Durable Responses Are Observed With Cemiplimab in mBCC
Rate for objective response and stable disease were encouraging, according to findings from a phase 2 trial evaluating the PD-1 inhibitor, cemiplimab-rwlc.
Karl Lewis, MD

Rate for objective response and stable disease were encouraging, according to findings from a phase 2 trial (NCT03132636) evaluating the PD-1 inhibitor, cemiplimab-rwlc (Libtayo). This antitumor activity included responses that were durable and safe in patients with metastatic basal cell carcinoma (mBCC) after progression on or intolerance to hedgehog inhibitors. Interim results were presented ahead of the 35th Annual Meeting & Pre-Conference Programs of the Society for Immunotherapy of Cancer (SITC 2020).
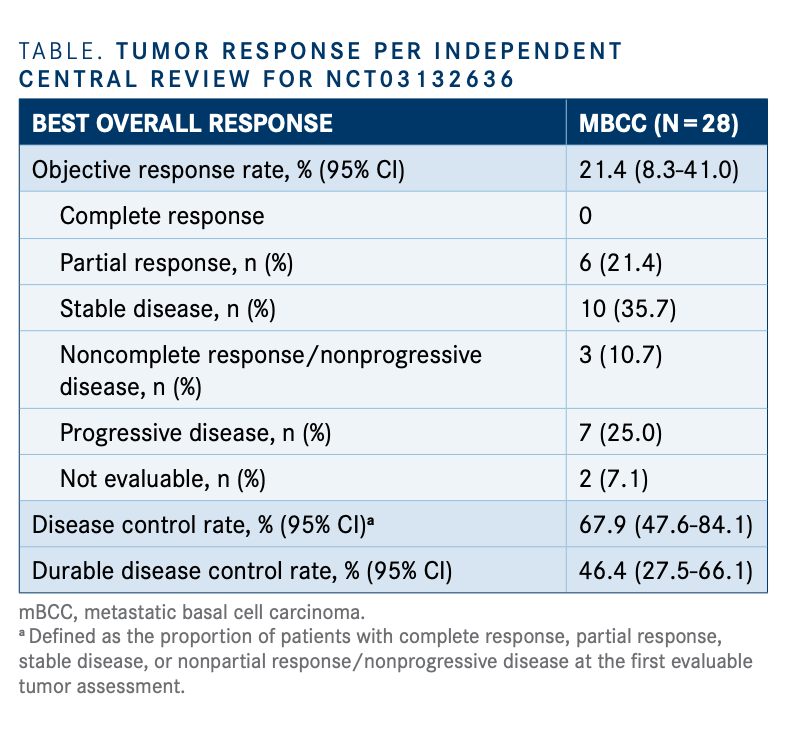
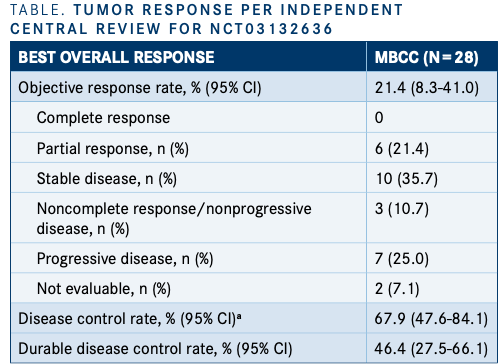
Among 28 patients, the objective response rate (ORR) per independent central review (ICR) was 21.4% (n = 6; 95% CI, 8.3%-41.0%), which consisted of all partial responses (PRs). The stable disease (SD) rate was 35.7% (n =10), which translated to a disease control rate (DCR) of 67.9%, defined as the proportion of patients with complete response (CR), PR, SD, or nonprogressive disease at first assessment (95% CI, 47.6%-84.1%) (TABLE).
“There have been case reports with cemiplimab, but this is the first prospective study in any meaningful number of patients. The activity and durability [of the agent] seem to be promising,” Karl Lewis, MD, lead study author and professor of medicine-medical oncology at the Colorado School of Medicine, said in a virtual press briefing ahead of SITC 2020, which was held virtually.
Basil cell carcinoma (BCC) is the most common type of skin cancer, and ultraviolet exposure is a significant risk factor. The majority of patients with advanced BCC undergo curative surgery. However, systemic therapy is also available for patients with advanced disease who are ineligible for curative surgery or radiation.
