Reviewing PD-L1 Status and Immunotherapy Combinations in NSCLC
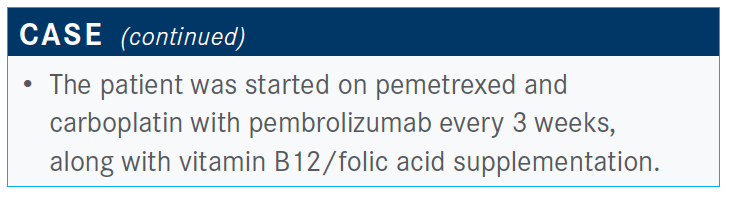
During a Targeted Oncology Case-Based Peer Perspectives event, Deepa Rangachari, MD, reviewed the case of a 59-year-old Caucasian man with non–small cell lung cancer who expressed PD-L1.
Deepa Rangachari, MD

During a Targeted Oncology Case-Based Peer Perspectives event, Deepa Rangachari, MD, Harvard Medical Faculty Physician, Beth Israel Deaconess Medical Center, Boston, MA, reviewed the case of a 59-year-old Caucasian man with non–small cell lung cancer (NSCLC) who expressed PD-L1 and the treatment approach for this patient.
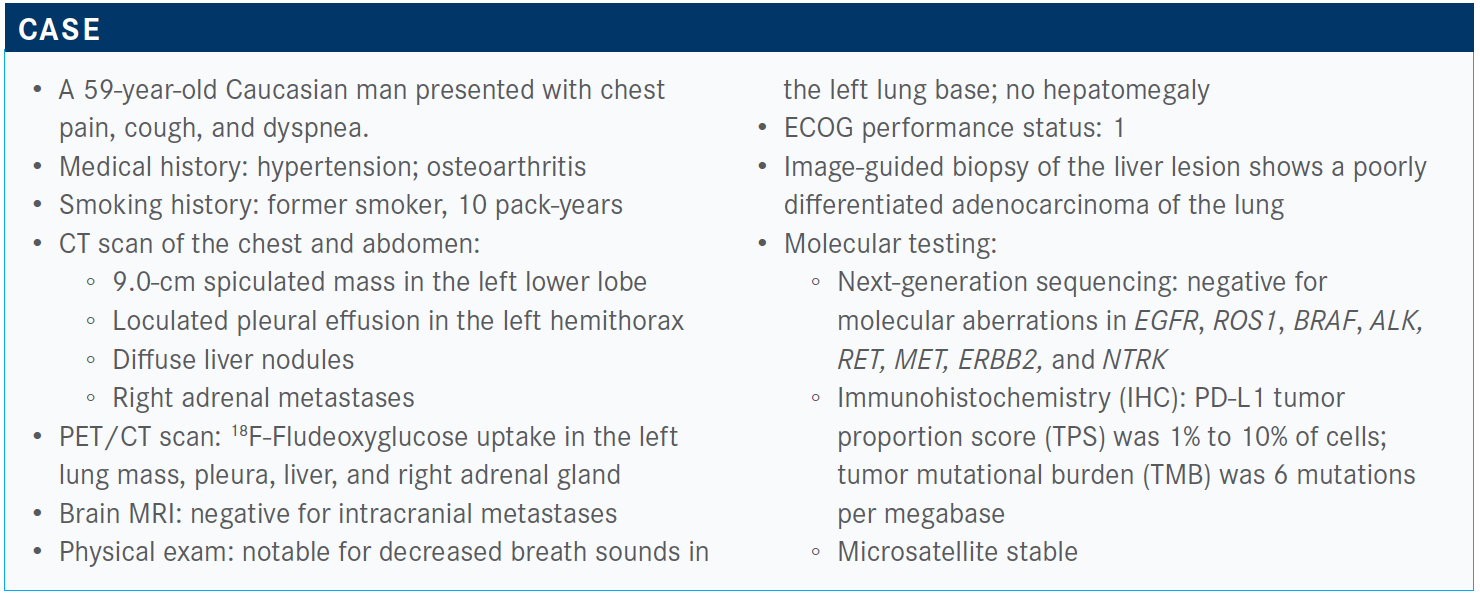
Targeted Oncology™: Which clinical trial results that led to approvals in the frontline setting would you apply to a patient such as this?
