Novel Agents are Changing the Face of Metastatic TNBC
Only 1 treatment option is currently available for treating patients with metastatic germline <em>BRCA</em>-mutated triple-negative breast cancer, but research into novel therapies, including PI3K/conjugates could soon result in a host of new therapies for this hard-to-treat disease.
Joyce A. O'Shaughnessy, MD
Only 1 treatment option is currently available for treating patients with metastatic germline BRCA-mutated triple-negative breast cancer (TNBC), but research into novel therapies, including PI3K/conjugates (ADCs) could soon result in a host of new therapies for this hard-to-treat disease.
“Right now, for TNBC, chemotherapy is our only option,” said Joyce A. O’Shaughnessy, MD, co-chair of Breast Cancer Research and the chair of Breast Cancer Prevention Research at Baylor-Sammons Cancer Center and for The US Oncology Network. “That’s about to change very soon with the likely availability of atezolizumab [Tecentriq].”
Standard-of-care doxorubicin (Adriamycin) and cyclophosphamide followed by paclitaxel (Taxol; AC/T) chemotherapy induces a 5-year disease-free survival of 65% to 80% and a pathological complete response (pCR) rate of 30% to 42% in patients with TNBC. The pCR rate rises to 54% to 58% with carboplatin. pCR is associated with excellent outcomes, but the recurrence rate for patients who do not achieve a pCR is 30% to 70%.
For metastatic disease, the overall survival (OS) is 12 to 18 months. Treatment consists of sequential single-agent chemotherapy. The only clinically available agents target germline BRCA carriers.
Genentech, the manufacturer of atezolizumab, in July announced topline results from the phase III IMpassion130 trial showing that the antiPD-L1 monoclonal antibody combination with nab-paclitaxel (Abraxane) demonstrated statistically significant improvement in progression-free survival (PFS) in treatment-naïve patients with locally advanced or metastatic TNBC.
The company also reported encouraging OS findings in the PD-L1positive population. Furthermore, no new safety signals emerged with the combination, and adverse events were consistent with previous single-agent use of the drugs.
Investigators are also exploring atezolizumab in combination with paclitaxel for patients with inoperable locally advanced or metastatic TNBC in the ongoing phase III IMpassion131 (NCT03125902). PFS is the primary endpoint of the study.
Atezolizumab/nab-paclitaxel is a promising treatment for patients with TNBC, but it is hardly the only therapy under investigation. In a presentation during the 17th Annual International Congress on the Future of Breast Cancer® East, held by Physicians’ Education Resource®in New York, O’Shaughnessy walked her audience through the most recent findings and ongoing research in the field, focusing on agents inhibiting the PI3K/AKT signaling pathway and the ADC sacituzumab govitecan.
Firstline AKT Inhibitors Improve PFS
The PI3K/AKT/mTOR signaling pathway is frequently activated in TNBC. Furthermore, deficient PTEN expression is often found in TNBC and is associated with a higher degree of PI3K pathway activation.
Firstline PI3K/AKT inhibition has shown promising activity in combination with paclitaxel in a pair of phase II placebo-controlled trials, LOTUS and PAKT, and in a phase I/II trial exploring alpelisib (BYL719) plus nab-paclitaxel in patients with locally recurrent or metastatic HER2-negative breast cancer.
“This is an important emerging story,” O’Shaughnessy said. “[These trials] are beginning to enrich for the TNBCs in the metastatic setting that have genomic alterations in the PI3 kinase pathway. AKT is a very important nodal point in TNBC.”
