Neoadjuvant Chemotherapy Considerations in Triple-Negative Breast Cancer
The optimal neoadjuvant chemotherapy regimen in triple-negative breast cancer has not been clearly defined. Achieving a pathologic complete response provides important prognostic information, and, especially in TNBC, is considered a surrogate endpoint for event-free survival.
Angela Demichele, MD, MSCE
Abstract
The optimal neoadjuvant chemotherapy (NACT) regimen in triple-negative breast cancer (TNBC) has not been clearly defined. Achieving a pathologic complete response (pCR) provides important prognostic information, and, especially in TNBC, is considered a surrogate endpoint for event-free survival. Thus, many neoadjuvant studies in TNBC focus on this as a primary endpoint, and such information may be used for accelerated US Food and Drug Administration approval. Current controversies in the field include: (1) the role of platinumbased compounds; (2) the optimal chemotherapy backbone; and (3) the benefits of additional therapy after surgery. Conflicting results of 2 major studies adding carboplatin to NACT have highlighted the need to balance potential benefits to disease outcomes against increased toxicity. While the PROGECT study suggests efficacy of a nonanthracycline-containing regimen, this is observational data, and evidence in the form of a clinical trial remains to be seen. Data surrounding optimal taxane use support the use of nab-paclitaxel in place of paclitaxel in limited clinical situations. Although bevacizumab may increase pCR rates, this has not translated into survival benefit. Capecitabine shows promise in patients who have not achieved pCR after NACT. The neoadjuvant setting remains an important model for drug development. This review will focus on the most important and most current neoadjuvant trials in women with TNBC.
Introduction
Accounting for 13% of breast cancer cases annually,1triple-negative breast cancer (TNBC) is so designated due to the lack of expression of the estrogen (ER), progesterone (PR), and HER2 receptors. TNBC portends the worst prognosis among the major subtypes of breast cancer, and both the limitations in our understanding of the underlying biology and the lack of targeted therapy are primary challenges in treating this disease,2with cytotoxic chemotherapy remaining the mainstay of systemic treatment. Although TNBCs carry a higher mortality as compared with luminal-type breast cancers (ER/PR-positive [ER/PR+], HER2-negative), neoadjuvant chemotherapy (NACT) is more likely to result in a pathologic complete response (pCR) in patients with TNBC primary tumors than in those with luminal tumors.3Pathologic complete response is an important endpoint because patients who attain this status after surgery have improved survival, and this improved prognosis is greatest in the more aggressive subtypes of TNBC and HER2- positive-only tumors.4
In addition to the prognostic information gained from pathologic analysis of the primary tumor after NACT, it also provides researchers an opportunity to expeditiously determine a drug’s efficacy. Studying drugs in the adjuvant setting depends on the timeto- event (ie, recurrence); however, the neoadjuvant setting provides evidence of treatment effects immediately after surgery. Although benefit in the neoadjuvant setting is thought to predict survival in the adjuvant setting, this is not clearly established, and caution should be taken when extrapolating pCR data into true survival endpoints.5Thus, the neoadjuvant setting remains an important model for drug development. This review will focus on the most important and most current neoadjuvant trials in women with TNBC.
Addition of Carboplatin
Carboplatin is an attractive drug for use in TNBC due to its particular relevance to the pathobiology of TNBC. About 80% of BRCA1 mutation‒associated breast cancers are triple-negative, and are generally regarded as particularly sensitive to interstrand cross-linking agents, such as platinum analogs, due to the defect in homologous recombination (HR)-based DNA repair characteristic of a BRCA1 mutation.6Additionally, a subset of TNBC tumors exhibit similar defects in HR-based DNA repair, even in the absence of a germline BRCA mutation,7 and these tumors may be carboplatin-sensitive.8Singleagent, platinum-based therapy has had varied success in metastatic TNBC, with prospective studies reporting response rates that vary from 10% to 40%.9
More recently, 2 studies have investigated the addition of carboplatin to standard-combination NACT in patients with TNBC. The CALGB 40603 study,10conducted in the United States, was a phase II, 2 × 2 factorial trial that investigated the benefit of adding carboplatin, bevacizumab, or the combination to taxane/anthracycline-based chemotherapy. The trial enrolled 443 women with stage II/III TNBC into 1 of 4 arms. The chemotherapy backbone was 12 weeks of weekly paclitaxel (80 mg/m2), followed by dose-dense doxorubicin and cyclophosphamide (ddAC) every 2 weeks for 4 cycles (60 mg/m2and 600 mg/m2, respectively), which formed the control group to 3 experimental arms: (1) bevacizumab 10 mg/kg every 2 weeks for 9 cycles; (2) carboplatin area under the curve (AUC) 6 every 3 weeks for 4 cycles; and (3) both bevacizumab and carboplatin, dosed as above. These arms gave the experimental drug(s) concurrently with paclitaxel, with bevacizumab also partially overlapping with the ddAC treatment period.