Vismodegib (Erivedge) and sonidegib (Odomzo) are oral hedgehog inhibitors approved for patients with locally advanced or mBCC. However, no FDA-approved treatment options are available to patients who progress on or are intolerant to hedgehog inhibitors.
Cemiplimab is the first systemic therapy that has shown clinical benefit in patients with locally advanced and mBCC after treatment with hedgehog inhibitors. The first demonstration was reported in findings from the locally advanced cohort of this phase 2 study presented during the European Society for Medical Oncology Virtual Congress 2020.
The phase 2 study enrolled 2 cohorts: group 1 con-sisted of patients with nodal and distant mBCC and group 2 of patients with locally advanced BCC (n=84).The mBCC cohort included patients followed for approx-imately 57 weeks to provide an ORR with a 95% CI.
Patients received 350 mg of intravenous cemiplimab every 3 weeks for up to 93 weeks. Tumor assessments were performed from days 1 to 5 every 9 weeks and from days 6 to 9 every 12 weeks thereafter. Tumor response assessment was measured by ICR using RECIST 1.1 criteria for visceral lesions or modified World Health Organization criteria for skin lesions.
ORR per ICR served as the primary end point of the study. Secondary end points included ORR by investi-gator review, progression-free survival (PFS), PFS by ICR and investigator review, overall survival, CR rate by ICR, and safety and tolerability of cemiplimab.
Regarding prior therapy in the mBCC cohort, 100% of patients received vismodegib (n=28),10.7% (n=3) received sonidegib (Odomzo), and 10.7% (n=3) received vismodegib and sonidegib.Reasons for discontinuation of prior therapy includ-ed disease progression on hedgehog inhibitor therapy (75.0%; n=21); prior hedgehog inhibitorintolerance (35.7%; n=10), predominantly forvismodegib (39.3%; n=11) versus sonidegib (7.1%; n=2); and SD as best response after 9 months on hedgehog inhibitor therapy (17.9%; n=5).
Twenty-five percent of patients (n=7) experi-enced progressive disease. Less than 10% of patients (7.1%; n=2) were not evaluable.
The median duration of response (DOR) had not been reached at the time of data cutoff. The 6- and 12-month DOR estimates for patients with response were 100% (95% CI, 68.3%-97.6%) and 66.7% (95% CI, 19.5%-90.4%), respectively.
The safety profile of cemiplimab was found to be consistent with prior reports of the agent in other tumor types. Any-grade treatment-related adverse effects (TRAEs) occurred in 78.6% of patients (n=22). Grade 3 or higherTRAEs were reported in 17.9% of patients (n=5), and 1 death from staphylococcal pneu-monia occurred, which was determined to be unrelated to study treatment.
The most common TRAEs were fatigue (25%; n=21), pruritus (14%; n=12), and asthenia(14%; n=12). The most common grade 3 orhigher TRAEs were fatigue (2%; n=2), colitis (2%; n=2), and autoimmune colitis (2%; n=2).Fourteen patients (17%) discontinued treatment due to any-grade TRAEs.
In previously presented findings of the locally advanced BCC cohort, cemiplimab led to an ORR of 31.0% (95% CI, 21.3%-42.0%), which included a 6% CR rate (n=5) and a 25.0% PR rate (n=21). Additionally, slightly less than half of patients (48.8%; n=41) achieved SD.
"In the locally advanced cohort, responses to [cemiplimab] seemed to be delayed. Unlike cuta-neous squamous cell carcinoma, for which cemi-plimab is approved [and] patients that respond seem to respond quickly, [there seems to be a time lag for] patients with basal cell carcinoma....Hopefully, with longer follow-up, this [21.4%] response rate might improve,” Lewis said.
In the locally advanced cohort, the median DOR per ICR had not been reached at the time of data cutoff. The 6- and 12-month DOR rates were 90.9% (95% CI, 68.3%-97.6%) and 85.2% (95% CI, 60.5%-95.0%), respectively.
Mario Sznol, MD, professor of medicine at Yale School of Medicine and comoderator of the press briefing, offered some perspective on the study, stating, “This is really an important advance for these patients. [As we know], any new therapeutic has substantial clinical significance.”
REFERENCE:
Lewis KD, Peris K, Sekulic A, et al. Interim analysis of phase 2 results for cemiplimab in patients with metastatic basal cell carcinoma (mBCC) who progressed on or are intolerant to hedgehog inhibitors (HHIs). Poster presented at: Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting & Pre-Conference Programs; November 9-14, 2020; Virtual Abstract 428.
