Investigations of Targeted Therapies for NRG1 Fusion–Positive Cancers
The recent discovery and characterization of neuregulin 1 (NRG1) fusions as actionable genomic events in patients with advanced metastatic cancer have paved the way to further exploration of their potential usefulness in the personalized treatment of patients with NRG1 fusion–positive malignancies.1 Based upon the mechanistic understanding of the oncogenic driver role of NRG1 fusions via autocrine and paracrine signaling, early proof-of-concept and case-based studies investigated the viability of targeting HER2/HER3 (ERBB2/ERBB3) to treat NRG1 fusion–positive cancers.2-15 The results of these studies and preclinical trials showed that use of targeted agents could be an effective therapeutic strategy for tumors that harbor NRG1 fusions. Consequently, several studies were launched to further explore investigational HER-targeted agents and those approved by the FDA to treat NRG1 fusion–positive cancers; key trials are listed in the Table.16-23
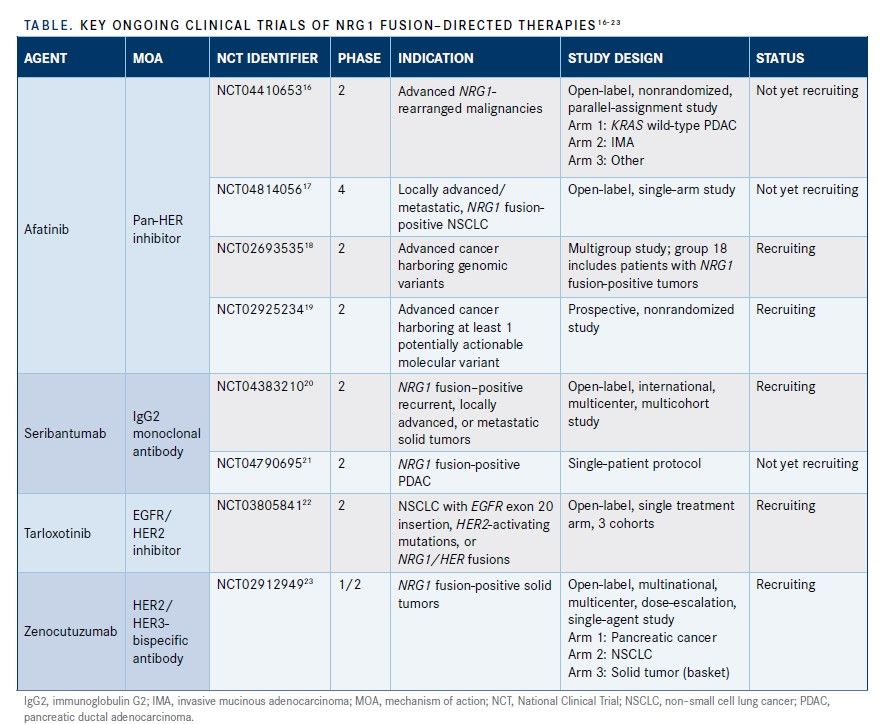
This article will detail the mechanisms of action of key HER-targeted agents
and present the results of preclinical and case-based studies of therapeutics being tested for safety and efficacy in phase 2 and 3 clinical trials involving patients with NRG1 fusion–positive cancers. This discussion will include the potential of these agents to expand the therapeutic landscape and provide new, personalized treatment options for this patient population.
