Redefining Multiple Myeloma Diagnosis and Management
This article reviews some of the concepts surrounding the diagnosis of multiple myeloma are still evolving, and are thus shaping how we see and manage multiple myeloma - hopefully moving slowly but surely toward its elusive cure.
Abstract
Our understanding of multiple myeloma including its pathophysiology, clinical behavior, and management, has improved immensely over recent years. This has translated into development of a more diverse portfolio of therapeutic agents and significantly improved patient outcomes, with the survival among standard-risk patients being in the vicinity of 10 years or more. This also has led to redefining some of the basic concepts surrounding this diagnosis, including the very definition ofmultiple myeloma, response criteria, risk stratification, and goals of treatment. This article reviews some of these concepts that are still evolving, and are thus shaping how we see and manage multiple myeloma - hopefully moving slowly but surely toward its elusive cure.
It is frequently mentioned that the outcomes of patients with multiple myeloma are ever improving, mostly due to the advent of "novel therapeutic agents." It is notable that less than 15 years ago, the diagnosis of multiple myeloma carried a dismal prognosis with no drugs specifically approved by the US Food and Drug Administration (FDA) for its treatment. Since then, not just the therapeutic agents, many of which don't seem "novel" anymore, but our understanding of various other aspects of this disease including its pathophysiology and diagnostic and prognostic techniques have evolved immensely. The goal of this review is to highlight some of these landmark changes that have modified the way we see multiple myeloma and discuss others that are still evolving and that will surely impact the future of patients with this disease, which is so far considered incurable by most.
Redefining Multiple Myeloma
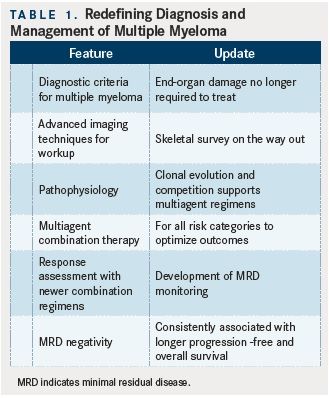
(TABLE 1)
While, historically, the definition ofactive multiple myelomarequired treatment to be initiated at the first sign of end-organ damage (per the CRAB criteria),1it meant that the majority of the patients would not receive treatment to prevent this damage from setting in. This may have been acceptable when the therapeutic options were limited and there was no apparent benefit from early intervention, but in an era when 5-year survival from myeloma is quoted at approximately 50%,2and some patients are living with this disease for 10 years or longer, the need to prevent end-organ damage rather than merely treating it has become imperative in ensuring improved survivorship and better tolerability to subsequent therapies.
Considering this, the International Myeloma Working Group (IMWG) has recently updated its definition ofactive multiple myelomaby adding cases that do not meet the classic CRAB criteria, but that have clonal bone marrow plasma cell percentage ≥60%, involved:uninvolved serum free light-chain ratio ≥100 with the involved serum free light-chain ≥10 mg/dL, or more than 1 focal lesion on magnetic resonance imaging (MRI) studies.3Furthermore, the widespread utilization and availability of serum and urine free light-chain analyses has decreased the number of truly nonsecretory cases of multiple myeloma, providing measurable markers of disease assessment and response in a larger number of patients. It is also accepted that patients with a biopsy- proven bony or extramedullary plasmacytoma and meeting any of the CRAB criteria even without ≥10% clonal bone marrow plasma cells are treated as active myeloma.3While all of this certainly will increase the prevalence of active multiple myeloma, it also will affect clinical trial eligibility and outcomes by introducing a subgroup of patients to treatment before the morbidity from the diagnosis affects them.
