George Explores Impact of Risk Status With Cabozantinib/Nivolumab in Advanced RCC
During a Case-Based Roundtable® event, Daniel George, MD, discussed the results of the CheckMate 9ER trial across favorable, intermediate, and poor risk groups in patients with advanced renal cell carcinoma.
Daniel George, MD
Eleanor Easley Distinguished Professor in the School of Medicine
Professor of Medicine
Professor in Surgery
Duke University School of Medicine
Member, Duke Cancer Institute
Durham, NC

CASE SUMMARY
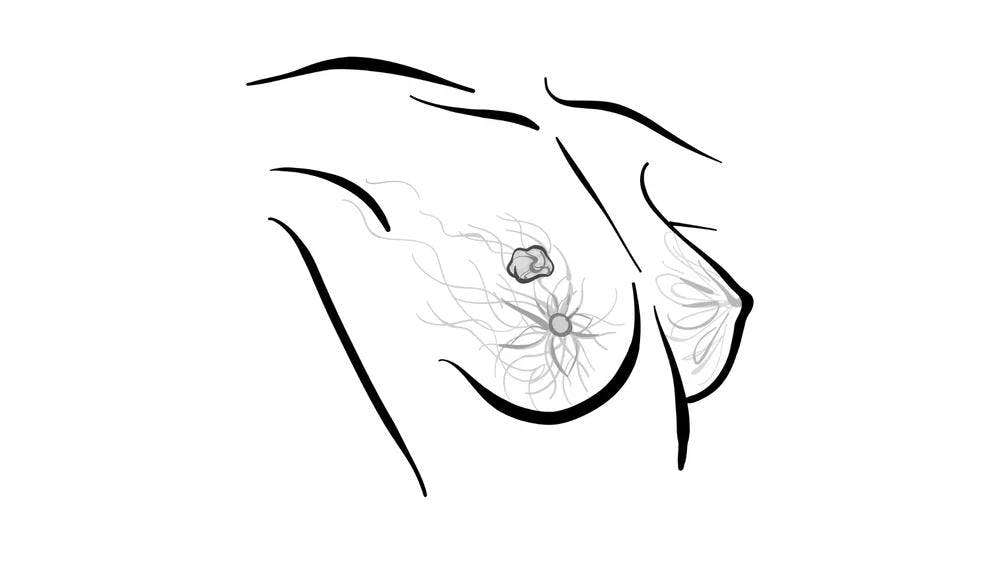
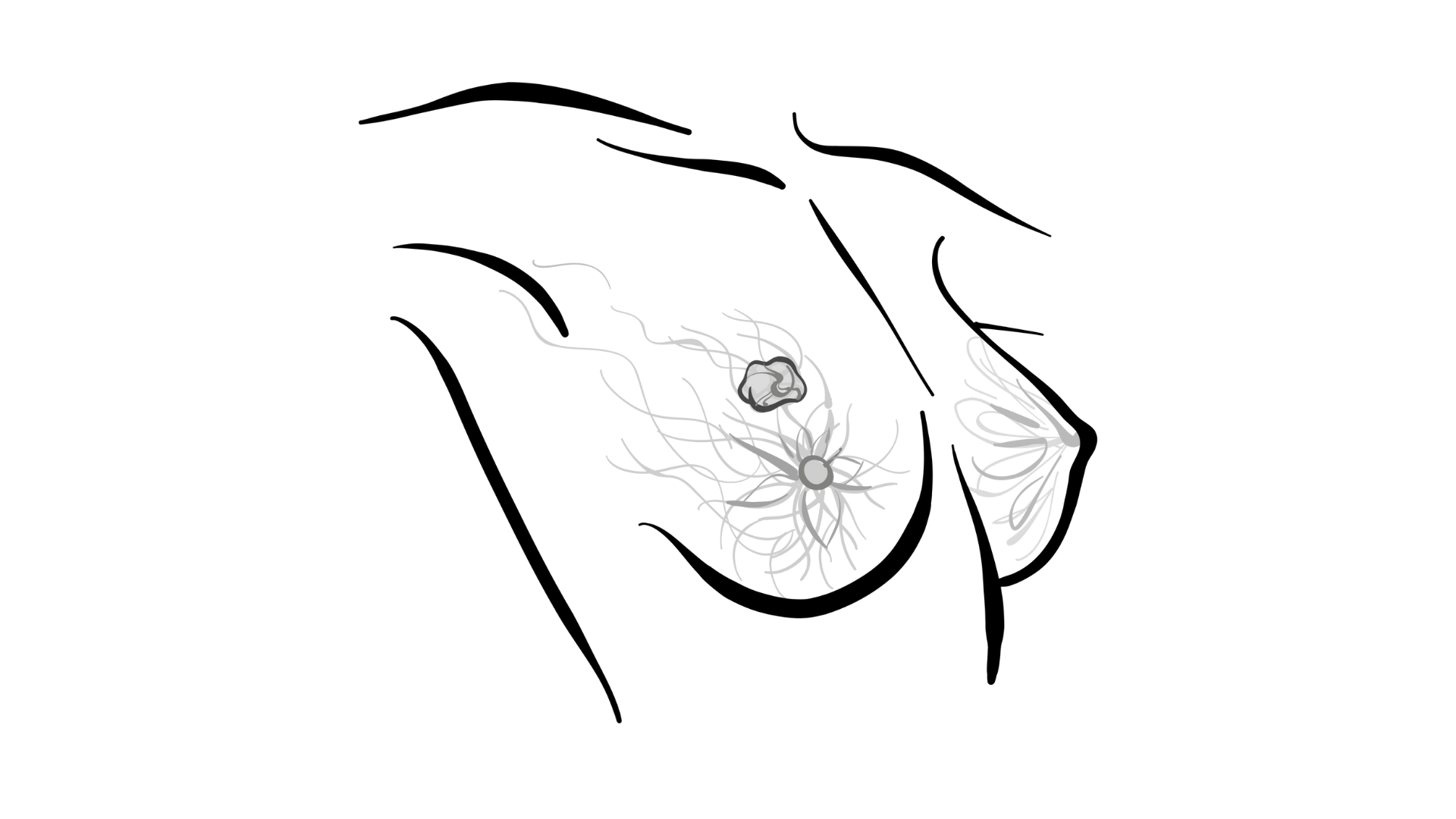
- A 61-year-old man, married, father of 2 grown children with 5 grandchildren who live nearby, lives an active lifestyle (daily walks, golfs regularly)
- History of low-volume, indolent metastatic clear cell renal cell carcinoma (ccRCC), status post left nephrectomy and adrenalectomy
- The patient was observed based on low volume and indolence of disease and patient preference .
- Three years after nephrectomy: continued indolent growth on scans, increased total tumor burden, new paratracheal lymph node (2.0 × 1.5 cm), and more than 10 pulmonary nodules on CT scan
- Lung biopsy confirmed metastatic ccRCC
- Laboratory values within normal limits and ECOG performance status of 0
PEERS & PERSPECTIVES IN ONCOLOGY: Could you describe the data that led to the approval of cabozantinib/nivolumab in patients with advanced ccRCC?
GEORGE: It is based on the CheckMate 9ER study [NCT03141177]. [It enrolled] 650 patients in an open-label fashion, [and the patients were] randomly assigned to cabozantinib [Cabometyx] plus nivolumab [Opdivo] or sunitinib [Sutent]. There was IMDC [International Metastatic RCC Database Consortium] risk score stratification. Most of the patients had intermediate/poor risk.1 The primary end point was progression-free survival [PFS]. The median follow-up for this analysis was 44 months, with a data lock [of May 27, 2022].