Afatinib
Afatinib is indicated for the first-line treatment of patients with metastatic non–small cell lung cancer (NSCLC) whose tumors have nonresistant EGFR mutations as detected by an FDA-approved test. It is also indicated for the treatment of patients with metastatic NSCLC whose disease has progressed after administration of platinum-based chemotherapy.24
Afatinib binds to HER2 and HER4, which are kinase domains of EGFR. This binding irreversibly inhibits tyrosine kinase autophosphorylation, which downregulates EGFR signaling. Certain EGFR mutations can result in autophosphorylation of the EGFR receptor and its overactivation, which, in the absence of ligand binding, can support cell proliferation in NSCLC. In vitro, afatinib inhibited autophosphorylation and/or proliferation of cell lines expressing wild-type and mutated EGFR; it also inhibited proliferation of cell lines that overexpress HER2.24
Because NRG1 fusions trigger HER3 receptor overactivation, the proven efficacy of afatinib as a pan-HER inhibitor prompted investigation of its potential antitumor activity in NRG1 fusion‒positive cancers.25
Real-World, Retrospective TrialStudies of Patients With NRG1 Fusion–Positive Cancers
A real-world, retrospective chart review study (NCT04750824) evaluated the efficacy of afatinib following immunotherapy in patients who are given a diagnosis of NRG1 fusion–positive metastatic squamous cell lung cancer who received at least 1 line of systemic therapy between January 2017 and March 2020.26
The primary outcome measures are the proportion of patients who had a complete response (CR) or partial response (PR); secondary outcome measures include duration of clinical benefit (defined as time from initial response for any patient with CR, PR, or stable disease [SD] until progression or death) and duration of response (DOR), defined as time from initial CR or PR until earliest disease progression or death.25
The final results of this study have not been published, but the results of a feasibility assessment by Gajra et al of the subgroup of patients with NSCLC were published in 2021.26,27 As part of this assessment, physicians based in the United States who are part of the Cardinal Health Oncology Provider Extended Network retrospectively abstracted data from the medical records of adult patients with NRG1 fusion–positive solid tumors. Patients were divided into cohorts based on whether they received afatinib during previous lines of therapy or only other systemic therapies. Subgroup analysis was conducted for patients having NSCLC as the primary tumor type. Representatives of Cardinal Health reviewed data and provided summaries using descriptive statistics.27
Of the 107 patients in the study, 49 patients (46.0%) had NSCLC; 26 of these patients had received afatinib therapy. The most common NRG1 fusion partners identified among these patients were CD74 (n = 12 [24.5%]) and SCD4 (n = 9 [18.0%]). These data supported findings from previous studies, which showed that NRG1 fusions can be the primary tumor type in patients with NSCLC.27
Disease progressed following treatment with afatinib in 5 of the 26 patients (19.0%) who had received afatinib in the first-line through third-line therapeutic settings; among these patients, disease progression occurred in 2 patients following first-line therapy, 2 patients following second-line therapy, and 1 patient following third-line therapy. Among the 23 patients who received a treatment other than afatinib in the first- through third-line settings, 5 patients (21.7%) experienced disease progression (following first-line therapy, 3 patients; following second-line therapy, 2 patients).27