Understanding Multiple Myeloma Pathophysiology
Our understanding of the pathophysiology of multiple myeloma has gone beyond the traditional view of it as a malignant monoclonal plasma cell disorder that eventually becomes refractory to treatment. With genomic and epigenetic analyses, a clearer picture of the various factors at play as the disease course progresses is emerging. Studies consistently show that in every patient with multiple myeloma, several parallel malignant clones are present at the time of diagnosis, with the clonal characteristics changing over time and in relation to therapy.4In patients known to have high-risk disease by cytogenetics, significantly more genomic changes occur over time compared with patients with standard-risk myeloma, suggesting genetic instability in the former.4Thus, while effective treatment may reduce or eliminate the dominant clone, other clones can still exist and gain a survival and/or growth advantage. This may provide a basis for the deeper and more durable responses being seen with combination regimens in the frontline as well as the relapsed myeloma setting.5,6Several reports over the past few years have focused on the interaction of genetic alterations in multiple myeloma with epigenetic changes, such as aberrant DNA and histone methylation or abnormal microRNA (miRNA) expression that are found to contribute to the pathobiology of the disease.7-9The interaction of the malignant clone with its microenvironment, as well as mechanisms that lead to the malignant plasma cell evading such interactions in advanced disease, is also being better understood, leading to the development of newer, distinct classes of drugs.10
Risk Stratification
Once a patient with multiple myeloma meets the criteria for receiving treatment, risk stratification is conducted to discuss and determine prognosis, and even potential treatment strategies. While patient characteristics such as age,11performance status, and disease stage12are important considerations, nearly every patient is riskstratified by looking for mutations using fluorescence in-situ hybridization (FISH) or conventional karyotyping.13,14Beyond defining average outcomes in patients with newly diagnosed multiple myeloma, it was speculated that the cytogenetic risk categories may be used to guide the choice of therapeutic regimen as well as the duration of therapy.15However, data from recent studies show that multiple myeloma patients with standardrisk biology are the ones who are benefiting most from highly effective novel regimens,6,16whereas effective therapies for patients with higher-risk biology are yet to be better defined. The mutations included in various risk categories of MM have also changed over time.17-19While the role of cytogenetics in determining prognosis of patients with is well established and is the basis for several guidelines and clinical trials, newer technologies exploring genomic variability of the malignant clone, utilizing gene expression profiling (GEP), have become available in recent years. These include myPRS, SKY-92,20,21and M3P,22,23which provide a prognostic framework defining patient subgroups and their expected clinical behavior, as well as long-term outcome.
Use of Molecular Data to Determine Treatment Choices
The role of biologic characteristics of the plasma cell beyond risk stratification in determining therapeutic options is emerging. Mutations in the cereblon gene(CRBN)leading to lower expression have been associated with resistance to immunomodulatory drugs (IMiDs) and poorer response rates and overall survival (OS) in patients treated with pomalidomide.24While this seems to be the first biomarker in multiple myeloma with therapeutic implications, it is not yet being used in routine practice, and in my opinion, more standardization and calibration is needed before this may be widely available and used to direct therapeutic choices in routine patient care. Similar biomarkers, which may be helpful in predicting response to proteasome inhibitor treatment in patients with multiple myeloma areIRE1/XBP1, suppression of which confers resistance to bortezomib, although thus far this has been reported mostly in preclinical models with sparse patient-level data.25Another group of biomarkers being tested to determine therapeutic eligibility is the expression of surface antigens on plasma cells, against which monoclonal antibodies (mAbs) are in clinical development (eg, CD38, CD138, CD56). One of the tools that should be available soon for commercial use is a molecular profiling panel called MMprofiler (SkylineDx), which would have the capability of providing the SKY92 prognostic gene signature, cytogenetic markers, GEP clusters, single-gene expression, and patient-level customized genome-wide data.
Updating the Response Criteria
From 1998 until 2006, the clinical responses in patients with multiple myeloma as well as determining disease relapse, were based on the European Group for Blood and Marrow Transplantation (EBMT) criteria.26The IMWG updated these criteria in 2006, when some older definitions were clarified, new response categories were added, and the free light-chain criteria for measurable disease and response were defined.27,28This update went beyond just a state of complete response (CR) to further categorize it into molecular CR, immunophenotypic CR, and stringent CR.27These refinements of the CR category have been validated in various clinical settings and are achievable therapeutic goals to improve patient outcomes.29Because the recently reported and currently utilized treatment regimens for multiple myeloma have been showing better responses than ever noted before, there has been work to further refine the depth of response by determining minimal residual disease (MRD) status of patients. This can be done by utilizing flow cytometry or high-throughput sequencing, and studies have shown that among patients achieving a biochemical CR, MRDnegative status is associated with superior outcomes, including progression-free survival (PFS) and OS.30-32Recent data show that high-throughput sequencing based MRD testing has at least a 10-fold higher sensitivity than the flow cytometry–based methodology.16 While these techniques are being employed commonly in clinical trials, uniform criteria for routine clinical practice are yet to be established.
