Durvalumab Misses Primary End Point in Early-Stage NSCLC
Durvalumab did not significantly improve disease-free survival in patients with early-stage non–small cell lung cancer following resection.
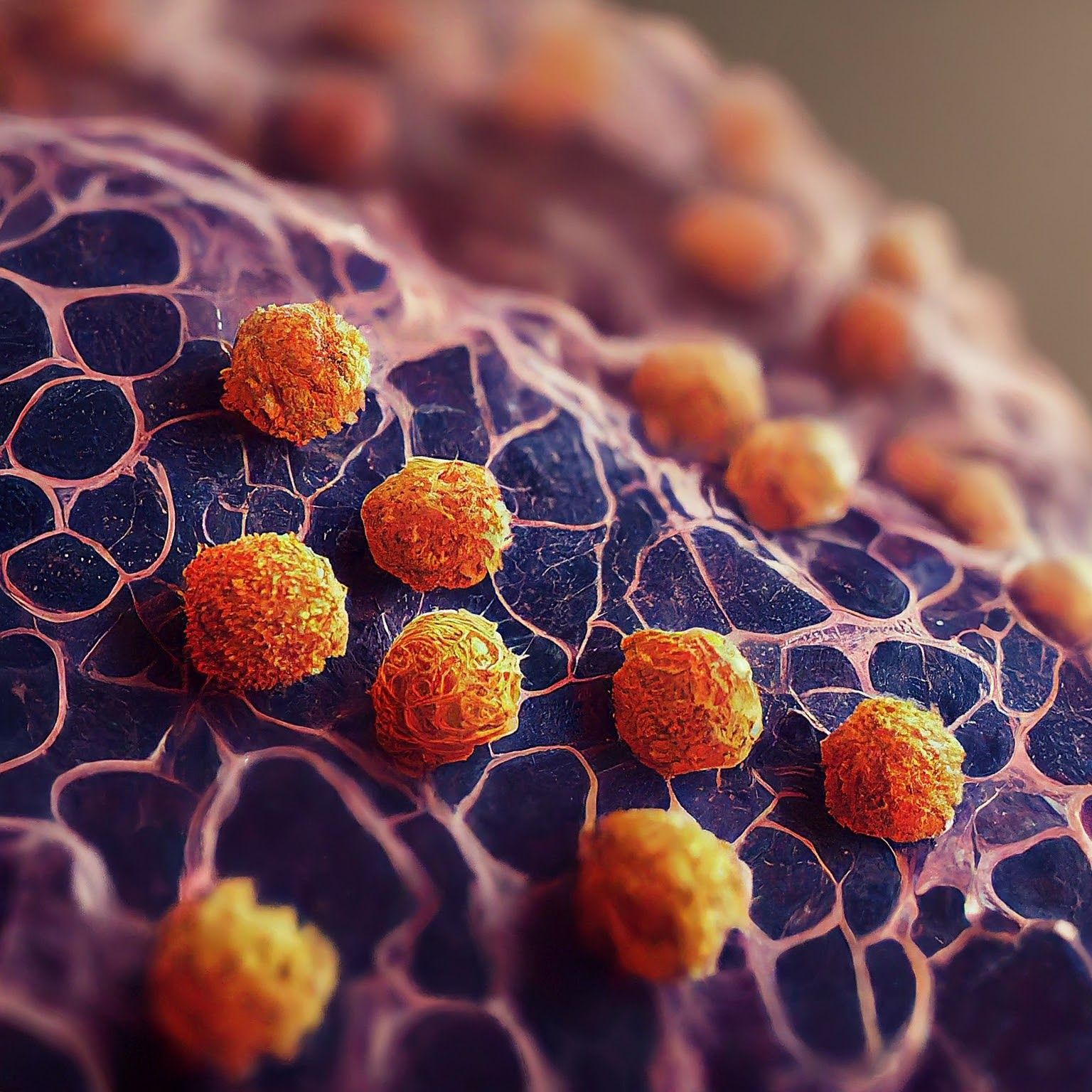
Microscopic image of non-small cell lung cancer - Generated with Google Gemini AI
Durvalumab (Imfinzi) did not lead to a statistically significant improvement in the primary end point of disease-free survival (DFS) vs placebo in early-stage non–small cell lung cancer (NSCLC) after complete tumor resection in tumors that express PD-L1 on 25% or more of cells, according to an analysis of the ADJUVANT BR.31 (NCT02273375) study.1
“We are disappointed in the ADJUVANT BR.31 results. [Durvalumab] has helped change the treatment landscape and achieved multiple positive phase 3 trials for patients with earlier stages of lung cancer. We are committed to addressing the remaining unmet need in lung cancer through our broad development program," said Susan Galbraith, executive vice president of oncology research and development at AstraZeneca, in a press release.
In November 2023, the phase 3 PACIFIC-2 study (NCT0351997) of concurrent durvalumab and chemoradiotherapy missed its primary end point of progression-free survival (PFS) vs chemoradiotherapy alone in unresectable, stage III NSCLC.2
Durvalumab is the only approved immunotherapy in the curative intent setting of unresectable stage III NSCLC in patients who did not experience disease progression following chemoradiotherapy, based on the phase 3 PACIFIC trial (NCT02125461). Several other PACIFIC trials are investigating durvalumab in other NSCLC settings, including PACFIC-4 (NCT03833154) in patients with medically inoperable, early-stage NSCLC. The PACIFIC-5 (NCT03706690), PACIFIC-8 (NCT05211895), and PACIFIC-9 (NCT05221840) trials are looking at durvalumab in unresectable stage III NSCLC.1
About ADJUVANT BR.31
ADJUVANT BR.31 is a randomized, multicenter, double-blind, phase 3 trial sponsored by the Canadian Cancer Trials Group. A total of 1415 patients with stage IB (≥4cm), II, or IIIA NSCLC following complete tumor resection with or without adjuvant chemotherapy were randomized 2:1 to receive 20 mg/kg intravenous infusion of durvalumab or placebo every 4 weeks for up to 48 weeks.1
DFS for patients with NSCLC that is PD-L1 expression in tumor cells ≥ 25% and patients without common activating EGFR mutations or ALK gene rearrangements was the primary end point. Secondary end points included DFS in other patient subpopulations, overall survival, incidence of adverse events, quality of life, and cost effectiveness.3
A total of 269 centers across 19 countries and regions, including in Canada, the US, Australia, Europe and Asia, enrolled patients.1 To be eligible for enrollment, patients were not permitted to have neoadjuvant chemotherapy or prior anticancer therapy for NSCLC other than postoperative adjuvant chemotherapy. Patients were also required to have an ECOG status of 0 or 1 and adequate hematologic and laboratory levels.3