Seribantumab
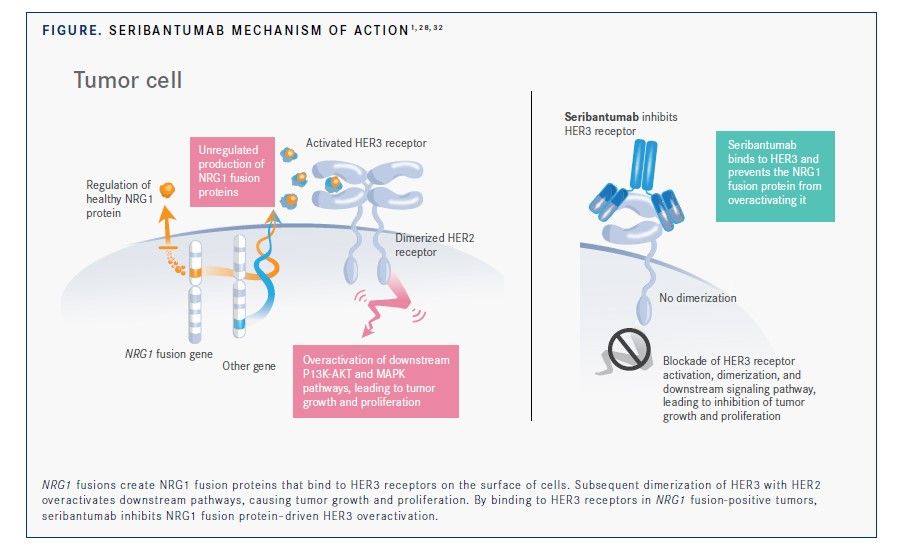
Most types of cancer are not driven by HER3 mutations or amplifications. Therefore, the effect of NRG1 fusions on HER3 activation demonstrates a novel HER3 dysregulation mechanism in cancer.28
Increased HER3 expression is associated with poor prognosis and resistance to chemotherapy. Also, increased expression of HER3 has been involved in resistance to HER2 inhibitors in HER2-amplified breast cancer and ovarian cancer. Furthermore, HER3 upregulation has been involved in resistance to EGFR inhibitors, endocrine therapy, and IGF1R inhibitors in patients with lung cancer, breast cancer, head and neck squamous cell carcinoma, and pancreatic cancer.29
Investigators have reported that HER3-dependent resistance mechanisms are mediated via activation of the PI3K/AKT, MAPK/ERK, and JAK/STAT pathways.30 However, the efficacy of most HER3-targeted therapies given alone was limited. Also, results of past studies of investigational HER3-targeted agents given with other targeted therapies showed limited clinical value due to unacceptable toxicity profiles or lack of meaningful clinical activity.31
Following the discovery of actionable NRG1 fusions that promote oncogenesis via activation of HER3-mediated 4 signaling, researchers hypothesized the HER3-targeted therapies could benefit patients with tumors harboring these genomic aberrations.2
Seribantumab (MM-121) is the first fully human, immunoglobulin G2 monoclonal antibody to receive a fast track designation by the FDA as an NRG1 inhibitor.31 Seribantumab targets HER3 receptors, inhibiting NRG1 fusion–mediated HER3 activation and subsequent signaling of the PI3K/AKT pathways (Figure).1,28,32 This activity inhibits continued proliferation and growth of NRG1 fusion–positive tumor cells.1,28,32
The FDA granted fast-track designation to seribantumab in 2016 for its development as a therapy in patients with NRG1–positive, locally advanced or metastatic NSCLC whose disease has progressed following immunotherapy. This designation was based on the results of the SHERLOC trial (NCT02387216).31
Preclinical Studies
In a preclinical study, Odinstov et al evaluated the potential efficacy of seribantumab in NRG1 fusion–positive gastrointestinal cancers. The investigators developed models of isogenic pancreatic cancer cells using lentiviral-mediated complementary DNA expression of ATP1B1-NRG1 and SLC3A2-NRG1 in immortalized human pancreatic ductal cells (H6C7); they then evaluated the efficacy of seribantumab in isogenic cell lines and in patient-derived xenograft (PDX) models of APP-NRG1–positive pancreatic ductal adenocarcinoma (PDAC)and RBPMS-NRG1–positive intrahepatic cholangiocarcinoma. The investigators used Western blotting analysis to evaluate protein phosphorylation and expression. Both reverse-transcription polymerase chain reaction and next-generation sequencing (NGS) were used to confirm the presence of NRG1 fusions.13
Treatment of ATP1B1-NRG1–positive and SLC3A2-NRG1–positive H6C7 pancreatic cells with seribantumab resulted in a dose-dependent blockade of HER3 and AKT phosphorylation. Administration of 5 mg or 10 mg of seribantumab twice weekly inhibited tumor growth in a PDX mouse model of PDAC that harbored APP-NRG1 fusions. Moreover, treatment with 2 doses of seribantumab resulted in tumor shrinkage of up to 55.0%; tumors treated with afatinib (5 mg/kg once daily) showed no shrinkage.13