Another aspect of the change has been the newer imaging modalities, of which positron emission tomography (PET) and MRI scans have been included in disease assessment and progression criteria already.3Further refinement of these techniques has helped in predicting prognosis in various therapeutic settings. For example, presence of more than 3 focal lesions or SUV >4.2 at diagnosis are predictors of shorter PFS, and PET-CT negativity 3 months after an autologous stem cell transplant (ASCT) predicts a superior PFS and OS.33
Shifting Goals of Multiple Myeloma Treatment
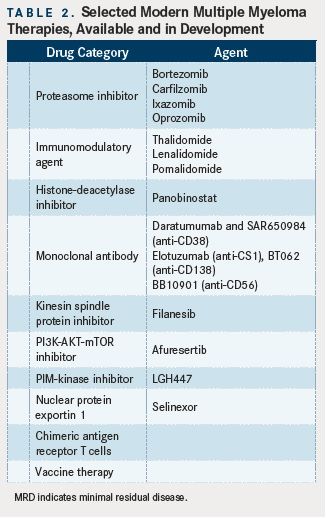
(TABLE 2)
Historically, the treatment algorithm guidelines in multiple myeloma have been based on whether a patient is considered ASCT-eligible or not. This had dichotomized the treatment approach, with the major difference being that younger, transplant-eligible patients would not be given melphalan-based regimens.19While this is still true, the distinction between transplant-eligible and -ineligible patients has been becoming less defined in recent years. The combination therapeutic regimens being used widely utilizing IMiDs and proteasome inhibitors, such as cyclophosphamide- bortezomib-dexamethasone (CyBorD), lenalidomide-bortezomib-dexamethasone (RVd), and carfilzomib-lenalidomide-dexamethoasone (CaRd), are fairly well tolerated and have made the use of melphalan less frequent, at least in the United States.6,34. Since the response rates have been ever improving, achieving an objective response to induction treatment in nearly all patients has become the norm rather than the exception, at least in the newly diagnosed setting and in a significant proportion of patients with relapsed disease. Thus, the comparator arm in randomized, phase III clinical trials is no longer single-agent dexamethasone alone, and novel combination regimens have to show further improvement over the benefit from IMiD and proteasome inhibitor containing doublets, at the least. The goals of treatment and therapeutic decision making have in turn been broadened to address several previously overlooked questions, such as quality of life, survivorship, improving depth of response, managing longterm complications, refining the duration of treatment, and even demonstrating improvement in OS.35-37
The Era of Real Novel Therapeutic Agents
The first “novel” therapeutic agent for the treatment of multiple myeloma to be approved by the FDA was bortezomib, in 2003. Since then, the 2 classes of drugs, proteasome inhibitors and IMiDs, have defined how we manage this disease and have resulted in significantly improved OS and PFS in patients. However, until recently, the only newer agents receiving FDA approval for the treatment of myeloma were more drugs within these 2 classes, with a better side-effect profiles and an improvement in efficacy.38,39 In 2014, an altogether novel category of targeted drugs, the histone-deacetylase (HDAC) inhibitors, became available, with panobinostat being the first agent in this category.40 Although this agent has been received with some debate around its efficacy and adverse-event profile, several combination trials are under way to better define its role in myeloma therapeutics. Nevertheless, the availability of a novel drug class, rather than just novel agents within the older classes, is an exciting development. Several more drug classes are undergoing rapid clinical development, and include mAbs (eg, anti-CD38, anti-CD138, and anti-CS1), a kinesin spindle protein inhibitor (filanesib), a phosphatidylinositide-3-kinase (PI3K)-AKT-mammalian target of rapamycin (mTOR) pathway inhibitor (afuresertib), a PIM-kinase inhibitor (LGH447), and a nuclear protein exportin 1 (selinexor), among others.41Alternative approaches, including vaccine therapy and chimeric antigen receptor (CAR) T cells, are also being explored for multiple myeloma in several ongoing clinical trials.42,43Availability of these and other truly novel therapeutic options will help take the next step toward improving outcomes in patients with multiple myeloma by hopefully affecting disease biology and deepening the response rates, as well as providing more lasting efficacy, potentially realizing an elusive cure in this disease.
References:
- International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group.Br J Haematol.2003;121(5):749-757.
- SEER Cancer Statistics Factsheets: Myeloma. Bethesda, MD: National Cancer Institute.
- Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma.Lancet Oncol.2014;15(12):e538-548. doi: 10.1016/S1470-2045(14)70442-5.
- Keats JJ, Chesi M, Egan JB, et al. Clonal competition with alternating dominance in multiple myeloma.Blood.2012;120(5):1067-1076. doi: 10.1182/ blood-2012-01-405985.
