Neoadjuvant Is Superior to Adjuvant Immunotherapy in Stage III Melanoma
Research has suggested that neoadjuvant immunotherapy combinations are superior to adjuvant immunotherapy for patients with stage III melanoma.

Research has suggested that neoadjuvant immunotherapy combinations are superior to adjuvant immunotherapy for patients with stage III melanoma. Further, with the increased use of neoadjuvant therapy, adjuvant or palliative therapy may not be as necessary for those with melanoma, said Christian U. Blank, MD, PhD, in a presentation during the 2021 World Congress of Melanoma & 17th EADO Congress.
Blank, of the Department of Medical Oncology, Division of Molecular Oncology and Immunology at Netherlands Cancer Institute in Amsterdam, suggested that this is because immunotherapy prior to surgery would allow for the activation of many different T cells, which would continue to attack tumor cells even after a lesion has been removed.1,2
“We think that if the tumor is still present when you start immunotherapy, you can induce a broader and more profound immune response against all different tumor cells. Then you can have a broader immune response in the rest of the body instead of, if you remove the tumor, [being able to] induce only an immune response against the micrometastasis, [which] gives you a less profound immune response,” explained Blank.
This was demonstrated in the landmark phase 1b OpACIN trial (NCT02437279), which looked at the feasibility for neoadjuvant immunotherapy This was demonstrated in the landmark phase 1b OpACIN trial (NCT02437279), which looked at the feasibility for neoadjuvant immunotherapy.
The neoadjuvant approach showed an increased expansion of peripheral blood mononuclear cells from baseline compared with the adjuvant arm.3 This translated to an improvement in relapse-free survival (RFS) for the neoadjuvant arm versus the adjuvant arm (80% vs 60%, respectively, at 3 years) and in overall survival (90% vs 70%, respectively, at 4 years).4 However, Blank stressed that as there were few patients in the trial, the data are not yet practice changing.
The neoadjuvant approach showed an increased expansion of peripheral blood mononuclear cells from baseline compared with the adjuvant arm.3 This translated to an improvement in relapse-free survival (RFS) for the neoadjuvant arm versus the adjuvant arm (80% vs 60%, respectively, at 3 years) and in overall survival (90% vs 70%, respectively, at 4 years).4 However, Blank stressed that as there were few patients in the trial, the data are not yet practice changing.5
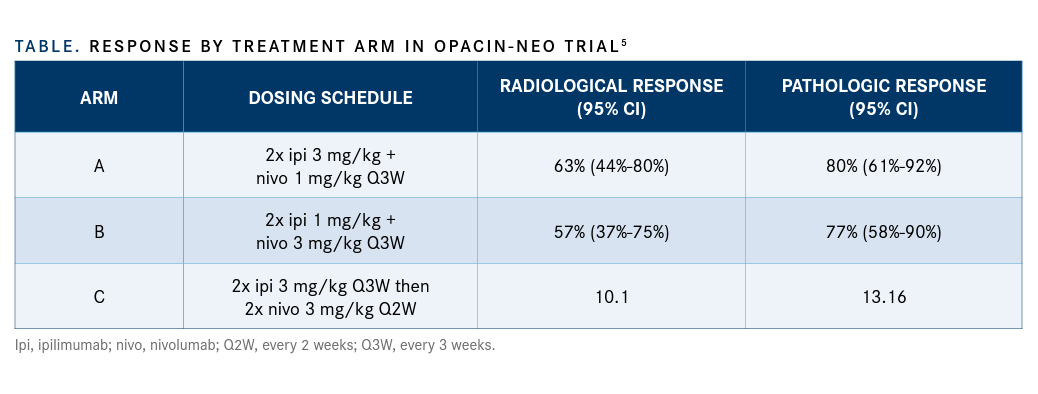
Radiological objective responses were seen in 63% of patients in arm A, 57% in arm B, and 35% in arm C; pathologic responses were seen in 80%, 77%, and 65% of patients in arms A, B, and C, respectively (TABLE). None of the pathologic responders had relapsed after a median follow-up of 8.3 months compared with 43% of the nonresponders. Investigators observed grade Radiological objective responses were seen in 63% of patients in arm A, 57% in arm B, and 35% in arm C; pathologic responses were seen in 80%, 77%, and 65% of patients in arms A, B, and C, respectively (TABLE). None of the pathologic responders had relapsed after a median follow-up of 8.3 months compared with 43% of the nonresponders. Investigators observed grade.
“We have now found…a combination that is very well tolerated and gives excellent outcomes for the patient,” Blank stated.
After 24 months of follow-up without adjuvant therapy, the RFS rate was 90% for arm A, 77.6% for arm B, and 83.3% for arm C.6 According to response, patients who had a pathologic response had a 96.6% RFS rate at 2 years compared with a 35.5% rate in patients who did not have a pathologic response.