Western blotting analysis of residual CTG-0943tumors following treatment with seribantumab demonstrated a total blockade of EGFR, HER2, and HER3 and cyclin D1 phosphorylation, which suggested effective suppression of the oncogenic signaling pathways activated by NRG1 fusions. These findings demonstrated the potential clinical activity of seribantumab as monotherapy in tumors driven by NRG1 fusions.13
Similar results were observed in another preclinical study that involved novel patient-derived and isogenic models of NRG1 fusion–positive tumors. In this study, seribantumab inhibited NRG1-mediated growth of MCF-7 cells, which do not harbor any NRG1 alterations. Seribantumab also inhibited the growth of cancer cells harboring NRG1 fusions, including DOC4-NRG1 in MDA-MB-175-VII cell lines and SLC3A2-NRG1 in LUAD-0061AS3 cell lines. The growth of HCC95 cancer cells with NRG1 amplification also was inhibited by seribantumab.15
Seribantumab induced cellular apoptosis of MDA-MB-175-VII and LUAD-0061AS3 cells as determined by the induction of caspase 3/7 activity. Induction of proapoptotic proteins and reduced expression of the cell-cycle regulator cyclin D1 were also observed following seribantumab treatments. Seribantumab inhibited phosphorylation of EGFR, HER2, HER3, and HER4, as well as the known signaling mediators AKT and ERK1/2 in CD74-NRG1–positive tumor cells of MDA-MB-175-VII and LUAD-0061AS3 cell lines. Moreover, seribantumab treatment resulted in 50.0% to 100% suppression of tumor growth in mice bearing a LUAD-0061AS3 PDX.15
In contrast with afatinib, which inhibited tumor growth only when administered at high doses, all doses of seribantumab tested inhibited tumor growth. Use of seribantumab resulted in sustained tumor regression, whereas treatment with afatinib resulted in tumor regrowth. Similarly, seribantumab treatment induced tumor regression in OV-10-0050, an ovarian cancer PDX model harboring CLU-NRG1.15
CRESTONE Clinical Trial
Based on growing evidence that supports targeting HER3 in patients with NRG1 fusion–positive tumors and preclinical findings demonstrating the efficacy of seribantumab in NRG1 fusion–positive tumor models, seribantumab is being evaluated patients with locally advanced or metastatic solid tumors that harbor NRG1 fusions as part of CRESTONE (NCT04383210), an open-label, international, multicenter, phase 2 clinical trial.20,32,33
CRESTONE was designed as a tumor-agnostic trial to assess the efficacy and safety of seribantumab therapy in patients with NRG1 fusion–positive advanced or metastatic solid tumors that progress or are resistant to available treatment options.21,36 The CRESTONE trial is being conducted with registrational intent following an accelerated approval pathway.32,33
Eligibility criteria include diagnosis of advanced solid tumors harboring an NRG1 fusion with progression following standard-of-care treatment or lack of suitable treatment options. NRG1–fusion status at enrollment will be assessed using a molecular assay performed by a laboratory meeting the requirements of the Clinical Laboratory Improvement Amendments. NRG1–fusion status for patients in cohort 1 will be centrally confirmed using an RNA-based NGS assay.32,33
The primary end point is the objective response rate per RECIST v1.1. Secondary end points include duration of response, safety, progression-free survival, overall survival, and clinical benefit rate (defined as CR, disease progression, and SD after 24 weeks of treatment).20,32
The study has a multicohort design and sample collection, which will enable exploration of the clinical relevance of NRG1–fusion partners and assess the impact of prior therapies, including other HER-targeted agents. Investigators also will assess potential therapy resistance mechanisms.32 CRESTONE is currently open and enrolling patients. There are 25 to 30 planned sites in the United States.20,32