The addition of carboplatin significantly increased the pCR rate compared with control, from 46% to 60% (OR, 1.76,P= .0018).10 While the addition of bevacizumab resulted in a similar pCR rate, the combination of both agents resulted in the numerically highest pCR rate of 67%. However, in the subsequent survival analysis, adding carboplatin did not significantly impact survival.11The absolute benefit in 3-year event-free survival (EFS) of adding carboplatin was 4.9% (76.5% vs 71.6%, respectively; HR, 0.84; 95% CI, 0.58-1.22;P= .36). Overall survival (OS) differences were also not significant, with 81.9% OS in the carboplatin group versus 84.6% without carboplatin (HR, 1.15; 95% CI, 0.74-1.79;
P= .53).11Furthermore, toxicity was higher in the carboplatin group, with those who received carboplatin being less likely to complete therapy without skipping doses, requiring a dose modification, or discontinuing therapy early. Grade ≥3 neutropenia and thrombocytopenia were also more common in the carboplatin group (56% and 20%, respectively) as
compared with control (22% and 4%, respectively).10
These results conflict with those in the Gepar- Sixto trial. In GeparSixto,12a total of 595 patients with centrally confirmed TNBC were enrolled into 2 groups, with both groups receiving 18 weeks of weekly paclitaxel, weekly nonpegylated liposomal doxorubicin, and bevacizumab every 3 weeks. The experimental arm additionally received weekly carboplatin. A total of 333 women completed treatment in the combined arms. In the TNBC subgroup, carboplatin resulted in a significantly improved pCR rate over control (53% vs 37%;P= .005). This translated into an absolute benefit in 3-year EFS for the addition of carboplatin over control of 9.7% (85.8% vs 76.1%, respectively; HR, 0.56 [95% CI, 0.33-0.96]).12
Clearly, the outcomes were better in the Gepar- Sixto trial compared with CALGB 40603. However, there are several differences between these 2 studies worth noting. GeparSixto had more-favorable baseline characteristics, as 26% of patients in GeparSixto were cN0, compared with 42% in CALGB 40603. Additionally, a larger proportion were cT1 in GeparSixto (26% vs 11%). The backbone therapy was also more intensive in GeparSixto, although this would be expected to affect all arms. In CALGB 40603, the backbone therapy also included cyclophosphamide, which can also cause DNA damage like platinum agents, potentially making the treatment effect similar in the control and experimental arms. Last, the dosing intervals were more compact in GeparSixto, which would potentially allow for less time for DNA repair. Toxicity was greater in the carboplatin- containing arms of both studies, but more grade 3/4 toxicities were seen in GeparSixto relative to CALGB 40603. There are also no data on the long-term effects of these experimental regimens because the median follow-up time was only 3 years.
With these 2 studies in mind, the decision to add carboplatin to a NACT regimen remains an individualized one. Although the hazard ratios suggest benefit, its small size suggests that many patients do just fine without the addition of carboplatin, and can be spared the toxicity. When considering the addition of carboplatin, the backbone regimen and dosing schedule of carboplatin may be critical to optimal efficacy of the drug. If carboplatin is added, clinicians should be cautious given the unknown longterm effects of the added toxicity.
A recent study also worth noting combines carboplatin with another drug aimed at exploiting HR-based DNA repair deficiencies. The I-SPY 2 investigators conducted a phase II study of the adaptive randomization of adding veliparib and carboplatin to the paclitaxel portion of weekly paclitaxel followed by doxorubicin and cyclophosphamide, with pCR being the primary endpoint.13Veliparib, a potent inhibitor of oral poly(ADP-ribose) polymerase (PARP), was chosen because of preclinical trials showing that it potentiates the antineoplastic effects of carboplatin.14In patients with TNBC, the pCR rate in the experimental arm was 51% versus 26% in the control arm, resulting in a 99% probability of superiority over control, and an 88% probability of success in a phase III clinical trial. The toxicity profile was similar to that in the CALGB 40603 trial. While this combination appears to improve the rate of pCR compared with control, it is impossible to separate the effects of carboplatin and veliparib. Preliminary data from the Brightness Study presented at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting helps to clarify this issue.
The Brightness Study randomized 634 patients with resectable, early-stage TNBC to neoadjuvantly receive 1 of 3 paclitaxel-AC‒containing arms: veliparib with carboplatin, carboplatin, or backbone therapy alone.15There was no difference in pCR rate between the 2 carboplatin-containing groups (53.2% with veliparib/carboplatin vs 57.5% with carboplatin;P= .36), and both carboplatin-containing groups had a higher pCR rate than the control group (31%;P<.001 in both groups).15 These data suggest that the benefit seen in the I-SPY 2 trial was primarily due to carboplatin. Survival outcomes for the Brightness Study are still pending.
