definitely a reasonable option. I don’t think there’s any problem with carfilzomib.
DEKKER: I use daratumumab and isatuximab. Clearly, subcutaneous administration is a plus, but I had a few patients who had a cutaneous reaction or had skin conditions, so I decided to go with isatuximab.
KRISHNAN: Do most [of you] feel they’re comparable, or do [you] feel that there’s a difference?
DEKKER: I think they’re probably comparable. I do think [that] sometimes later products may have some advantages, because they know the issues with the original product and tried to tweak the molecule a little bit. So theoretically, I would say isatuximab may be a bit better, but the problem is daratumumab is good enough on its own, so I’m doubtful we will find much of the difference. We could keep analyzing the data and find a subtype, a subgroup here or there, or a special population that will be beneficial. But for both [medications, it is] likely all the data will come down to the same ballpark.
KRISHNAN: I’m just curious, Dr Dekker, when you say you think isatuximab is better, is it in terms of [AEs] or efficacy?
DEKKER: Both, because again, they look at the molecule, they see off-target effects, and they see where the escape mechanisms are. So when they manufacture the molecule, all this minor tweaking in the design may help to both improve efficacy and decrease toxicity. But how clinically significant that is, how truly that will translate into something meaningful in clinical practice without head-to-head data—that will be impossible to determine.
KRISHNAN: So if I could summarize, most [of you] are convinced [of using] CD38 antibody without, and finding them interchangeable depending on their practice and some specific patient issues. Then it’s really the partner to that antibody, right?
MUKHERJEE: Yeah, I’m comfortable with using daratumumab now and usually do introduce that in the second line. Depending on the other comorbidities of the patient, if they have cardiac issues, then I would go with pomalidomide. If not, then carfilzomib. I’m comfortable with daratumumab, but I’m not that comfortable with isatuximab yet.
KRISHNAN: That’s interesting. I will give you a look to the future. There’s a phase 3 trial ongoing, [comparing] DPd[with] teclistamab-cqyv [Tecvayli], pomalidomide, and dexamethasone, so that will be interesting—the T-cell engager, the new drug that just got approved, then being moved into that early relapse setting. I think many of you are familiar with the CARTITUDE-1 trial [NCT03548207], also in the earlier relapse setting.1
What will be interesting [is that in 2024 or 2025], myeloma may look completely different. We [may] see T-cell engaging therapy moved up earlier, in part because the CD38 antibodies are [also] going to be moved up even earlier, in terms of their use in induction therapy. I think that is the challenge in myeloma.
DISCUSSION QUESTION
- What can you tell us about the progression-free survival [PFS] data for phase 3 triplet regimens for lenalidomide-refractory, relapsed-refractory multiple myeloma?
KRISHNAN: I think the [PFS data for these regimens are] what people responded to, [those] who wanted to use carfilzomib as the partner to CD38. In the IKEMA trial [NCT03275285], which compared IKd vs Kd [carfilzomib and dexamethasone], the PFS is decent and you’re getting almost 3.5 years out of a first relapse regimen [From the Data2].
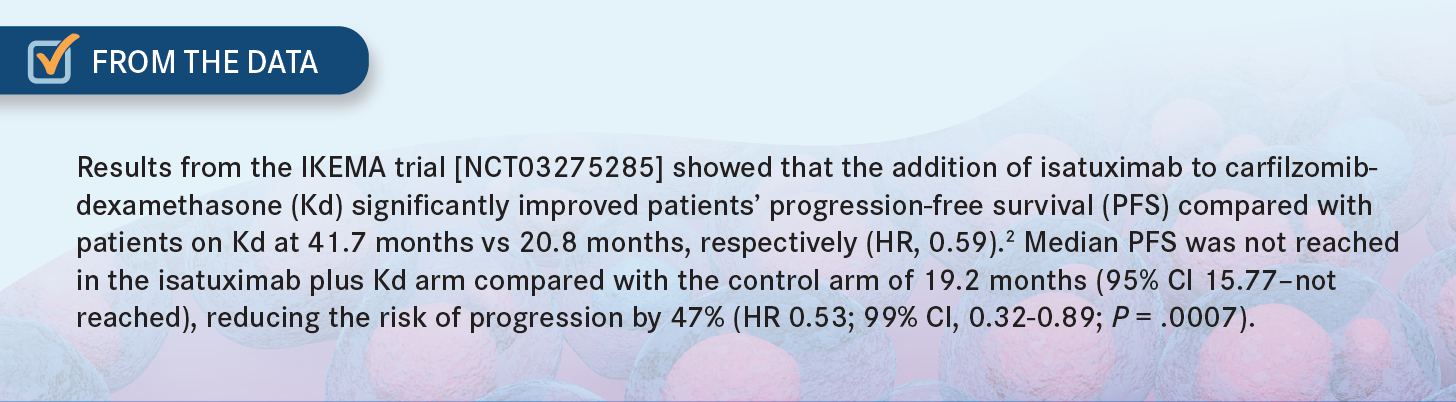
In the CANDOR trial [NCT03158688], [the PFS is approximately] 2.5 years, [comparing DKd vs Kd].3 And then [the PFS] goes down from there in the CASTOR [NCT02136134], ICARIA-MM [NCT02990338], APOLLO [NCT03180736], and OPTIMISMM trials [NCT01734928].4-7 Interestingly—and I use a lot of DPd—if you compare the PFS, it’s not as great at [approximately 1] year based on the APOLLO study, and IPd is the same at [approximately 1] year.5,6
DISCUSSION QUESTION
- What else influences your decision in determining what you choose as therapy in a patient similar to the one in our case?