Tarloxotinib
Tarloxotinib is a pan-HER inhibitor that was developed as hypooxia-activated prodrug that releases as a potent irreversible active metabolite (tarloxotinib-E) under hypoxic conditions to preferentially deliver the active moiety to tumor vs normal cells.14
RAIN-701 Clinical Trial
The safety and efficacy of taloxotinib is being evaluated in RAIN (NCT03805841), a phase 2, open-label, single-treatment arm clinical trial in adult patients with NSCLC whose tumors test positive for EGFR exon 20 insertions (cohort A), HER2 mutations (cohort B), and NRG1 and HER fusions (cohort C). Participants must have experienced disease progression after platinum-based chemotherapy or other standard-of-care therapy and measurable disease according to RECIST v1.1 criteria. Exclusion criteria include other known oncogene driver mutations and other investigational therapy administered within 28 days or 5 half-lives.22
The primary outcome is objective response rate through study completion (an average of 10 months), as defined by the number of patients who obtain CR or PR.22 This trial is still recruiting participants. No results of studies in cohort C have been published to date.22
Zenocutuzumab
The oncogenic mechanism of NRG1 fusions is mainly mediated through the heterodimerization of HER2 and HER3, leading to sustained induction of oncogenic signaling pathways.30,34 For this reason, the investigational bispecific antibody zenocutuzumab (MCLA-128) was developed to target both HER2 and HER3 to antagonize NRG1 fusion activity.11
Zenocutuzumab uses a “dock and block” mechanism of action: it docks into HER2 and blocks the ability of HER3 to bind with NRG1 fusions to prevent the dimerization of HER3 and HER2. This mechanism of action disrupts the ability of NRG1 fusions to drive signaling for tumor growth and survival.14
On January 8, 2021, the FDA granted zenocutuzumab fast-track designation for the treatment of patients with metastatic NRG1 fusion-positive solid tumors whose disease has progressed following on standard-of-care therapy.35
Safety Run-in of Phase 2 Study in Patients With Metastatic Breast Cancer
A phase 2, open-label, multicenter, international study (NCT03321981) is currently investigating the safety and efficacy of zenocutuzumab used with chemotherapy in patients with HER2-positive metastatic breast cancer (MBC) and patients with locally advanced or MBC that is estrogen receptor–positive with low HER2 expression.36
Results of the safety run-in portion of this study, which included 28 patients with HER2-positive MBC, were published by Hamilton et al in 2020. Common adverse effects (AEs) of any grade included neutropenia (17 patients [61.0%]), diarrhea (17 patients [61.0%]), asthenia/fatigue (13 patients [46.0%]), and nausea (8 patients [29.0%]). Grade 3 or 4 neutropenia and diarrhea were experienced by 13 patients (46.0%) and 1 patient (4.0%), respectively.11
The investigators concluded that use of this triplet regimen was safe and well-tolerated and offered a manageable AE profile. They noted that the AE profile was mostly related to the chemotherapy component of the regimen.11
Clinical Proof-of-Concept Study in Patients With NRG1 Fusion-Positive Tumors
In a clinical proof-of-concept study, 29 patients with NRG1 fusion-positive tumors representing 8 different cancer types were identified. Of these patients, 3 who did not respond to chemotherapy were treated with zenocutuzumab at a dose of 750 mg intravenously every 2 weeks.9