Additional studies investigating the role of adjuvant platinum-based therapy are currently ongoing. An ECOG-ACRIN study (E1131, NCT02445391)16randomizes patients who have residual TNBC after NACT to 2 arms: cisplatin or carboplatin versus capecitabine. An NRG study (NRG-BR003, NCT02488967),17though excluding patients who had received prior NACT, is investigating the addition of carboplatin to AC-paclitaxel solely in the adjuvant setting, and may provide further insight into the efficacy of carboplatin in TNBC.
Necessity of Anthracyclines
Anthracyclines are effective in early-stage breast cancer, but carry long-term cardiovascular and secondary leukemia risks.18,19The PROGECT study20sought to determine whether an anthracycline-sparing regimen would be sufficiently efficacious to enable patients to forgo treatment with an anthracycline. The study was a prospective registry of 2 cohorts from Kansas and Spain composed of 190 patients with stage I-III TNBC, who were either BRCA1/2 carriers (16%) or noncarriers. These patients received neoadjuvant CbD, consisting of carboplatin (AUC 6) and docetaxel (75 mg/m2) every 3 weeks for 4 to 6 cycles. After NACT and surgery, residual cancer burden and pCR were evaluated.
The overall pCR rate was 55%, with BRCA status having no significant impact on pCR. The authors note that this is similar to the pCR rate achieved when carboplatin is added to anthracycline-containing regimens.20Patients with stage III disease had a significantly lower likelihood of achieving pCR (37%), although these patients comprised about 30% of the study population, and about half the patients had node-positive disease. The authors also note that the toxicity profile of CbD was more favorable than anthracycline- containing regimens. Whereas only 50% to 76% of patients complete all cycles of carboplatin/ anthracycline-containing regimens, upwards of 83% of patients taking CbD completed all treatment.
The results of this observational study are promising. Although an initial analysis of the Kansas-only population reported a slightly higher pCR rate,21a major criticism was that this high rate may reflect selection bias due to higher numbers of patients with node-negative disease. However, in the combined analysis, nodal demographics were similar to those of other randomized, neoadjuvant TNBC clinical trials. With a substantial pCR rate and favorable toxicity profile, the CbD regimen warrants further investigation in a prospective, randomized clinical trial, which is currently ongoing (NCT02413320).
Page Break:
Optimal Choice of Taxane
The activity of taxanes in neoadjuvant regimens is perhaps best exhibited in the NSABP B-18/B-27 study,22with the addition of docetaxel to AC resulting in improved pCR rate. Efforts have been made to identify the optimal taxane for each clinical setting, with nanoparticle-albumin-bound-paclitaxel (nab-paclitaxel) being of particular interest in the neoadjuvant setting due to previously reported absence of hypersensitivity reactions, ability to infuse a higher dosage over a shorter period, and improved response rates.23The ETNA trial,24presented at the 2016 ASCO meeting, randomized women with operable or locally advanced TNBC or luminal B-like breast cancer to receive either paclitaxel (90 mg/m2, 3 weeks on, 1 week off, for 4 cycles) or nab-paclitaxel (125 mg/m2, 3 weeks on, 1 week off, for 4 cycles) prior to an anthracycline-containing NACT regimen. The primary endpoint was pCR rate. A total of 695 patients were eligible and randomized, with about 30% in each group having TNBC and 50% having nodal involvement.
The pCR rate was not significantly different between the 2 treatment arms (18.6% for paclitaxel, 22.5% for nab-paclitaxel;P= .19). In a planned subgroup analysis, there remained no significant difference between nab-paclitaxel and paclitaxel with regard to the TNBC population (pCR rate, 41.3% vs 37.3%, respectively; odds ratio [OR], 0.85; 95% CI, 0.49-1.45). Additionally, toxicity was worse among the patients receiving nabpaclitaxel, with higher rates of grade 3/4 peripheral neuropathy, neutropenia, fatigue, and vomiting.24
These results conflict with the findings in the GeparSepto trial. Although having a similar design,25GeparSepto differed in that it also allowed women with HER2 disease, had a standardized nontaxane backbone of epirubicin and cyclophosphamide, and more aggressively dosed nab-paclitaxel (125 mg/m2, weekly without interruption). In a preplanned subgroup analysis of TNBC subjects, nab-paclitaxel was associated with a significantly higher rate of pCR compared with paclitaxel (48% vs 26%, respectively;P= .00027; OR, 2.61; 95% CI, 1.57-4.33).25Toxicity was also higher in the nab-paclitaxel group, with significantly higher rates of grade 3/4 anemia and peripheral neuropathy, while neutropenia, fatigue, and vomiting were not significantly different.