- Kapoor P, Ramakrishnan V, Rajkumar SV. Bortezomib combination therapy in multiple myeloma.Semin Hematol.2012;49(3):228-242. doi: 10.1053/j. seminhematol.2012.04.010.
- Stewart AK, Rajkumar SV, Dimopoulos MA, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma.N Engl J Med.2015;372(2):142- 152. doi: 10.1056/NEJMoa1411321.
- Chapman MA, Lawrence MS, Keats JJ, et al. Initial genome sequencing and analysis of multiple myeloma.Nature.2011;471(7339):467-472. doi: 10.1038/ nature09837.
- Dimopoulos K, Gimsing P, Gronbaek K. Aberrant microRNA expression in multiple myeloma.Eur J Haematol.2013;91(2):95-105. doi: 10.1111/ejh.12124.
- Sharma A, Heuck CJ, Fazzari MJ, et al. DNA methylation alterations in multiple myeloma as a model for epigenetic changes in cancer.Wiley Interdiscip Rev Syst Biol Med.2010;2(6):654-669. doi: 10.1002/wsbm.89.
- Ocio EM, Richardson PG, Rajkumar SV, et al. New drugs and novel mechanisms of action in multiple myeloma in 2013: a report from the International Myeloma Working Group (IMWG).Leukemia.2014;28(3):525-542. doi: 10.1038/ leu.2013.350.
- Ailawadhi S, Aldoss IT, Yang D, et al. Outcome disparities in multiple myeloma: a SEER-based comparative analysis of ethnic subgroups.Br J Haematol.2012;158(1):91-98. doi: 10.1111/j.1365-2141.2012.09124.x.
- Greipp PR, San Miguel J, Durie BG, et al. International staging system for multiple myeloma.J Clin Oncol.2005;23(15):3412-3420.
- Dispenzieri A, Rajkumar SV, Gertz MA, et al. Treatment of newly diagnosed multiple myeloma based on Mayo Stratification of Myeloma and Risk-adapted Therapy (mSMART): consensus statement.Mayo Clin Proc.2007;82(3):323-341.
- Stewart AK, Bergsagel PL, Greipp PR, et al. A practical guide to defining high-risk myeloma for clinical trials, patient counseling and choice of therapy.Leukemia.2007;21(3):529-534.
- Mikhael JR, Dingli D, Roy V, et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines 2013.Mayo Clin Proc.2013;88(4):360- 376. doi: 10.1016/j.mayocp.2013.01.019.
- Korde N, Roschewski M, Zingone A, et al. Treatment with carfilzomiblenalidomide- dexamethasone with lenalidomide extension in patients with smoldering or newly diagnosed multiple myeloma.JAMA Oncol.2015;1(6):746- 754. doi: 10.1001/jamaoncol.2015.2010.
- An G, Xu Y, Shi L, et al. Chromosome 1q21 gains confer inferior outcomes in multiple myeloma treated with bortezomib but copy number variation and percentage of plasma cells involved have no additional prognostic value.Haematologica.2014;99(2):353-359. doi: 10.3324/haematol.2013.088211.
- Rajkumar SV. Treatment of multiple myeloma.Nat Rev Clin Oncol.2011;8(8):479- 491. doi: 10.1038/nrclinonc.2011.63.
- Rajkumar SV. Multiple myeloma: 2012 update on diagnosis, risk-stratification, and management.Am J Hematol.2012;87(1):78-88. doi: 10.1002/ajh.22237.
- Kuiper R, Broyl A, de Knegt Y, et al. A gene expression signature for high-risk multiple myeloma.Leukemia.2012;26(11):2406-2413. doi: 10.1038/leu.2012.127.
- van Laar R, Flinchum R, Brown N, et al. Translating a gene expression signature for multiple myeloma prognosis into a robust high-throughput assay for clinical use.BMC Med Genomics.2014;7:25. doi: 10.1186/1755-8794-7-25.
- Kortum KM, Langer C, Monge J, et al. Targeted sequencing using a 47 gene multiple myeloma mutation panel (M(3) P) in -17p high risk disease.Br J Haematol.2015;168(4):507-510. doi: 10.1111/bjh.13171.
- Kortum KM, Langer C, Monge J, et al. Longitudinal analysis of 25 sequential sample-pairs using a custom multiple myeloma mutation sequencing panel (M(3) P).Ann Hematol.2015;94(7):1205-1211. doi: 10.1007/s00277-015-2344-9.