The investigators found that patients with high tumor mutational burden (TMB) and a high interferon-γ (IFN-γ)-related gene expression signature score (n = 9) had a 100% event-free survival (EFS) rate at 2 years and a 100% pathologic response rate, compared with a 49.5% EFS rate and a 39% pathologic response rate in patients with a low TMB and IFN-γ score (n = 23).7
The consideration of personalized adjuvant therapy dependent upon response to neoadjuvant immunotherapy led to the creation of the phase 2 PRADO trial, an extension of the OpACIN-neo study. Following treatment with the determined dosing schedule for neoadjuvant ipilimumab/nivolumab and resection, patients with stage IIIB/C de novo or recurrent melanoma who did not respond underwent therapeutic lymph node dissection followed by adjuvant nivolumab every 4 weeks, or dabrafenib (Tafinlar) and trametinib (Mekinist) in patients who were BRAF mutant, with or without added radiation therapy.
The pathologic response rate was 71% in the total cohort (n = 99), with pathologic complete response (pCR) in 50%. Twenty-one percent of patients had no pathologic response and 1 patient was not evaluable.8
Investigators observed immune-related AEs of any grade in 97% of patients, and grade 3/4 events in 22%. The most common (≥ 5 patients) events of any grade were fatigue (55%), rash (47%), and pruritus (27%).
Surgery-related AEs were reported in 54% of patients, 6% of which were grade 3. The most common surgical AEs were seroma (31%) and wound infection (11%). Higher quality-of-life scores were reported in patients who did not require a lymph node dissection.
Ongoing and Emerging Trials
Investigators are working to further establish ipilimumab/nivolumab as a standard neoadjuvant treatment in melanoma by means of the planned phase 3 NADINA trial. They will evaluate neoadjuvant ipilimumab/nivolumab and response- driven adjuvant therapy compared with adjuvant nivolumab in patients with stage III melanoma.
The trial is expected to enroll 420 patients with stage III de novo or recurrent resectable melanoma with at least 1 lymph node metastasis who are naive to immune checkpoint inhibitors. Blank hopes this trial will begin in the second half of the year.
The ongoing phase 1b/2 DONIMI trial (NCT04133948) is exploring the potential of ipilimumab/nivolumab in combination with domatinostat, an HDAC inhibitor, in patients with macroscopic stage III melanoma. Patients receive either nivolumab monotherapy or domatinostat and nivolumab for those with high IFN-γ signatures, and either domatinostat and nivolumab or the triplet for those with low IFN-γ signatures.
“These data are pretty promising because we show for the first time a personalization, a prospective way using the [IFN-γ] signature,” Blank said, who hopes the data will be presented at the 2021 European Society for Medical Oncology Congress.
Declaring Superiority for Immuno-Oncology Combos
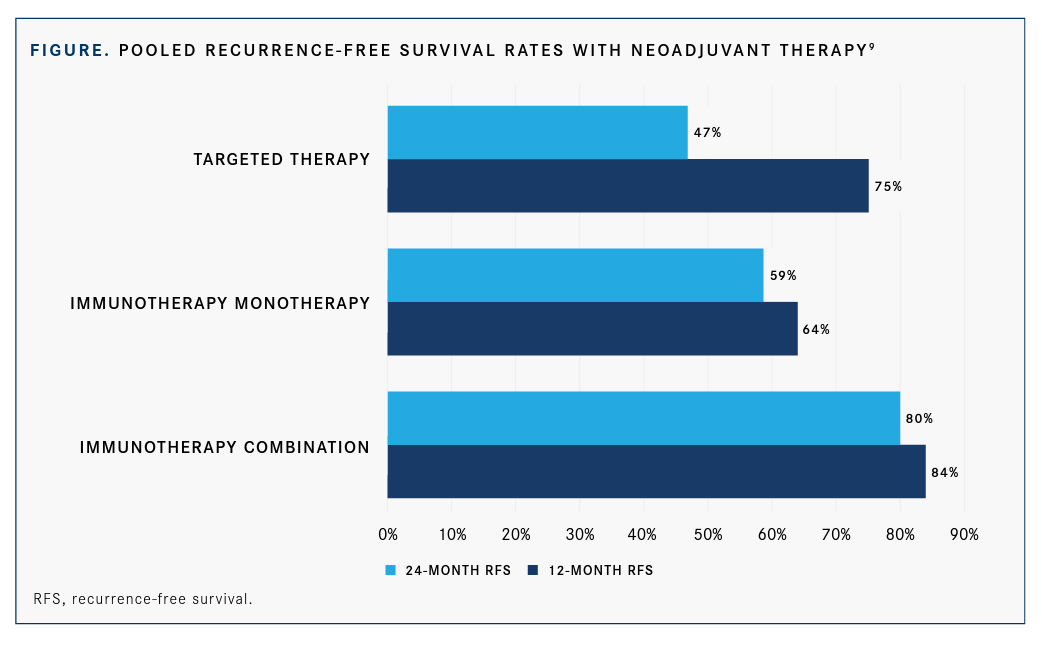
A recent analysis from the International Neoadjuvant Melanoma Consortium (INMC) pooled data from 6 clinical trials of neoadjuvant therapy for patients with melanoma. Across the trials, 192 patients were treated, 141 with immunotherapy and 51 with targeted therapy. In the immunotherapy group, 104 received a combination of ipilimumab/nivolumab and 37 received an anti–PD-1 monotherapy.9
Forty percent of all patients had a pCR, 47% with targeted therapy and 33% with immunotherapy, including 43% for those treated with the immunotherapy combination and 20% among those treated with monotherapy. This correlated with improved RFS and OS rates, though pathologic responses were a better prediction for outcomes in the immunotherapy-treated patients than in the targeted therapy–treated patients.