This larger effect may be due in part to the difference in dosing between the 2 taxanes, with a relatively smaller paclitaxel dosage and larger nabpaclitaxel dosage. Although it is unclear that the small increase in pCR rate would ever translate into a recurrence-free survival (RFS) benefit, it clearly comes at an increased toxicity and financial cost. Although nab-paclitaxel may be a good alternative if the patient has an allergic reaction to paclitaxel, the data suggesting its preferred use over paclitaxel are, at this point, largely insufficient.
Use of Bevacizumab
Bevacizumab, an anti-VEGF monoclonal antibody, was first studied in the metastatic breast cancer setting in 2007, and both clinical trials and meta-analyses showed improved progression-free survival (PFS), but not OS.26-29Although the initial promise of improved progression-free survival (PFS) in ECOG E2100 led to the FDA granting approval to bevacizumab in the metastatic setting,26 it was later revoked in 2011 after the phase III RIBBON-1 and AVADO studies showed less-positive results at the cost of significant toxicity.27,28,30In the adjuvant setting, the BEATRICE study31failed to show improvement in invasive RFS in patients with intermediate- risk TNBC when bevacizumab was added to adjuvant chemotherapy.
In the neoadjuvant setting, there have been conflicting results. GeparQuinto and CALGB 40603 both showed an increased rate of pCR in the bevacizumab arms of about 10% over the non-bevacizumab arms.10,32However, an update of CALGB 40603 presented at the 2015 San Antonio Breast Cancer Symposium showed that even though individual patients who achieved pCR had improved RFS and OS, these clinical benefits were not significantly associated with the addition of bevacizumab to standard therapy at the trial level.11Notably, the study was underpowered to make this distinction. These 2 trials contradict NSABP B40, which showed benefit for pCR33and OS34only in women with hormone receptor (HR)‒positive disease, with negative findings in the TNBC subgroup.
The ARTemis study35,36recently announced disease- free survival (DFS) and OS data at 3.4 years of follow-up. ARTemis randomized women with HER2- negative breast cancer, stratifying on HR status, to receive a core NACT regimen of 3 cycles of docetaxel (D) followed by 3 cycles of cyclophosphamide, epirubicin, and fluorouracil (CEF), with or without bevacizumab. A previous report revealed that significantly more patients in the bevacizumab group achieved pCR, and this effect was more pronounced in the TNBC subgroup (45% vs 31%) as well as the weakly- ER-positive group (51% vs 30%).36However, pCR was not associated with improved OS or disease-free survival in the bevacizumab groups, whereas in the non-bevacizumab containing arms, pCR retained its association with DFS and OS.35These data led the authors to postulate that micrometastatic breast cancer may grow in an angiogenesis-independent manner. Therefore, at present, there is no clearly defined clinical benefit of bevacizumab in neoadjuvant TNBC.
A Role for Post-Neoadjuvant Capecitabine?
Given the still significantly high rates of residual disease after neoadjuvant therapy in TNBC, which portends inferior EFS, another approach to improving outcomes in this population is to add additional adjuvant therapy after surgery. Standard of care does not include additional therapy in the presence of residual disease. Thus, there is an opportunity to test strategies in this population that is currently undergoing only surveillance. Moreover, such studies are more efficient than standard adjuvant trials because they are enriched for the population of patients at highest risk of recurrence, and thus, likely to have a greater number of events in the early posttreatment period.
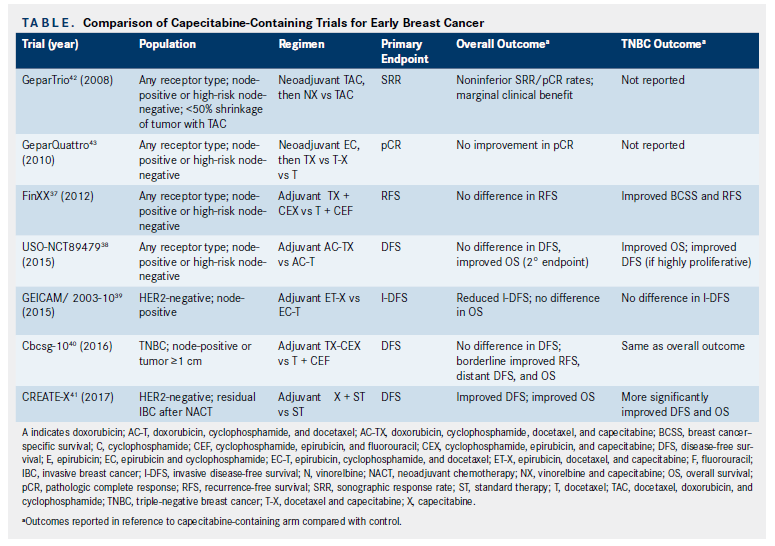
Several studies (Table) have investigated the use of capecitabine adjuvantly in this setting, and have yielded conflicting results. Although FinXX37showed that adding capecitabine improved breast cancer‒specific survival overall and RFS in the TNBC subgroup, and a USO study (NCT00089479)38showed improved OS with capecitabine, GEICAM/2003-1039actually showed worse invasive DFS with capecitabine.