RANGACHARI: The KEYNOTE-189 trial [NCT02578680] is the one that explored either carboplatin or cisplatin [plus pemetrexed] versus pembrolizumab [Keytruda], carboplatin or cisplatin, and pemetrexed. This trial was in patients with nonsquamous NSCLC, because of the use of pemetrexed.1
No actionable alterations were allowed and PD-L1 status was not required for entry. Patients were stratified according to tumor PD-L1 expression. Patients weren’t allowed study entry if they had untreated brain metastases, and they had to have no active autoimmune disease requiring systemic steroids, [based on] standard exclusion/inclusion criteria.1 The updated overall survival [OS] follow-up from KEYNOTE-189 was presented earlier this year, showing a median OS of 22 months in the pembrolizumab combination arm [95% CI, 19.5-25.2], effectively the longest OS published thus far for these frontline strategies, vs 10.7 months [95% CI, 8.7-13.6] for patients receiving chemotherapy alone.2
The OS curves separated early on and there was notable durability of the survival outcome, with close to 50% of patients on pembrolizumab alive at [18 months] versus just under a third of patients on chemotherapy alive. PD-L1 is our one vetted immune biomarker, although there has been an incredible amount of activity and interest in other immune biomarkers to help predict benefit, including TMB, [and] presence or absence of other nonactionable commutations like STK11 and KEAP1 KRAS expression.
But for now, we’re hanging our hats mostly on PD-L1. Regardless of tumor PD-L1 expression, the combination of chemotherapy plus immunotherapy showed favorable OS as compared with chemotherapy alone. The magnitude of benefit was comparable across all subgroups, although certainly very high, even in patients absent tumor PD-L1.
About one-third of patients who have tumors lack PD-L1 expression. About a third of patients will fall into the category of low to intermediate expression, and about a third of patients will have high tumor PD-L1 expression. Roughly two-thirds of patients have either no tumor PD-L1 expression or low PD-L1 expression, for which the treatment options are a bit more complicated.
For this patient, multiple combination therapy strategies are viable, including chemotherapy and immunotherapy, chemoimmunotherapy with bevacizumab [Avastin], or just immunotherapy alone.
The KEYNOTE-042 trial [NCT02220894] looked at pembrolizumab versus chemotherapy in patients with PD-L1 TPS greater than or equal to 1%. Patients with TPS 50% or more and patients with TPS of 1% to 49% were stratified according to expression. In the overall study population, there was improvement in OS in patients treated with pembrolizumab whose tumors had any degree of PD-L1 expression [PD-L1 ≥ 1%, median OS 16.7 months (95% CI, 13.9-19.7); PD-L1 > 20%, median OS 17.7 months (95% CI, 15.3-22.1); PD-L1 > 50%, median OS 20 months (95% CI, 15.4-24.9)].3,4
It’s the subgroup analysis that has given a lot of people pause about using this strategy. If you look at which group of patients drove the survival benefit, it’s the patients on pembrolizumab with high tumor PD-L1, greater than or equal to 50%, who had the most dramatic OS benefit [vs median OS of 12.2 months in patients with high tumor PD-L1 on chemotherapy alone (95% CI, 10.4-14.2)] as opposed to patients with the intermediate levels of tumor PD-L1 expression [pembrolizumab, median OS 13.4 months (95% CI, 10.7-18.2) vs chemotherapy, median OS 12.1 months (95% CI, 11.0-14.0)], raising the question [whether] patients with 1% to 49% expression [are] truly benefiting.
The flipside is that the patients with TPS 1% to 49% who got immunotherapy alone rather than chemotherapy didn’t do worse, although this was not designed as a noninferiority trial. You could extrapolate that pembrolizumab is not worse than chemotherapy, although, again, the trial wasn’t designed to answer that question. You can use pembrolizumab as a single agent in [patients with a low to intermediate PD-L1 TPS], particularly in someone for whom you have clinical concerns about intensifying therapy by adding chemotherapy or other agents, …recognizing that the patients who derived the most benefit and drove most of the survival advantage in KEYNOTE-042 were the patients with high tumor PD-L1.