The LOTUS trial included 126 patients who were chemotherapy- free for at least 6 months and who had not received systemic treatment for advanced or metastatic disease. Sixty-two patients were assigned to 400 mg of daily ipatasertib, an oral AKT inhibitor, on days 1 to 21 of a 28-day cycle. Another 62 patients were assigned to placebo. Both groups received 80 mg/m2 of paclitaxel on days 1, 8, and 15 of a 28-day cycle.1
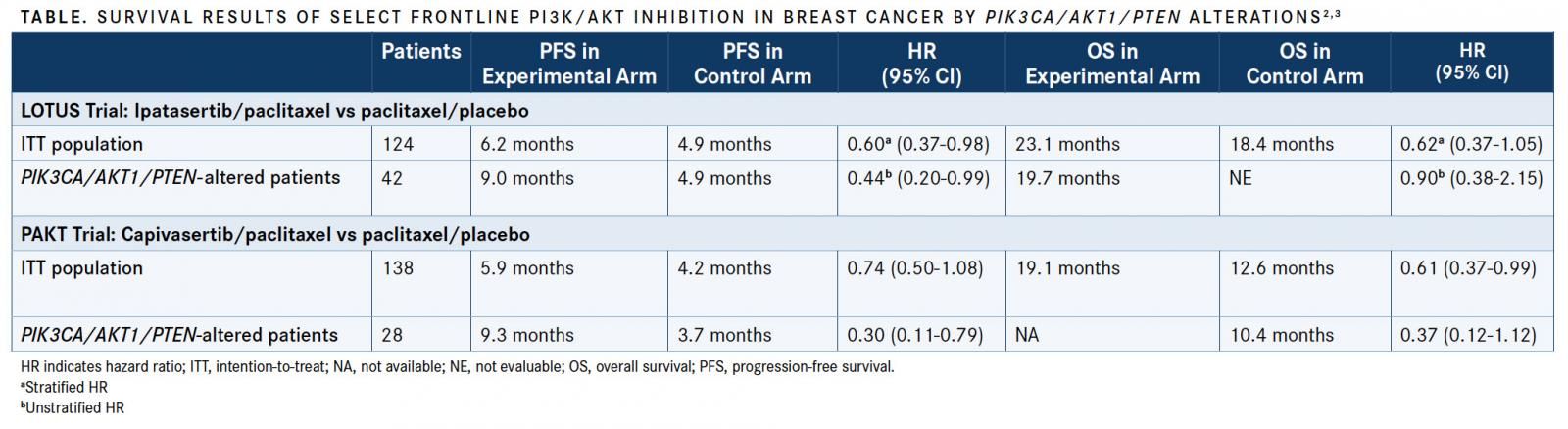
The median PFS in the intent-to-treat (ITT) population (n = 124) was 6.2 months in the ipatasertib arm versus 4.9 months in the placebo arm (stratified HR, 0.60; 95% CI, 0.37-0.98;P= .037). The median PFS benefit among the 42 patients withPIK3CA/AKT1/PTEN-altered tumors was stronger (9.0 vs. 4.9 months; unstratified HR, 0.44; 95% CI, 0.20-0.99; log-rankP= .041) (TABLE).
Interim survival data presented in June at the 2018 ASCO Annual Meeting from the ITT population showed a median OS of 23.1 months in the ipatasertib arm, compared with 18.4 months with placebo (stratified HR, 0.62; 95% CI, 0.37-1.05).2
Ipatasertib in combination with paclitaxel is under investigation in the ongoing, randomized phase II/III IPATunity130 trial (NCT03337724). Investigators hope to determine whether the combination can overcome resistance to chemotherapy, which is a mainstay treatment for patients either with TNBC or ER-positive, HER2-negative breast cancer.
O’Shaughnessy, who is also a member of the IPATunity 130 steering committee, has said in the past that the combination could represent an opportunity to build a new platform for treatment of patients with TNBC or ER-positive disease withPIK3CA/AKT1/PTENmutations.
In PAKT (NCT02423603), patients were assigned to paclitaxel 90 mg/m2 in combination with 400 mg daily AZD5363 (capivasertib; n = 70) or placebo (n = 70).3AZD5363, like ipatasertib, is a highly selective, oral, small molecule AKT inhibitor. Patients were treated in 28-day cycles until progression or unacceptable toxicity.
Eligible patients were diagnosed with either metastatic breast cancer or TNBC. They had received no prior treatment for metastatic disease and no taxane therapy for up to 12 months.
Among patients withPIK3CA/AKT1/PTENaltered tumors (n = 28), the median PFS was 9.3 months in the experimental arm (95% CI, 3.7- 17.7) compared with 3.7 months (95% CI, 1.9-5.9) in the placebo arm (HR, 0.30; 95% CI, 0.11-0.79; 2-sidedP= .01) (TABLE).
Among those with nonaltered tumors, 42 patients were assigned to each treatment group. The median PFS in the experimental arm was 5.3 months (95% CI, 3.5-7.3) compared with 4.4 months (95% CI, 3.5-5.7) in the placebo arm (HR, 1.13; 95% CI, 0.70-1.82; 2-sidedP= .61).
The median OS among the population with altered tumors was not reached (95% CI, 10.2-NR) in the experimental arm compared with 10.4 months (95% CI, 4.0-NR) in the control arm (HR, 0.37; 95% CI, 0.12-1.12; 2-sidedP= .07). In nonaltered patients, the median OS was 16.6 months (95% CI, 10.8-20.4) versus 13.2 months (95% CI, 10.8-17.3) in favor of the capivasertib arm (HR, 0.84; 95% CI, 0.48-1.49; 2-sidedP= .56).
“The AKT inhibitors are quite interesting and may be able to overcome resistance in some of the BL2 and possibly luminal apocrine cancers,” O’Shaughnessy said. “We don’t yet have that subtyping for all these studies, which would be very interesting to see.”
A phase I/II study of alpelisib with nab-paclitaxel in patients with metastatic HER2-negative breast cancer (NCT02379247) included 42 patients, 12 of whom were diagnosed with TNBC. The median PFS in patients with present PI3K pathway activation was 13 months versus 7 months for those without pathway activation (HR, 0.40; 95% CI, 0.18-0.90;P= .017).4The median PFS for the entire population was 9 months (95% CI, 6-12).
Novartis, the manufacturer of alpelisib, in August reported that the phase III SOLAR-1 trial had demonstrated that the PI3K inhibitor plus fulvestrant met the primary endpoint for improved PFS compared with fulvestrant (Faslodex) alone. SOLAR-1 assessed the combination in women with HR-positive/HER2-negativePIK3CA-mutant advanced or metastatic breast cancer who had progressed on or following aromatase inhibitor treatment with or without a CDK4/6 inhibitor. The company plans to release detailed data at a future medical conference.
A New Option on the Horizon
Several ADCs with different targets have been investigated in patients with metastatic TNBC. The one that has shown the highest response rate to date is sacituzumab govitecan (IMMU-132).
The FDA granted sacituzumab govitecan a priority review designation in July 2018 and O’Shaughnessy said that the ADC could be available for patients who have undergone at least 2 previous therapies for metastatic disease by the end of this year. Under the Prescription Drug User Fee Act, the FDA is scheduled to decide by January 18, 2019.
In results from a phase II study presented at the 2017 San Antonio Breast Cancer Symposium, sacituzumab govitecan induced an objective response rate (ORR) of 34% in heavily pretreated patients with metastatic TNBC.5In the 110-patient, single-arm trial, the ORR was accompanied by stable disease for ≥6 months in 11% of patients, for an overall disease control rate of 45%. The median PFS was 5.5 months (95% CI, 4.8-6.6) and the median OS was 12.7 months (95% CI, 10.8-13.6).
“It was quite good in this heavily pretreated triple-negative population. It was really quite striking,” O’Shaughnessy said. “It was tolerable as well, so hopefully that will be approved soon.”
Sacituzumab govitecan consists of the active metabolite of irinotecan, SN-38, linked with a humanized IgG antibody targeted against Trop- 2, a cell-surface glycoprotein that is expressed in approximately 90% of TNBCs. In the phase II study, 57 patients had moderate (2+) to strong (3+) Trop-2 expression by immunohistochemistry, and 5 had weak or absent expression. Data were not available for the remaining patients.
The agent is under investigation in the phase III ASCENT (NCT02574455) trial. A dose of 10 mg/kg of sacituzumab govitecan will be compared with physician’s choice of capecitabine (Xeloda), eribulin (Halaven), gemcitabine (Gemzar), or vinorelbine (Navelbine). Investigators plan to recruit 328 relapsed/refractory patients who have undergone at least 2 prior therapies or >1 therapy for those who progressed within 12 months of completing adjuvant or neoadjuvant therapy.
References:
- Kim SB, Dent R, Im SA, et al. Ipatasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (LOTUS): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial.Lancet Oncol.2017;18(10):1360-1372. doi: 10.1016/S1470-2045(17)30450-3.
- Dent R, Im S-A, Espie M, et al. Overall survival (OS) update of the double- blind placebo (PBO)-controlled randomized phase 2 LOTUS trial of firstline ipatasertib (IPAT) + paclitaxel (PAC) for locally advanced/metastatic triple-negative breast cancer (mTNBC).J Clin Oncol.2018;36(suppl; abstr 1008). meetinglibrary.asco.org/record/160552/abstract.
- Schmid P, Abraham J, Chan S, et al. AZD5363 plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (PAKT): a randomised, double-blind, placebo-controlled, phase II trial.J Clin Oncol.2018;36(suppl; abstr 1007). meetinglibrary.asco.org/record/ 158551/abstract.
- Sharma P, Abramson VG, O’Dea A, et al. Clinical and biomarker results from phase I/II study of PI3K inhibitor BYL 719 (alpelisib) plus nab-paclitaxel in HER2-negative metastatic breast cancer.J Clin Oncol.2018;36(suppl; abstr 1018). meetinglibrary.asco.org/record/158546/abstract.
- Bardia A, Vahdat LT, Diamond J, et al. Sacituzumab govitecan (IMMU-132), an anti-Trop-2-SN-38 antibody-drug conjugate, as ≥3rd-line therapeutic option for patients with relapsed/refractory metastatic triple-negative breast cancer (mTNBC): efficacy results.Cancer Res.2018;78(suppl 4; abstr GS1- 07). doi: 10.1158/1538-7445.SABCS17-GS1-07.