Because of the suggestion of benefit in the TNBC population, the Cbcsg-10 trial investigated the addition of adjuvant capecitabine to a taxane/anthracycline backbone in patients with TNBC who had not previously received NACT.40Although the combination of drugs in each arm were essentially the same as in the FinXX study, the dosing was slightly different between the 2, with the FinXX group giving relatively lower dosages of docetaxel and capecitabine in the experimental arm, and a slightly higher dosage of docetaxel in the control arm. The 30-month follow- up data were reported at the 2016 ASCO meeting.40DFS was not significantly different between the experimental and control groups (90.6% vs 86.8%;P= .23). There were borderline significant findings for any recurrence or death (6.6% vs 11.4%;P= .048); distant DFS (94.3% vs 89.3%;P= .019); and a trend towards OS benefit (97.4% vs 95.6%;P= .063).40
In terms of toxicity and tolerability of capecitabine, a little more than one-third of patients completed the 8-week course with either the planned or a reduced dosage of capecitabine, with 25.4% discontinuing therapy, resulting in a relative dose intensity of 78.7%.41There were greater rates of neutropenia and diarrhea in the experimental arm, and the incidence of grade 3/4 hand-foot syndrome was 11.1%. Although these results show a surprising benefit, especially in the TNBC subgroup, toxicity limits the ability to give the intended therapy. These results contradict the findings in GeparTrio,42which found that adding capecitabine and vinorelbine to patients who were not responding sonographically to NACT yielded only a marginal 6% pCR rate. CREATE-X also contradicts GeparQuattro,43which showed that adding capecitabine to neoadjuvant epirubicin and cyclophosphamide did not significantly increase pCR rate.
Future Directions
Immunotherapy is being actively investigated in TNBC in the neoadjuvant setting, and preliminary results are promising. Efficacy results from the I-SPY 2 trial of the checkpoint inhibitor pembrolizumab were reported at the 2017 ASCO annual meeting.44Patients with high-risk, HER2-negative breast cancer were randomized to neoadjuvant weekly paclitaxel with or without pembrolizumab (200 mg every 3 weeks × 4) followed by AC. In the TNBC population (n = 118), the estimated pCR rates were roughly 3-fold higher in the pembrolizumab arm compared with control (62.4% vs 22.3%, respectively), which translates into a >99% probability of superiority of the pembrolizumab-containing regimen over control, and a >99% probability of success in a phase III clinical trial.44 Other trials currently ongoing include a phase II trial (NCT02957968)45that is adding the combination of decitabine plus pembrolizumab to standard neoadjuvant regimens, as well the phase III SWOG S1418/BR006 trial (NCT02954874)46utilizing adjuvant pembrolizumab in patients with TNBC with residual disease after NACT.
Conclusions
Although many unanswered questions still remain about the optimal NACT regimen, the studies summarized in this review can offer some guidance for both clinicians and researchers. Although Gepar- Sixto and CALGB 40603 suggest some benefit, the choice to use carboplatin is an individualized decision, and may be warranted when there is a need for rapid control of locoregional disease, for those who are at greatest risk for relapse (stage III, very young age). Lack of long-term safety data also underscores the importance of careful patient selection. The PROGECT study, while suggesting that CbD therapy yields comparable pCR rates, is still an observational study. In the absence of a clinical trial (which is ongoing), an anthracycline-containing regimen should remain the standard of care. The contrasting ETNA and GeparSepto studies do not support the use of nab-paclitaxel over paclitaxel, although it is a reasonable alternative for those who are allergic to paclitaxel. With the recently reported results of ARTemis and CALGB 40603, there is no survival benefit to adding bevacizumab to a neoadjuvant regimen, even though pCR rates may be improved, suggesting that micrometastatic disease may not rely strongly on angiogenesis pathways. Finally, while the data for capecitabine are not compelling enough to add it routinely in the adjuvant or neoadjuvant setting in TNBC, there may be a role for it when residual disease remains after NACT, with greatest benefit seen in TNBC.