A 52-year-old man with an ARP1B1-NRG1–positive PDAC with liver metastases, worsening fatigue, and weight loss was treated with zenocutuzumab; he experienced a rapid reduction of CA19-9, a tumor marker protein, from 262 U/mL to 56 U/mL, which indicated a reduction in tumor cells. An imaging test at 8 weeks of treatment revealed a PR of 44.0% according to RECIST v1.1 criteria.9
A 34-year-old man with ARP1B1-NRG1–positive PDAC with liver metastases and longstanding tumor-associated abdominal pain experienced rapid resolution of pain and normalization of CA19-9 from 418 U/mL to 11 U/mL with zenocutuzumab treatment. At 6 weeks, imaging revealed a 22.0% reduction in tumor diameter and lack of fluorodeoxyglucose avidity in the liver metastases.9
A patient with CD64-NRG1–positive NSCLC with brain metastases showed a rapid response to zenocutuzumab therapy; scans showed a PR of 33.0% according to RECIST v1.1 criteria and tumor shrinkage following 8 weeks of treatment, even though his disease progressed after 6 prior lines of therapy that included use of afatinib.9
These investigators currently are recruiting patients for a global, open-label, multicenter, dose-escalation, single-agent, phase 1/2 basket trial of zenocutuzumab for patients with NRG1 fusion–positive solid tumors (NCT02912949). The study will assess safety, tolerability, pharmacokinetics, pharmacodynamics, immunogenicity, and antitumor activity of zenocutuzumab.23
Conclusions
Advances in genomic technologies have advanced precision cancer medicine and its evolution towards development of tumor-agnostic therapies. Understanding the mechanism of NRG1-mediated oncogenesis via activation of HER2/HER3 heterodimerization has fueled considerable interest in development of HER-targeted therapies that can specifically inhibit the activity of NRG1 fusions in tumor cells.1,2,28,37
The results of future tumor-agnostic clinical trials could further validate the clinical activity of HER-targeted agents in NRG1 fusion–positive tumors, expand the treatment landscape, and provide more personalized options for several types of cancer that are unresponsive or resistant to treatment.4
References
1. Fernandez-Cuesta L, Plenker D, Osada H, et al. CD74-NRG1 fusions in lung adenocarcinoma. Cancer Discov. 2014;4(4):415-422. doi:10.1158/2159-8290.CD-13-0633
2. Drilon A, Somwar R, Mangatt BP, et al. Response to ERBB3-directed targeted therapy in NRG1-rearranged cancers. Cancer Discov. 2018;8(6):686-695. doi:10.1158/2159-8290.CD-17-1004
3. Fernandez-Cuesta L, Thomas RK. Molecular pathways: targeting NRG1 fusions in lung cancer. Clin Cancer Res. 2015;21(9):1989-1994. doi:10.1158/1078-0432.CCR-14-0854
4. Jones MR, Lim H, Shen Y, et al. Successful targeting of the NRG1 pathway indicates novel treatment strategy for metastatic cancer. Ann Oncol. 2017;28(12):3092-3097. doi:10.1093/annonc/mdx523
5. Gay ND, Wang Y, Beadling C, et al. Durable response to afatinib in lung adenocarcinoma harboring NRG1 gene fusions. J Thorac Oncol. 2017;12(8):e107-e110. doi:10.1016/j.jtho.2017.04.025
6. Cheema PK, Doherty M, Tsao MS. A case of invasive mucinous pulmonary adenocarcinoma with a CD74-NRG1 fusion protein targeted with afatinib. J Thorac Oncol. 2017;12(12):e200-e202. doi:10.1016/j.jtho.2017.07.033
7. Heining C, Horak P, Uhrig S, et al. NRG1 fusions in KRAS wild-type pancreatic cancer. Cancer Discov. 2018;8(9):1087-1095. doi:10.1158/2159-8290.CD-18-0036
8. Laskin JJ, Cadranel J, Renouf DJ, et al. Afatinib as a novel potential treatment option for NRG1 fusion-positive tumors. J Global Oncol. 2019;5(suppl):110. doi:10.1200/JGO.2019.5.suppl.110