- Schuster SR, Kortuem KM, Zhu YX, et al. The clinical significance of cereblon expression in multiple myeloma.Leuk Res.2014;38(1):23-28. doi: 10.1016/j. leukres.2013.08.015.
- Leung-Hagesteijn C, Erdmann N, Cheung G, et al. Xbp1s-negative tumor B cells and pre-plasmablasts mediate therapeutic proteasome inhibitor resistance in multiple myeloma.Cancer Cell.2013;24(3):289-304. doi: 10.1016/j. ccr.2013.08.009.
- Blade J, Samson D, Reece D, et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. European Group for Blood and Marrow Transplant.Br J Haematol.1998;102(5):1115-1123.
- Durie BG, Harousseau JL, Miguel JS, et al. International uniform response criteria for multiple myeloma.Leukemia.2006;20(9):1467-1473.
- Kyle RA, Rajkumar SV. Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma.Leukemia.2009;23(1):3-9. doi: 10.1038/leu.2008.291.
- Kapoor P, Kumar SK, Dispenzieri A, et al. Importance of achieving stringent complete response after autologous stem-cell transplantation in multiple myeloma.J Clin Oncol.2013;31(36):4529-4535. doi: 10.1200/JCO.2013.49.0086.
- Martinez-Lopez J, Lahuerta JJ, Pepin F, et al. Prognostic value of deep sequencing method for minimal residual disease detection in multiple myeloma.Blood.2014;123(20):3073-3079. doi: 10.1182/blood-2014-01-550020.
- Rawstron AC, Child JA, de Tute RM, et al. Minimal residual disease assessed by multiparameter flow cytometry in multiple myeloma: impact on outcome in the Medical Research Council Myeloma IX Study.J Clin Oncol.2013;31(20):2540- 2547. doi: 10.1200/JCO.2012.46.2119.
- Mailankody S, Korde N, Lesokhin AM, et al. Minimal residual disease in multiple myeloma: bringing the bench to the bedside.Nat Rev Clin Oncol.2015;12(5):286- 295. doi: 10.1038/nrclinonc.2014.239.
- Zamagni E, Patriarca F, Nanni C, et al. Prognostic relevance of 18-F FDG PET/CT in newly diagnosed multiple myeloma patients treated with up-front autologous transplantation.Blood.2011;118(23):5989-5995. doi: 10.1182/ blood-2011-06-361386.
- Kumar S, Flinn I, Richardson PG, et al. Randomized, multicenter, phase 2 study (EVOLUTION) of combinations of bortezomib, dexamethasone, cyclophosphamide, and lenalidomide in previously untreated multiple myeloma.Blood.2012;119(19):4375-4382. doi: 10.1182/blood-2011-11-395749.
- Ludwig H, Durie BG, McCarthy P, et al. IMWG consensus on maintenance therapy in multiple myeloma.Blood.2012;119(13):3003-3015. doi: 10.1182/ blood-2011-11-374249.
- Sonneveld P, Verelst SG, Lewis P, et al. Review of health-related quality of life data in multiple myeloma patients treated with novel agents.Leukemia.2013;27(10):1959-1969. doi: 10.1038/leu.2013.185.
- Bilotti E, Faiman BM, Richards TA, et al. Survivorship care guidelines for patients living with multiple myeloma: consensus statements of the International Myeloma Foundation Nurse Leadership Board.Clin J Oncol Nurs.2011;15 Suppl:5-8. doi: 10.1188/11.S1.CJON.5-8.
- Siegel DS, Martin T, Wang M, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma.Blood.2012;120(14):2817-2825. doi: 10.1182/blood-2012-05-425934.
- Elkinson S, McCormack PL. Pomalidomide: first global approval.Drugs.2013;73(6):595-604. doi: 10.1007/s40265-013-0047-x.
- San-Miguel JF, Hungria VT, Yoon SS, et al. Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial.Lancet Oncol.2014;15(11):1195-1206. doi: 10.1016/S1470-2045(14)70440-1.
- Mimura N, Hideshima T, Anderson KC. Novel therapeutic strategies for multiple myeloma.Exp Hematol.2015. doi: 10.1016/j.exphem.2015.04.010.
- Garfall AL, Fraietta JA, Maus MV. Immunotherapy with chimeric antigen receptors for multiple myeloma.Discov Med.2014;17(91):37-46.
- Russell SJ, Federspiel MJ, Peng KW, et al. Remission of disseminated cancer after systemic oncolytic virotherapy.Mayo Clin Proc.2014;89(7):926-933.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More