Although studies of capecitabine as a part of a standard adjuvant regimen are not compelling enough to warrant a broad change in current practice, the CREATE-X trial41sought to incorporate adjuvant capecitabine in a different clinical context. The study randomized 900 patients with stage I-IIIB, HER2-negative breast cancer who had received NACT and did not achieve pCR (or who had node-positive disease at surgery) to receive standard postoperative therapy (including hormone therapy for ER+ disease) with or without adjuvant capecitabine (1250 mg/m22 weeks on, 1 week off). The preliminary efficacy analysis met the primary DFS endpoint, and thus the trial was terminated early due to an 8.9% absolute increase in freedom from recurrence or second cancer at 3 years of follow- up (82.8% in the capecitabine group vs 73.9% in the control group;P= .01). The 5-year OS also was longer in the capecitabine group (89.2% vs 83.6% in the control group;P= .01). In a subgroup analysis, an even greater benefit was seen in the TNBC group, with a 13.1% absolute increase in DFS (69.8 vs 56.1 in controls), and a hazard ratio for recurrence, second cancer, or death of 0.58 (95% CI, 0.39-0.87).41
References
- Plasilova ML, Hayse B, Killelea BK, et al. Features of triple-negative breast cancer: analysis of 38,813 cases from the national cancer database.Medicine(Baltimore). 2016;95(35):e4614. doi: 10.1097/MD.0000000000004614.
- Ademuyiwa FO, Groman A, Hong CC, et al. Time-trends in survival in young women with breast cancer in a SEER population-based study.Breast Cancer Res Treat. 2013;138(1):241-248. doi: 10.1007/s10549-013-2425-1.
- Carey LA, Dees EC, Sawyer L, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes.Clin Cancer Res. 2007;13(8):2329-2334.
- Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis.Lancet. 2014;384(9938):164-172. doi: 10.1016/S0140-6736(13)62422-8.
- DeMichele A, Yee D, Berry DA, et al. The neoadjuvant model is still the future for drug development in breast cancer.Clin Cancer Res. 2015;21(13):2911-2915. doi: 10.1158/1078-0432.CCR-14-1760.
- Turner NC, Tutt ANJ. Platinum chemotherapy for BRCA1-related breast cancer: do we need more evidence?Breast Cancer Research. 2012;14(6):115-115.
- Popova T, Manié E, Rieunier G, et al. Ploidy and large-scale genomic instability consistently identify basal-like breast carcinomas with BRCA1/2 inactivation.Cancer Res. 2012;72(21):5454-5462. doi: 10.1158/0008-5472.CAN-12-1470.
- Isakoff SJ, Mayer EL, He L, et al. TBCRC009: a multicenter phase II clinical trial of platinum monotherapy with biomarker assessment in metastatic triple-negative breast cancer.J Clin Oncol. 2015;33(17):1902-1909. doi: 10.1200/JCO.2014.57.6660.
- Liu M, Mo Q-G, Wei C-Y, et al. Platinum-based chemotherapy in triplenegative breast cancer: a meta-analysis. Oncol Lett. 2013;5(3):983-991.
- Sikov WM, Berry DA, Perou CM, et al. Impact of the addition of carboplatin and/or bevacizumab to neoadjuvant once-per-week paclitaxel followed by dose-dense doxorubicin and cyclophosphamide on pathologic complete response rates in stage II to III triple-negative breast cancer: CALGB 40603 (Alliance).J Clin Oncol. 2015;33(1):13-21. doi: 10.1200/JCO.2014.57.0572.
- Sikov W, Berry D, Perou C, et al. Event-free and overall survival following neoadjuvant weekly paclitaxel and dose-dense AC +/- carboplatin and/ or bevacizumab in triple-negative breast cancer: outcomes from CALGB 40603 (Alliance). Presented at the 38th Annual San Antonio Breast Cancer Symposium; December 8-12, 2015; San Antonio, TX. Abstract S2-05.
- von Minckwitz G, Schneeweiss A, Loibl S, et al. Neoadjuvant carboplatin in patients with triple-negative and HER2-positive early breast cancer (GeparSixto; GBG 66): a randomised phase 2 trial.Lancet Oncol.2014;15(7):747-756. doi: 10.1016/S1470-2045(14)70160-3.
- Rugo HS, Olopade OI, DeMichele A, et al. Adaptive randomization of veliparibcarboplatin treatment in breast cancer.N Engl J Med. 2016;375(1):23-34. doi: 10.1056/NEJMoa1513749.
- Donawho CK, Luo Y, Luo Y, et al. ABT-888, an orally active poly(ADP-ribose) polymerase inhibitor that potentiates DNA-damaging agents in preclinical tumor models.Clin Cancer Res. 2007;13(9):2728-2737.