9. Schram AM, O’Reilly EM, Somwar R, et al. Clinical proof of concept for MCLA-128, a bispecific HER2/3 antibody therapy, in NRG1 fusion-positive cancers. Mol Cancer Ther. 2019;18(suppl 12):PR02. doi:10.1158/1535-7163.TARG-19-PR02
10. Tirunagaru VG, Estrada-Bernal A, Yu H, et al. Tarloxotinib exhibits potent activity in NRG1 fusion and rearranged cancers. Cancer Res. 2019;79(suppl 13):2202. doi:10.1158/1538-7445.AM2019-2202
11. Hamilton EP, Petit T, Pistilli B, et al. Clinical activity of MCLA-128 (zenocutuzumab), trastuzumab, and vinorelbine in HER2 amplified metastatic breast cancer (MBC) patients (pts) who had progressed on anti-HER2 ADCs. J Clin Oncol. 2020;38(suppl15):3093. doi:10.1200/JCO.2020.38.15_suppl.3093
12. Sequist LV, Gray JE, Harb WA, et al. Randomized phase II trial of seribantumab in combination with erlotinib in patients with EGFR wild-type non-small cell lung cancer. Oncologist. 2019;24(8):1095-1102. doi: 10.1634/theoncologist.2018-069
13. Odinstov I, Lui AJ, Bloom PR, et al. Preclinical activity of seribantumab in gastrointestinal cancers with NRG1 fusions. Cancer Res. 2021:81(suppl 13):935.doi:10.1158/1538-7445.AM2021-935
14. Liu SV, Villacruz LC, Lee VHF, et al. LBA61 First analysis of RAIN-701: study of tarloxotinib in patients with non-small cell lung cancer (NSCLC) EGFR exon 20 insertion, HER2-activating mutations & other solid tumours with NRG1/ERBB gene fusions. Ann Oncol. 2020;(suppl 4):S1189. doi:10.1016/jannonc.2020.08/2294
15. Odinstov I, Lui AJ, Sisso WJ, et al. The anti-HER3 mAb seribantumab effectively inhibits growth of patient-derived and isogenic cell line and xenograft models with oncogenic NRG1 fusions. Clin Cancer Res. 2021;81(11):3154-3166. doi:10.1158/1078-0432.CCR-20-3605
16. Afatinib in advanced NRG1-rearranged malignancies. ClinicalTrials.gov. Updated April 13, 2021. Accessed August 26, 2021. https://clinicaltrials.gov/ct2/show/NCT04410653
17. To evaluate the efficacy of afatinib in the treatment of locally advanced/metastatic non-small cell lung cancer with NRG1 Fusion. ClinicalTrials.gov. Updated April 1, 2021. Accessed August 26, 2021. https://clinicaltrials.gov/ct2/show/NCT04814056
18. TAPUR: testing the use of Food and Drug Administration (FDA) approved drugs that target a specific abnormality in a tumor gene in people with advanced stage cancer (TAPUR). ClinicalTrials.gov. Updated August 25, 2021. Accessed September 15, 2021. https://clinicaltrials.gov/ct2/show/record/NCT02693535
19. The drug rediscovery protocol (DRUP Trial) (DRUP). ClinicalTrials.gov. Updated March 11, 2021. Accessed August 16, 2021. https://clinicaltrials.gov/ct2/show/record/NCT02925234
20. Study of seribantumab in adult patients with NRG1 gene fusion positive advanced solid tumors. ClinicalTrials.gov. Updated August 3, 2021. Accessed August 16, 2021. https://www.clinicaltrials.gov/ct2/show/NCT04383210
21. Single patient protocol for an NRG1 fusion positive metastatic pancreatic cancer patient using seribantumab. Updated March 10, 2021. Accessed September 13, 2021. https://clinicaltrials.gov/ct2/show/NCT04790695
22. Study of tarloxotinib in pts with NSCLC (EGFR exon 20 insertion, HER2-activating mutations) & other solid tumors with NRG1/ERBB gene fusions (RAIN). ClinicalTrials.gov. Updated August 12, 2020. Accessed August 26, 2021. https://clinicaltrials.gov/ct2/show/NCT03805841
23. A study of zenocutuzumab (MCLA-128) in patients with solid tumors harboring an NRG1 fusion. ClinicalTrials.gov. Updated January 12, 2021. Accessed August 16, 2021. https://clinicaltrials.gov/ct2/show/record/NCT02912949