In patients with high tumor PD-L1, pembrolizumab by itself was highly effective in the KEYNOTE-024 trial [NCT02142738].5
How do you decide in which patients with low PD-L1 TPS you can initiate checkpoint inhibitor therapy?
Recently, with the implications of COVID-19 and not wanting to [cause heavy myelosuppression in] patients, I’ve treated patients with low PD-L1 TPS more frequently [than I did before COVID-19 with checkpoint inhibitors]. The only caveat in my mind is, if a patient is truly not well enough to be treated, I don’t think they should be treated with immunotherapy, even as a single agent. There are emerging data suggesting that patients with poor performance status who were treated with single-agent checkpoint inhibitors don’t necessarily derive benefit.
If they’re on the cusp, where I feel they could be treated but I don’t feel I can give intensive therapy, I think [a] single agent is a viable option.
What do recent trial data tell us about treating patients with low to intermediate PD-L1 TPS with checkpoint inhibitors?
In KEYNOTE-042, for patients in the low to intermediate range, 1% to 49%, the OS curves for pembrolizumab and chemotherapy crossed.3,4
One thing to keep in mind when we look at these landmark immunotherapy trials [is that] the comparator arm is platinumdoublet chemotherapy by itself, which in 2020 is effectively a historically defunct option. Unless someone has clear contraindications to immunotherapy, we really should not be giving platinum doublet alone to these patients who do not have actionable targets.
IMpower150 [NCT02366143] was a complicated trial with multiple arms that explored the combination of platinum doublet [carboplatin and paclitaxel] with immunotherapy of atezolizumab [Tecentriq] and bevacizumab, so triplet therapy, so to speak. There were 2 other arms in this trial, platinum-doublet chemotherapy with bevacizumab alone and platinum-doublet chemotherapy with atezolizumab alone.6
There was no minimum requirement for tumor PD-L1 expression. The data that have been presented thus far were for 2 subgroups from the intent-to-treat wild-type (WT) population, atezolizumab, bevacizumab, and chemotherapy [arm B] versus bevacizumab and chemotherapy [arm C]. We don’t have the comparison of atezolizumab and chemotherapy [arm A] versus arm B, so we don’t know whether atezolizumab, bevacizumab, and chemotherapy is better than atezolizumab and chemotherapy, which is an important question. Atezolizumab, bevacizumab, and chemotherapy was better than bevacizumab and chemotherapy in this study, regardless of tumor PD-L1 status [arm B, median OS 19.2 months (95% CI, 17.0-23.8) vs arm C, median OS 14.7 months (95% CI, 13.3.-16.9)].6,7
There was particular benefit in WT patients with liver metastases [arm B, median OS 13.2 months vs arm C, median OS 9.1 months (HR, 0.54)] and patients with EGFR or ALK alterations who had exhausted [other] available targeted therapies [arm B, median OS not evaluable vs arm C, median OS 17.5 months (HR, 0.54)].6 …I think there are specific patients in whom the addition of bevacizumab to platinum doublet and immunotherapy makes sense…but I am not sure it makes sense for everybody.
The more drugs you add, the greater incidence of treatment- related toxicity and greater incidence of treatment discontinuation due to toxicity. So there are some answers and some questions raised by this trial.
The bevacizumab plus chemotherapy arm is not the standard of care anymore. Knowing that atezolizumab, chemotherapy, and bevacizumab is better than bevacizumab plus chemotherapy is fine,6,7 but what you really want to know is [whether] atezolizumab, chemotherapy, and bevacizumab [is] better than atezolizumab and chemotherapy or pembrolizumab and chemotherapy. We don’t know.
Based on the subgroup analyses and improved outcomes shown in the WT population with liver metastases and in patients with tumor EGFR or ALK mutations who had exhausted targeted therapies, I would consider atezolizumab, chemotherapy, and bevacizumab in those 2 types of patients—especially in patients with EGFR- or ALK-positive tumors in whom immunotherapy, and even immunotherapy combinations, have shown disappointing results.