- Geyer CE, O’Shaughnessy J, Untch M, et al. Phase 3 study evaluating efficacy and safety of veliparib (V) plus carboplatin (Cb) or Cb in combination with standard neoadjuvant chemotherapy (NAC) in patients (pts) with early stage triple-negative breast cancer (TNBC).J Clin Oncol. 2017;35(suppl 15; abstr 520).
- Platinum based chemotherapy or capecitabine in treating patients with residual triple-negative basal-like breast cancer following neoadjuvant chemotherapy (NCT02445391). 2017; https://clinicaltrials.gov/ct2/show/ NCT02445391. Updated December 8, 2017. Accessed December 20, 2017.
- Doxorubicin hydrochloride and cyclophosphamide followed by paclitaxel with or without carboplatin in treating patients with triple-negative breast cancer (NCT02488967). 2017; https://clinicaltrials.gov/ct2/show/ NCT02488967. Updated October 5, 2016. Accessed December 20, 2017.
- Tan TC, Neilan TG, Francis S, et al. Anthracycline-induced cardiomyopathy in adults.Compr Physiol. 2015;5(3):1517-1540. doi: 10.1002/cphy.c140059.
- Wolff AC, Blackford AL, Visvanathan K, et al. Risk of marrow neoplasms after adjuvant breast cancer therapy: the National Comprehensive Cancer Network experience.J Clin Oncol.2015;33(4):340-348. doi: 10.1200/ JCO.2013.54.6119.
- Sharma P, López-Tarruella S, García-Saenz JA, et al. Efficacy of neoadjuvant carboplatin plus docetaxel in triple negative breast cancer: combined analysis of two cohorts.Clin Cancer Res. 2017;23(3):649-657. doi: 10.1158/1078-0432.CCR-16-0162.
- Sharma P, Kimler B, Ward C, et al. Prognosis of triple negative breast cancer patients who attain pathological complete response with neoadjuvant carboplatin/docetaxel and do not receive adjuvant anthracycline chemotherapy.J Clin Oncol.2016;34(Suppl_15; abstr 1015). DOI: 10.1200/JCO.2016.34.15_suppl.1015.)
- Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27.J Clin Oncol.2008;26(5):778-785. doi: 10.1200/JCO.2007.15.0235.
- Gradishar WJ, Tjulandin S, Davidson N, et al. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oilbased paclitaxel in women with breast cancer.J Clin Oncol.2005;23(31):7794-7803.
- Gianni L, Mansutti M, Anton A, et al. ETNA (Evaluating Treatment with Neoadjuvant Abraxane) randomized phase III study comparing neoadjuvant nab-Paclitaxel (nab-P) versus Paclitaxel (P) both followed by anthracycline regimens in women with HER2-negative high-risk breast cancer: a Michelangelo study (in collaboration with GEICAM and BCRC-WA).J Clin Oncol.2016;34(suppl 15; abstr 502).
- Untch M, Jackisch C, Schneeweiss A, et al; Arbeitsgemeinschaft Gynäkologische OnkologieBreast (AGO-B) Investigators. Nab-paclitaxel versus solvent-based paclitaxel in neoadjuvant chemotherapy for early breast cancer (GeparSepto—GBG 69): a randomised, phase 3 trial.Lancet Oncol.2016;17(3):345-356. doi: 10.1016/S1470-2045(15)00542-2.
- Miller K, Wang M, Gralow J, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer.N Engl J Med. 2007;357(26):2666-2676.
- Miles DW, Chan A, Dirix LY, et al. Phase III study of bevacizumab plus docetaxel compared with placebo plus docetaxel for the first-line treatment of human epidermal growth factor receptor 2negative metastatic breast cancer.J Clin Oncol.2010;28(20):3239-3247. doi: 10.1200/JCO.2008.21.6457.
- Li Q, Yan H, Zhao P, et al. Efficacy and safety of bevacizumab combined with chemotherapy for managing metastatic breast cancer: a meta-analysis of randomized controlled trials.Sci Rep.2015;5:15746. doi: 10.1038/srep15746.
- Miles DW, Diéras V, Cortés J, et al. First-line bevacizumab in combination with chemotherapy for HER2-negative metastatic breast cancer: pooled and subgroup analyses of data from 2447 patients.Ann Oncol.2013;24(11):2773-2780. doi: 10.1093/annonc/mdt276.
- Robert NJ, Diéras V, Glaspy J, et al. RIBBON-1: randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2negative, locally recurrent or metastatic breast cancer.J Clin Oncol. 2011;29(10):1252-1260. doi: 10.1200/JCO.2010.28.0982.
- Cameron D, Brown J, Dent R, et al. Adjuvant bevacizumab-containing therapy in triple-negative breast cancer (BEATRICE): primary results of a randomised, phase 3 trial.Lancet Oncol.2013;14(10):933-942. doi: 10.1016/S1470-2045(13)70335-8.