KRISHNAN: This patient did have some mild renal impairment, [as well as] the genetic risk with the [1q21 gain]. It sounds like that would push you a little bit more, as well.
LASHKARI: The 1 issue I think a lot of us have who see these patients with myeloma is that carfilzomib is a great drug, but it’s not without some of its own AEs in terms of cytopenias, fluid retention, and sometimes infusion reactions. And for the [patients who] are just in your office all the time, I feel for them. That’s another potential barrier, especially if you’re dealing with patients who may not be as robust as others.
That is a big factor that plays into my thinking for maybe not using carfilzomib at this time. Maybe I should be changing my mind if the data—as we saw with the 2 trials evaluating carfilzomib with daratumumab or isatuximab—are truly what you get out of it. Maybe that is a better option, but it may be a slightly harder sell for patients, especially those [who] value their quality of life and the amount of time that they’re not spending at your office.
KRISHNAN: I do think it’s a potent regimen. I tend to use it in younger patients, because I do think, in the CANDOR study, [most] of the deaths were in patients [older than] 65 [years], and more infectious death.3 In older patients, I tend to be a little more cautious about using it, and I only do it in older patients when my back is against the wall and they have really aggressive disease.
Otherwise, I do use it in younger patients with aggressive disease. In other younger patients, I try to, but to your point, a lot of younger patients tend to still be working, and coming into the office even once a week can be challenging. So lifestyle and patient preference also play an important role.
REFERENCES
1. Martin T, Usmani SZ, Berdeja JG, et al. Ciltacabtagene autoleucel, an anti-B-cell maturation antigen chimeric antigen receptor T-cell therapy, for relapsed/refractory multiple myeloma: CARTITUDE-1 2-year follow-up. J Clin Oncol. 2022;JCO2200842. doi:10.1200/JCO.22.00842
2. Moreau P, Dimopoulos MA, Mikhael J, et al. Isatuximab, carfilzomib, and dexamethasone in relapsed multiple myeloma (IKEMA): a multicentre, open-label, randomised phase 3 trial. Lancet. 2021;397(10292):2361-2371. doi:10.1016/S0140-6736(21)00592-4
3. Usmani SZ, Quach H, Mateos MV, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): updated outcomes from a randomised, multicentre, open-label, phase 3 study. Lancet Oncol. 2022;23(1):65-76. doi:10.1016/S1470-2045(21)00579-9
4. Spencer A, Lentzsch S, Weisel K, et al. Daratumumab plus bortezomib and dexamethasone versus bortezomib and dexamethasone in relapsed or refractory multiple myeloma: updated analysis of CASTOR. Haematologica. 2018;103(12):2079-2087. doi:10.3324/haematol.2018.194118
5. Richardson PG, Perrot A, San-Miguel J, et al. Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM): follow-up analysis of a randomised, phase 3 study. Lancet Oncol. 2022;23(3):416-427. doi:10.1016/S1470-2045(22)00019-5
6. Dimopoulos MA, Terpos E, Boccadoro M, et al. Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(6):801-812. doi:10.1016/S1470-2045(21)00128-5
7. Richardson PG, Oriol A, Beksac M, et al. Pomalidomide, bortezomib, and dexamethasone for patients with relapsed or refractory multiple myeloma previously treated with lenalidomide (OPTIMISMM): a randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(6):781-794. doi:10.1016/S1470-2045(19)30152-4