What other immunotherapy combinations have shown efficacy in this patient population?
The combination nivolumab [Opdivo] plus ipilimumab [Yervoy] vs nivolumab monotherapy vs chemotherapy strategy in CheckMate 227 [NCT02477826]. This trial is a complicated schema. If you drill down, it’s looking at 2 cohorts of patients: patients with PD-L1 greater than or equal to 1% and patients with absent tumor PD-L1. In particular, the primary outcome or end point that was being assessed in this trial was OS in the PD-L1 greater than or equal to 1% cohort.8,9
In the patients with PD-L1 greater than or equal to 1%, [the comparison of] OS was for patients receiving nivolumab plus ipilimumab versus patients receiving chemotherapy alone, which, in theory, is the option we should be thinking about in 2020.8,9
There was a clear demonstration of survival benefit [at 3 years] with nivolumab and ipilimumab in these patients with PD-L1 greater than or equal to 1%, with an HR of 0.79 [95% CI, 0.67- 0.93].10 Even in the patients with PD-L1 less than 1%, there was a survival benefit associated with nivolumab and ipilimumab, but it wasn’t the primary planned outcome of the trial.9 Interesting, but not necessarily actionable.
On the basis of these data in patients with PD-L1 greater than or equal to 1%, nivolumab and ipilimumab is now an FDA-approved option, meaning no chemotherapy at all.11 This strategy is not FDA approved in small cell lung cancer but has been studied in it.
The magnitude of OS benefit appears to be greatest in patients with high tumor PD-L1.9 That’s helpful, but is that necessarily better than a single-agent immune checkpoint inhibitor regimen? The answer is, we don’t know, but some benefits were seen in patients with any degree of tumor PD-L1. The addition of ipilimumab does lead to an increased number of treatment-related AEs, with drug discontinuation rates as high as almost 20% in the nivolumab and ipilimumab arm versus 9% in the chemotherapy alone arm.
It’s the predicted immune-related toxicities, including colitis, hepatitis, etc, that are seen at a greater rate when you combine 2 immune checkpoint inhibitors as opposed to giving 1 of them alone, so this is something important to consider. There’s a general sense that immune therapy must be more tolerable than chemotherapy or chemoimmunotherapy, but the answer is, not necessarily. Ipilimumab, with high-grade diarrhea or organ toxicity, could be problematic for some of our patients.
Skin toxicity is one of the most common treatment-related AEs, especially early on, with other toxicities including GI [gastrointestinal] toxicities and endocrinopathies occurring later in the disease course.10 Any immune-related toxicity can occur at any point in the treatment course, [though].
The FDA approval that came out right before ASCO [American Society of Clinical Oncology meeting] in late May [2020] was CheckMate 9LA [NCT03215706].12 This was nivolumab, ipilimumab, and a limited number of chemotherapy cycles: 2 cycles of platinum doublet, with nivolumab and ipilimumab, versus 4 cycles of platinum doublet, with the option of pemetrexed maintenance if the patient had adenocarcinoma. This trial was for all-comers, regardless of tumor PD-L1 status.13
The preliminary survival data presented at ASCO this year showed that the combination of nivolumab, ipilimumab, and a limited number of cycles of chemotherapy had an improved OS advantage as opposed to chemotherapy alone, with an HR of 0.66 [95% CI, 0.55-0.80]. When we use immunotherapy in the frontline setting, the survival tends to be more durable, with more than half of all patients in this study alive and well at 12 months as opposed to just under half of patients alive and well at 12 months after they received chemotherapy alone.
In the subgroup analyses stratified by tumor PD-L1 status, all subgroups, regardless of tumor PD-L1 expression, benefitted from this approach; there was a uniform magnitude of about a 40% reduction in the risk of death, with HRs all right around 0.60.