- Gerber B, Loibl S, Eidtmann H, et al; German Breast Group Investigators. Neoadjuvant bevacizumab and anthracyclinetaxane-based chemotherapy in 678 triple-negative primary breast cancers; results from the geparquinto study (GBG 44).Ann Oncol. 2013;24(12):2978-2984. doi: 10.1093/annonc/mdt361.
- Bear HD, Tang G, Rastogi P, et al. Bevacizumab added to neoadjuvant chemotherapy for breast cancer.N Engl J Med. 2012;366(4):310-320. doi: 10.1056/NEJMoa1111097.
- Bear HD, Tang G, Rastogi P, et al. Neoadjuvant plus adjuvant bevacizumab in early breast cancer (NSABP B-40 [NRG Oncology]): secondary outcomes of a phase 3, randomised controlled trial.Lancet Oncol.2015;16(9):1037-1048. doi: 10.1016/ S1470-2045(15)00041-8.
- Earl HM, Hiller L, Dunn J, et al; ARTemis Investigators Group. Disease-free (DFS) and overall survival (OS) at 3.4 years (yrs) for neoadjuvant bevacizumab (Bev) added to docetaxel followed by fluorouracil, epirubicin and cyclophosphamide (D-FEC), for women with HER2 negative early breast cancer: the ARTemis trial.Ann Oncol.2017;28(8):1817-1824. doi: 10.1093/annonc/mdx173.
- Earl HM, Hiller L, Dunn JA, et al; ARTemis Investigators. Efficacy of neoadjuvant bevacizumab added to docetaxel followed by fluorouracil, epirubicin, and cyclophosphamide, for women with HER2-negative early breast cancer (ARTemis): an open-label, randomised, phase 3 trial.Lancet Oncol.2015;16(6):656-666. doi: 10.1016/S1470-2045(15)70137-3.
- Joensuu H, Kellokumpu-Lehtinen P-L, Huovinen R, et al. Adjuvant capecitabine, docetaxel, cyclophosphamide, and epirubicin for early breast cancer: final analysis of the randomized FinXX trial.J Clin Oncol. 2012;30(1):11-18. doi: 10.1200/JCO.2011.35.4639.
- O’Shaughnessy J, Koeppen H, Xiao Y, et al. Patients with slowly proliferative early breast cancer have low five-year recurrence rates in a phase III adjuvant trial of capecitabine.Clin Cancer Res. 2015;21(19):4305-4311. doi: 10.1158/1078-0432. CCR-15-0636.
- Martín M, Ruiz Simón A, Ruiz Borrego M, et al. Epirubicin plus cyclophosphamide followed by docetaxel versus epirubicin plus docetaxel followed by capecitabine as adjuvant therapy for node-positive early breast cancer: results from the GEICAM/2003-10 Study.J Clin Oncol.2015;33(32):3788-3795. doi: 10.1200/JCO.2015.61.9510.
- Zhimin S, Li J, Pang D, et al. Cbcsg-10: adjuvant capecitabine in combination with docetaxel and cyclophosphamide plus epirubicin for triple negative breast cancer.J Clin Oncol.2016;34(suppl 15; abstr 1012).
- Masuda N, Lee S-J, Ohtani S, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy.N Engl J Med. 2017;376(22):2147-2159. doi: 10.1056/ NEJMoa1612645.
- von Minckwitz G, Kümmel S, Vogel P, et al; German Breast Group. Neoadjuvant vinorelbinecapecitabine versus docetaxel–doxorubicin–cyclophosphamide in early nonresponsive breast cancer: phase III randomized GeparTrio trial.J Natl Cancer Inst.2008;100(8):542-551. doi: 10.1093/jnci/djn085.
- von Minckwitz G, Rezai M, Loibl S, et al. Capecitabine in addition to anthracyclineand taxane-based neoadjuvant treatment in patients with primary breast cancer: phase III GeparQuattro study.J Clin Oncol.2010;28(12):2015-2023. doi: 10.1200/ JCO.2009.23.8303.
- Nanda R, Liu MC, Yau C, et al. Pembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): results from I-SPY 2.J Clin Oncol. 2017;35(suppl 15; abstr 506).
- Neoadj Pembrolizumab + Decitabine Followed by Std Neoadj Chemo for Locally Advanced HER2- Breast Ca (NCT02957968). https://clinicaltrials.gov/ct2/show/ NCT02957968. Updated October 20, 2017. Accessed December 20, 2017.
- Pusztai L. Pembrolizumab in Treating Patients With Triple-Negative Breast Cancer (NCT02954874). https://clinicaltrials.gov/ct2/show/NCT02954874. Updated December 20, 2017. Accessed December 20, 2017.