24. Gilotrif. Prescribing information. Boehringer Ingelheim; 2019.
Accessed August 16, 2021. https://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Gilotrif/Gilotrif.pdf?DMW_FORMAT=pdf
25. Jones MR, Williamson LM, Topham JT, et al. NRG1 gene fusions are recurrent, clinically actionable gene rearrangements in KRAS wild-type pancreatic ductal adenocarcinoma. Clin Cancer Res. 2019;25(15):4674-4681. doi:10.1158/1078-0432.CCR-19-0191
26. Real-world effectiveness of afatinib (Gilotrif) following immunotherapy in the treatment of metastatic, squamous cell carcinoma of the lung: a multi-site retrospective chart review study in the U.S. ClinicalTrials.gov. Updated March 9, 2021. Accessed September 13, 2021. https://clinicaltrials.gov/ct2/show/NCT04750824
27. Gajra A, Klink AJ, Kaufman J, et al. A real-world feasibility study of patients with solid tumors harboring NRG1 gene fusions: NSCLC subset analysis. J Thorac Oncol. 2021;16(3):S676-S677. doi:https://doi.org/10.1016/j.jtho.2021.01.1240
28. Mota JM, Collier KA, Barros Costa RL, et al. A comprehensive review of heregulins, HER3, and HER4 as potential therapeutic targets in cancer. Oncotarget. 2017;8(51):89284-89306. doi:10.18632/oncotarget.18467
29. Jacob W, James I, Hasmann M, Weisser M. Clinical development of HER3-targeting monoclonal antibodies: perils and progress. Cancer Treat Rev. 2018;68:111-123. doi:10.1016/j.ctrv.2018.06.011
30. Mishra R, Patel H, Alanazi S, Yuan L, Garrett JT. HER3 signaling and targeted therapy in cancer. Oncol Rev. 2018;12(1):355. doi:10.4081/oncol.2018.355
31. FDA grants Merrimack fast track designation for seribantumab (MM-121) in non-small cell lung cancer. News release. July 6, 2016. Accessed September 13, 2021. https://www.prnewswire.com/news-releases/fda-grants-merrimack-fast-track-designation-for-seribantumab-mm-121-in-non-small-cell-lung-cancer-300294237.html
32. Hamilton E, Powell M, Thaker P, et al. CRESTONE: clinical study of response to seribantumab in tumors with neuregulin-1 (NRG1) fusions—a phase II study of the anti-HER3 mAb for advanced or metastatic solid tumors (NCT04383210). J Clin Oncol.2021;39(suppl 3):TPS449. doi:10.1200/JCO.2021.39.3_suppl.TPS449
33. Bendell JC, Lim KH, Burkhard ME, et al. CRESTONE: clinical study of response to seribantumab in tumors with neuregulin-1 (NRG1) fusions—a phase II study of the anti-HER3 mAb for advanced or metastatic solid tumors (NCT04383210). J Clin Oncol. 2021;39(suppl 3):TPS449
34. Russo A, Lopes AR, Scilla K, et al. NTRK and NRG1 gene fusions in advanced non-small cell lung cancer (NSCLC). Precis Cancer Med. 2020;3:14. doi:10.21037/pcm.2020.03.02
35. Merus granted FDA fast track designation of zenocutuzumab for the treatment of patients with neuregulin 1 fusion cancers. News release. Merus. January 7, 2021. Accessed September 14, 2021. https://ir.merus.nl/news-releases/news-release-details/merus-granted-fda-fast-track-designation-zenocutuzumab-treatment
36. MCLA-128 with trastuzumab/chemotherapy in HER2+ and with endocrine therapy in ER+ and low HER2 breast cancer. ClinicalTrials.gov. Updated August 26, 2021. Accessed September 13, 2021. https://clinicaltrials.gov/ct2/show/NCT03321981
37. Shin DH, Lee D, Hong DW, et al. Oncogenic function and clinical implications of SLC3A2-NRG1 fusion in invasive mucinous adenocarcinoma of the lung. Oncotarget. 2016;7(43):69450-69465. doi:10.18632/oncotarget.11913