There were no major surprises [with respect to progressionfree survival (PFS)], and no major surprises in that you can increase the response rate by combining chemotherapy with something else [PFS, 33% at 12 months], as opposed to chemotherapy alone [PFS, 18% at 12 months], where we know the response rate historically sits right around 20% to 25%, and that’s exactly what was seen in this clinical trial.
If you think about the objective response rate [ORR] seen in the KEYNOTE-189 trial, with combination chemotherapy and pembrolizumab, the rate was close to 50%.1 The more drugs you add, the higher the response rate and, in general, some benefit in survival. However, the more you add, the more adverse effects you’re likely to see. [In CheckMate 9LA], there was a reasonably high rate of skin-related toxicities, mostly grade 1/2; also, endocrinopathy was fairly common, as well as GI toxicities, particularly colitis, and hepatitis was also notable.13
Much of this increase in toxicity is driven by the combination of ipilimumab and nivolumab as compared to giving the PD-1 or PD-L1 agent alone…. This regimen is now approved for patients with previously untreated NSCLC, regardless of tumor PD-L1 expression.14
Does addition of chemotherapy to combination checkpoint inhibitor therapy correlate with decreased immune-related AEs?
From the rates that are reported, we can’t really say that. The number of cycles of platinum-doublet chemotherapy exposure was limited, only 2 cycles, so it’s not clear that combining the chemotherapy with nivolumab and ipilimumab mitigated the risk of immune-related AEs.13
Regimens looking at ipilimumab 3 mg/kg and nivolumab 1 mg/kg have been toxic in both small cell lung cancer and NSCLC, and generally haven’t advanced through later lines of investigation.
Atezolizumab was recently approved on the basis of the IMpower110 trial [NCT02409342] as a single agent for patients with high tumor PD-L1 expression.15 In this trial, for atezolizumab, high PD-L1 was defined as greater than or equal to 50% of tumor cells or greater than or equal to 10% of immune infiltrating cells. [This trial used the Ventana PD-L1] SP142 assay as opposed to the [PD-L1 IHC] 22C3 [pharmDx] assay, which is most commonly used to assess PD-L1 when using pembrolizumab. So this is yet another option for single-agent immune checkpoint inhibitor in high PD-L1–expressing patients.
For patients with liver metastasis or patients unwilling or not well enough for chemotherapy, what treatment option would you choose?
In a liver metastasis example or a situation in which a patient is either unwilling or not quite well enough to have chemotherapy, I might consider the chemotherapy-sparing option, but there are no easy answers.
My personal preference is to use pembrolizumab alone only in high [PD-L1] expressers unless there’s a good reason why I can’t give [immunotherapy]. The patient who’s well enough for treatment but not well enough for combination therapy has comorbidities, where giving platinum doublet might be tricky. During COVID-19, I’ve [limited platinum-doublet therapy] out of a desire to minimize the myelotoxicity that would come from giving the platinum.
[For patients who refuse chemotherapy], I would have an honest conversation [and tell them] that the nivolumab and ipilimumab combination is not necessarily the tolerable combination. Then I would be thinking about single-agent immunotherapy.
A lot of people have the idea [that chemotherapy is always worse,] and it behooves us to have honest conversations about the fact that even immunotherapy-based strategies can have their own issues.
It’s frustrating not to have better biomarkers, and that’s an active area of ongoing research for the more than 60% of patients who don’t have the option of actionable target. What is the best strategy? Who needs combinations? Which combination should we use? These are important questions, as they pertain not only to survival but to clinical and financial toxicity. These drugs cost a lot, and people can do very well for a long time. So we owe it to them to figure out how to use these drugs wisely.
What would you use for a maintenance therapy in this setting?