The primary end point was PFS in the intention-to-treat population, so all-comers [were included]. It is holding up over time, with a 16.6-month median PFS vs 8.4 months [with sunitinib at 44 months’ median follow-up; HR, 0.58; 95% CI, 0.48-0.71].1 When you go out to 3 years, you’ve still got 20% of patients responding with no progression on cabozantinib/nivolumab…vs just 11% with sunitinib, so there was a clear improvement in the entire population. These curves separate early, so even those rapidly progressing have a significant benefit, which persists all the way through the population.
When we look at overall survival [OS], it’s the same story. We see these curves separate early. Even within 12 to 18 months, there’s clear separation. We have a [10%] absolute difference in survival at 18 months [79.0% with cabozantinib/nivolumab vs 68.8% with sunitinib]. We have the same 10% improvement in OS at 36 months [58.7% vs 49.5%, respectively]. We have some censoring going on after that. We’ll have to get more follow-up. But this is an HR of 0.70 [95% CI, 0.56-0.87], and this is in the intention-to-treat [population, including] favorable and intermediate risk…. You can see a median OS improvement of 14 months, a dramatic improvement of more than a year in OS. There is a huge difference here that’s persisting throughout the population as we cross down to the median, and hopefully we’ll see further. This [was from the final analysis for] OS, but [data with a 55-month follow-up were presented in January].
If we look at [objective response rate (ORR)], we’re seeing a doubling of the overall response and a much higher CR [complete response] rate associated with [the combination]. There was a 12% CR rate vs 3.5% with sunitinib [in the intermediate/high-risk group].1 [In the intent-to-treat population], the ORR was almost 56%, and another 32% with stable disease, so only 6% with pure progressive disease from the start.2
How did the combination perform in particular subpopulations of the trial?
In the subgroup analysis for OS, everything has shifted over in favor of cabozantinib/nivolumab, and that’s the first thing I look at in these [data].3 Is there any group that’s not benefiting from this? The answer is no. Some groups probably benefit more than others. With liver metastasis, there’s a shift that suggests even greater benefit for that population [unstratified HR, 0.54; 95% CI, 0.34-0.87]. It is the same with bone metastases, although not quite as dramatic [HR, 0.63; 95% CI, 0.42-0.97]. There was [benefit regardless of stage at] initial presentation. With sarcomatoid feature, there was a huge difference. They’re rare; there are only 75 patients in the study, but the HR is 0.38 for that population [95% CI, 0.20-0.74]. Patients who have undergone a nephrectomy probably do better [HR, 0.62; 95% CI, 0.45-0.83]. When they haven’t undergone nephrectomy, this is a shorter-survival, poorer-risk population [HR, 0.87; 95% CI, 0.59-1.30]. But we see a shift slightly in favor [of] cabozantinib/ nivolumab for those who have, and most of our patients have undergone prior nephrectomy.
How did IMDC risk affect PFS and OS in patients receiving the combination?
For OS [by risk group], the intermediate/poor-risk population [showed] clear separation, with an even greater HR of 0.65 [95% CI, 0.51-0.83].1 When you look at the patients with favorable risk status, they’re doing better. At 36 months, there was a 68% OS rate with cabozantinib/nivolumab, but for the intermediate/poor-risk group, it was 55%. IMDC [risk status] is prognostic, but it’s not that huge [of] a difference. It was bigger when we were in the [single-agent] TKI [tyrosine kinase inhibitor] era, so it’s just showing that this is not as sensitive of a marker in this setting. If we looked at pure intermediate vs favorable risk, it would probably be even closer. With favorable risk, there is not much difference [between the arms because there were] not enough events. But the HR was [close to] 1.0 with wide CIs [HR, 1.07, 95% CI, 0.63-1.79].
If you look at PFS, it’s a different story. We’re seeing the separation there, but some of these patients [also] have long-term responses to sunitinib. In the intermediate/poor-risk groups, [there was] a much greater separation [HR, 0.55; 95% CI, 0.45-0.69]. If your patient has a higher burden, is more symptomatic, has more organ sites involved, and has anemia and elevated calcium, then we absolutely want to treat them with combination therapy.