In the immunotherapy-treated group, all patients who responded to neoadjuvant therapy had close to a 100% RFS rate at 2 years and patients without a response had a 37% RFS rate. Whereas in the targeted therapy group, patients with a pCR had an RFS rate of 79%, those with no pathologic response had an RFS rate of 18% at 2 years. Patients with a partial response had a rate of 0%.
The overall RFS rate was 75% at 2 years for patients treated with immunotherapy and 47% for those treated with targeted therapy (log-rank P = .003). “In the beginning [there is an advantage for targeted therapy, similar to] what we see in stage IV with targeted therapy, but [the curve] crosses very fast and then immunotherapy has a bigger trend, [which results in] long-term outcomes. So neoadjuvant immunotherapy definitely is superior to targeted therapy,” Blank said.
With immunotherapy, the combination regimen led to better responses than monotherapy, with 2-year RFS rates of 80% and 59%, respectively (FIGURE9).
“Therefore, I think we should go to a personalized immunotherapy in combination therapies and signature driven [decision making],” Blank said, detailing how he expects to make treatment decisions going forward. “In the future, we will biopsy our patients and we will do these algorithms…and based on the signature that these patients have, we will give the combination therapy. With that, I think we will achieve within the next 5 years a 95% response rate for the patients.”
References:
1. Blank C. Neoadjuvant checkpoint inhibitor combinations. Presented at: 10th World Congress of Melanoma & 17th EADO Congress; April 15-17, 2021; Virtual.
2. Versluis JM, Long GV, Blank CU. Learning from clinical trials of neoadjuvant checkpoint blockade. Nat Med. 2020;26(4):475-484. doi:10.1038/ s41591-020-0829-0
3. Blank CU, Rozeman EA, Fanchi LF, et al. Neoadjuvant versus adjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma. Nat Med. 2018;24(11):1655-1661. doi:10.1038/s41591-018-0198-0
4. Versluis JM, Reijers ILM, Rozeman EA, et al. 4-year relapse-free survival (RFS), overall survival (OS) and long-term toxicity of (neo)adjuvant ipilimumab (IPI) + nivolumab (NIVO) in macroscopic stage III melanoma: OpACIN trial. Ann Oncol. 2020;31(suppl 4):S742-S743. doi:10.1016/j. annonc.2020.08.1221
5. Rozeman EA, Menzies AM, van Akkooi ACJ, et al. Identification of the optimal combination dosing schedule of neoadjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma (OpACIN-neo): a multicentre, phase 2, randomised, controlled trial. Lancet Oncol. 2019;20(7):948-960. doi:10.1016/S1470-2045(19)30151-2
6. Rozeman EA, Reijers ILM, Hoefsmit EP, et al. Twenty-four months RFS and updated toxicity data from OpACIN-neo: a study to identify the optimal dosing schedule of neoadjuvant ipilimumab (IPI) and nivolumab (NIVO) in stage III melanoma. J Clin Oncol. 2020;38(suppl 15):10015. doi:10.1200/ JCO.2020.38.15_suppl.10015
7. Rozeman EA, Hoefsmit EP, Reijers ILM, et al. Survival and biomarker analyses from the OpACIN-neo and OpACIN neoadjuvant immunotherapy trials in stage III melanoma. Nat Med. 2021;27(2):256-263. doi:10.1038/ s41591-020-01211-7
8. Blank CU, Reijers ILM, Pennington T, et al. First safety and efficacy results of PRADO: a phase II study of personalized response-driven surgery and adjuvant therapy after neoadjuvant ipilimumab (IPI) and nivolumab (NIVO) in resectable stage III melanoma. J Clin Oncol. 2020;38(suppl 15):10002. doi:10.1200/JCO.2020.83.15_suppl.10002
9. Menzies AM, Amaria RN, Rozeman EA, et al. Pathological response and survival with neoadjuvant therapy in melanoma: a pooled analysis from the International Neoadjuvant Melanoma Consortium (INMC). Nat Med. 2021;27(2):301-309. doi:10.1038/s41591-020-01188-3