Pembrolizumab maintenance without pemetrexed; I think that’s a viable strategy. I imagine it’s because of concerns about continued long-term use of pemetrexed, and fatigue and peripheral edema tend to be the 2 biggest adverse effects that people have with long-term use, and some cytopenias. What was studied in KEYNOTE-189 that gave the best survival outcome was pembrolizumab and pemetrexed maintenance rather than singleagent maintenance.1
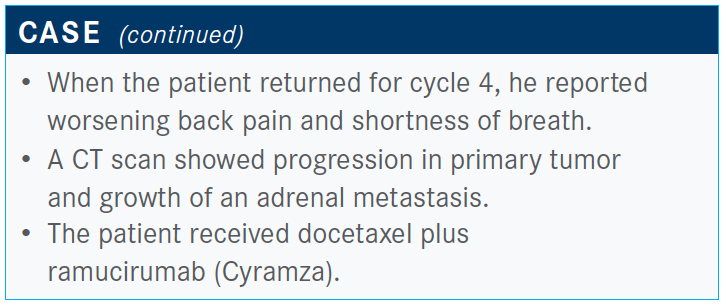
Please explain the data behind docetaxel and ramucirumab as a second-line therapy option.
The evidence behind docetaxel and ramucirumab is data from the REVEL trial [NCT01168973], which looked at this combination in the second line versus docetaxel alone.16
We don’t use antiangiogenic agents such as bevacizumab in patients with squamous histology tumors in the first-line setting because there was a high [rate] of hemorrhagic life-threatening events in the initial trials of platinum with bevacizumab in the squamous group in this trial in the second-line setting. [In spite of this], patients with squamous or nonsquamous tumors were permitted entry as long as there wasn’t major blood vessel involvement from a central tumor––and no intratumoral cavitation, which increases the hemorrhagic risk––as long as they’d had no thromboembolic events within 6 months of treatment initiation, and as long as there was no gross hemoptysis or active GI bleeding.16
Any patient in the second-line setting could get docetaxel and ramucirumab versus docetaxel alone. There was a small but present OS benefit in patients on docetaxel and ramucirumab of 10.5 months versus 9 months for patients on docetaxel alone, with an HR of 0.86 [95% CI, 0.75-0.98] and some incremental increase in ORR, 23% when you add ramucirumab to docetaxel versus docetaxel alone, 14% [odds ratio, 1.89 (95% CI, 1.41-2.54)].
In the preplanned subgroup analysis in patients with aggressive disease…aggressive disease was defined as disease progressing within 9 months of treatment initiation, first-line treatment initiation, or refractory disease, with a best response of PD [progressive disease] with firstline platinum-doublet therapy. In this group of patients with refractory or hyperprogressive disease, there was a significant improvement in OS, approaching 9 months in patients who received ramucirumab in addition to docetaxel [for up to 8 weeks] as opposed to docetaxel alone [6.9 months; HR, 0.83 (95% CI, 0.61-1.15)].17
One of the challenges with this subgroup analysis is that there are a lot of different definitions of refractory or hyperprogressive disease that one might use. The pragmatic definition, which is the one they use, is you give patients frontline platinum doublet and the first scan you get, there’s PD already or short-interval progression within a few months of platinum initiation. There is a signal here that, in this particular subgroup of patients, there may be significant added benefit from adding an antiangiogenic to the taxane rather than taxane alone, which is effectively what was happening with this patient.
He received 4 cycles of platinum doublet and is already having symptomatic progression. It’s a reasonable choice in patients who don’t have eligibility issues with use of antiangiogenics; they didn’t restrict use of antiangiogenics in older patients in the REVEL trial.16 But there is concern about giving it to people older than 65 or 70 years of age. Those older patients were represented in small numbers in that trial. The other things they looked at were quality of life and toxicity outcomes.
Patients who got docetaxel plus ramucirumab didn’t appear to have worsening of quality-of-life parameters or unexpected increases in toxicity beyond what might be predicted with ramucirumab. AE-related treatment discontinuation was 15% for patients on docetaxel and ramucirumab versus 9% for docetaxel alone. About a third of patients required some sort of dose adjustment, but as it related to the docetaxel and ramucirumab arm, most dose adjustments were due to proteinuria. Treatment-related deaths occurred in equal proportion in both arms.16
References
1. Gandhi L, Rodr.guez‑Abreu D, Gadgeel S, et al; KEYNOTE-189 Investigators. Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med. 2018;378(22):2078-2092. doi:10.1056/NEJMoa1801005
2. Gadgeel S, Rodr.guez‑Abreu D, Speranza G, et al. Updated analysis from KEYNOTE- 189: pembrolizumab or placebo plus pemetrexed and platinum for previously untreated metastatic nonsquamous non–small-cell lung cancer. J Clin Oncol. 2020;38(14):1505- 1517. doi:10.1200/JCO.19.03136
3. Lopes G, Wu Y-L, Kudaba I, et al. Pembrolizumab (pembro) vs platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 1: open-label, phase 3 KEYNOTE-042 study. J Clin Oncol. 2018;36(suppl 18). doi:10.1200/JCO.2018.36.18_suppl.LBA4
4. Mok TSK, Wu YL, Kudaba I, et al; KEYNOTE-042 Investigators. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819-1830. doi:10.1016/S0140-6736(18)32409-7
5. Reck M, Rodr.guez‑Abreu D, Robinson AG, et al; KEYNOTE-024 Investigators. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N Engl J Med. 2016;375(19):1823-1833. doi:10.1056/NEJMoa1606774
6. Socinski MA, Jotte R, Cappuzzo F, et al. Overall survival (OS) analysis of IMpower150, a randomized Ph 3 study of atezolizumab (atezo) + chemotherapy (chemo) Å} bevacizumab (bev) vs chemo + bev in 1L nonsquamous (NSQ) NSCLC. J Clin Oncol. 2018;36(suppl 15):9002. doi:10.1200/JCO.2018.36.15_suppl.9002
7. Socinski MA, Jotte RM, Cappuzzo F, et al; IMpower150 Study Group. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288-2301. doi:10.1056/NEJMoa1716948
8. Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093-2104. doi:10.1056/NEJMoa1801946
9. Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non–small-cell lung cancer. N Engl J Med. 2019;381(21):2020-2031. doi:10.1056/NEJMoa1910231
10. Ramalingam SS, Ciuleanu TE, Pluzanski A, et al. Nivolumab + ipilimumab versus platinum-doublet chemotherapy as first-line treatment for advanced nonsmall cell lung cancer: three-year update from CheckMate 227 part 1. J Clin Oncol. 2020;38(suppl 15):9500. doi:10.1200/JCO.2020.38.15_suppl.9500
11. FDA approves nivolumab plus ipilimumab for first-line mNSCLC (PD-L1 tumor expression ≥ 1%). FDA. May 15, 2020. Accessed October 30, 2020. https://bit.ly/31YiRSR
12. FDA approves nivolumab plus ipilimumab and chemotherapy for first-line treatment of metastatic NSCLC. FDA. Updated May 27, 2020. Accessed October 30, 2020. https://bit.ly/34GP8zR
13. Reck M, Ciuleanu TE, Dols MC, et al. Nivolumab (NIVO) + ipilimumab (IPI) + 2 cycles of platinum-doublet chemotherapy (chemo) vs 4 cycles chemo as first-line (1L) treatment (tx) for stage IV/recurrent non-small cell lung cancer (NSCLC): CheckMate 9LA. J Clin Oncol. 2020;38(suppl 15):9501. doi:10.1200/JCO.2020.38.15_suppl.9501
14. FDA approves nivolumab plus ipilimumab and chemotherapy for first-line treatment of metastatic NSCLC. FDA. Updated May 27, 2020. Accessed October 20, 2020. https://bit.ly/2HRoGut
15. FDA approves atezolizumab for first-line treatment of metastatic NSCLC with high PD-L1 expression. FDA. May 18, 2020. Accessed October 20, 2020. https://bit.ly/2HNJx1U
16. Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, doubleblind, randomised phase 3 trial. Lancet. 2014;384(9944):665-673. doi:10.1016/S0140-6736(14)60845-X
17. Reck M, Paz-Ares L, Bidoli P, et al. Outcomes in patients with aggressive or refractory disease from REVEL: a randomized phase III study of docetaxel with ramucirumab or placebo for second-line treatment of stage IV non-small-cell lung cancer. Lung Cancer. 2017;112:181-187. doi:10.1016/j.lungcan.2017.07.038

Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More