At that 44-month follow-up, [the PFS and OS] are holding steady across the board [Table3,4]. When we see the breakdown, it’s even greater in the poor-risk group. That’s where our [single-agent] TKIs come up short. Patients [receiving sunitinib] do better in the favorable- and intermediate-risk groups, but we’re still seeing benefits associated with [the combination]. When we look at OS, that’s where we see the real separation with intermediate and poor risk. When we pull out the poor-risk group, that’s where we see the greatest percent benefits associated with this.

What was the impact of the site of metastasis?
If we look at certain organ sites, we can see some trends. For PFS, there was a huge difference for liver, bone, and even lung metastases.5 In patients with visceral organ sites, we’re seeing some dramatic differences. When we look at OS, it’s a smaller number of overall events. But particularly with liver metastases, we’re seeing great effects, so the hepatocyte growth factor/Met [tyrosine kinase] story is playing out here and in the bone. However, there were fewer patients with bone metastasis, so we’ll need to see how those curves continue to look, but there is a clear difference in OS. With lung metastases…these curves separate less dramatically than the other 2 but is still a strong [OS].
What is the significance of measuring time to subsequent therapy?
Time to subsequent therapy is a patient end point.… Change in therapy is stressful for patients; they don’t know how they’re going to tolerate it, how they’re going to respond, and whether it’s going to get covered [by insurance]. There’s a delay in between [when] there’s a risk of complications with progression. Time to subsequent therapy was…nice [median of 20.6 months].1 [After 2 years, they are] just on cabozantinib alone. Getting out to 12 months, more than half the patients were still stable and [the curve] seems to be flattening out. We would like to see more numbers, but it’s a nice curve for these long-term responders.
What tolerability concerns were there on this trial?
[Adverse events] are similar. If anything, there is a bit more elevation of rates of low-grade toxicities with sunitinib, like fatigue, nausea, some of the inflammation, and some of the cytopenias.1 The cabozantinib/nivolumab [combination has] higher [rates of] hypothyroidism, diarrhea, liver function test [elevation], and things like that, so it is a mix of [toxicity between the arms]. But most of it is low grade, grade 1, and grade 2. If you look at grade 3 [and higher], they’re similar between the 2 arms.
REFERENCES:
1. Burotto M, Powles T, Escudier B, et al. Nivolumab plus cabozantinib vs sunitinib for first-line treatment of advanced renal cell carcinoma (aRCC): 3-year follow-up from the phase 3 CheckMate 9ER trial. J Clin Oncol. 2023;41(suppl 6):603. doi:10.1200/JCO.2023.41.6_suppl.603
2. Powles T, Choueiri TK, Burotto M, et al. Final overall survival analysis and organ-specific target lesion assessments with two-year follow-up in CheckMate 9ER: nivolumab plus cabozantinib versus sunitinib for patients with advanced renal cell carcinoma. J Clin Oncol. 2022;40(suppl 6):350. doi:10.1200/JCO.2022.40.6_suppl.350
3. Motzer RJ, Powles T, Burotto M, et al. Nivolumab plus cabozantinib versus sunitinib in first-line treatment for advanced renal cell carcinoma (CheckMate 9ER): long-term follow-up results from an open-label, randomised, phase 3 trial. Lancet Oncol. 2022;23(7):888-898. doi:10.1016/S1470-2045(22)00290-X
4. Erratum: nivolumab plus cabozantinib vs sunitinib for first-line treatment of advanced renal cell carcinoma (aRCC): 3-year follow-up from the phase 3 CheckMate 9 ER trial. J Clin Oncol. 2023;41(21):3767. doi:10.1200/JCO.23.00901
5. Apolo AB, Powles T, Burotto M, et al. Nivolumab plus cabozantinib (N+C) versus sunitinib (S) for advanced renal cell carcinoma (aRCC): outcomes by baseline disease characteristics in the phase 3 CheckMate 9ER trial. J Clin Oncol. 2021;39(suppl 15):4553. doi:10.1200/JCO.2021.39.15_suppl.4553

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen