DeZern Discusses Incorporating Current Options for Managing Anemia in Low-Risk MDS
During a Case-Based Roundtable® event, Amy DeZern, MD, MHS, discussed dosing approaches for managing anemia with luspatercept in patients with low-risk myelodysplastic syndrome.

Amy DeZern, MD, MHS
Director, Bone Marrow Failure and MDS Program
Professor of Oncology
Johns Hopkins Medicine
Baltimore, MD

Peers & Perspectives in Oncology: What is the current treatment paradigm for anemia in low-risk MDS?
DeZern: [We need to] rule out other causes of anemia. We [consider] iron deficiency and the gastrointestinal [GI] bleed and so forth. I would say one thing that is often not always present in the baseline evaluation is that baseline serum EPO and ferritin levels. Those are very useful early in the diagnosis, especially for moving down an MDS pathway. The [supportive care] options that we have available traditionally [include] red blood cell transfusion, [ESAs, erythroid maturation agent, immunomodulatory agent, and immunosuppressive therapy].1
Candidly, most anemia is multifactorial. You can have anemia of chronic renal insufficiency, chronic inflammation, you can be iron deficient, you can have a GI [bleed]. I do all of these things. I put a lot of stock in the baseline EPO level. But that gets into how we’re going to treat them. Usually, if your kidney function is sufficiently poor to make your baseline EPO level lower than it should be for your degree of anemia, it probably is some anemia of chronic renal disease.
Are there situations where you would use antithymocyte globulin (ATG) and cyclosporine for anemia? What about lenalidomide?
In a hypocellular marrow, yes. I use a decent amount of ATG, because I see so much aplastic anemia, but I have to demonstrate in a good marrow sample, it’s hypocellular, and then those patients do quite well. [I used] lenalidomide for non del(5q) patients with anemia in the past, but I don’t do it anymore. It’s too toxic now that we have other options. I still tend to list it if patients want to know they have options, but it’s only about a 25% response rate in non del(5q) patients, it is not very durable, and it has a lot of toxicity, both financial and otherwise. I think that the field is getting away from that.
I always check the mutational panel if I’m going to do lenalidomide. The presence of an SF3B1 mutation with a del(5q) is adverse.2 I need to know [whether] they have a TP53 mutation going in, because the selective pressure to end up with acute myeloid leukemia in a patient like [this] is pretty significant. You can still respond even if you have a TP53 mutation; it’s just going to be short, and you’re going to get a selective advantage for the adverse clone and end up with leukemia.
How is the approach to transfusions for anemia changing in MDS?
People are increasingly empowered to improve their health care–related quality of life for all the right reasons. They’re advocating not to spend too much time in transfusion chairs. People are more attuned to their health care costs than ever. Philosophically, there are physicians who believe iron overload is the [worst outcome], and there are some physicians who let their patients…get very bronzed [due to iron overload]. But we know the chelators have a lot of financial toxicity as well as predominantly causing terrible diarrhea, so they’re hard to get people to stay on. We’ve all been using ESAs forever. How do we dose them? Which one do we use? Do we move them around? The need to always check the hemoglobin and have baseline hemoglobin, and make sure patients don’t get too many bills is tricky.
What are your impressions of the phase 3 COMMANDS trial (NCT03682536) of luspatercept-aamt (Reblozyl)?
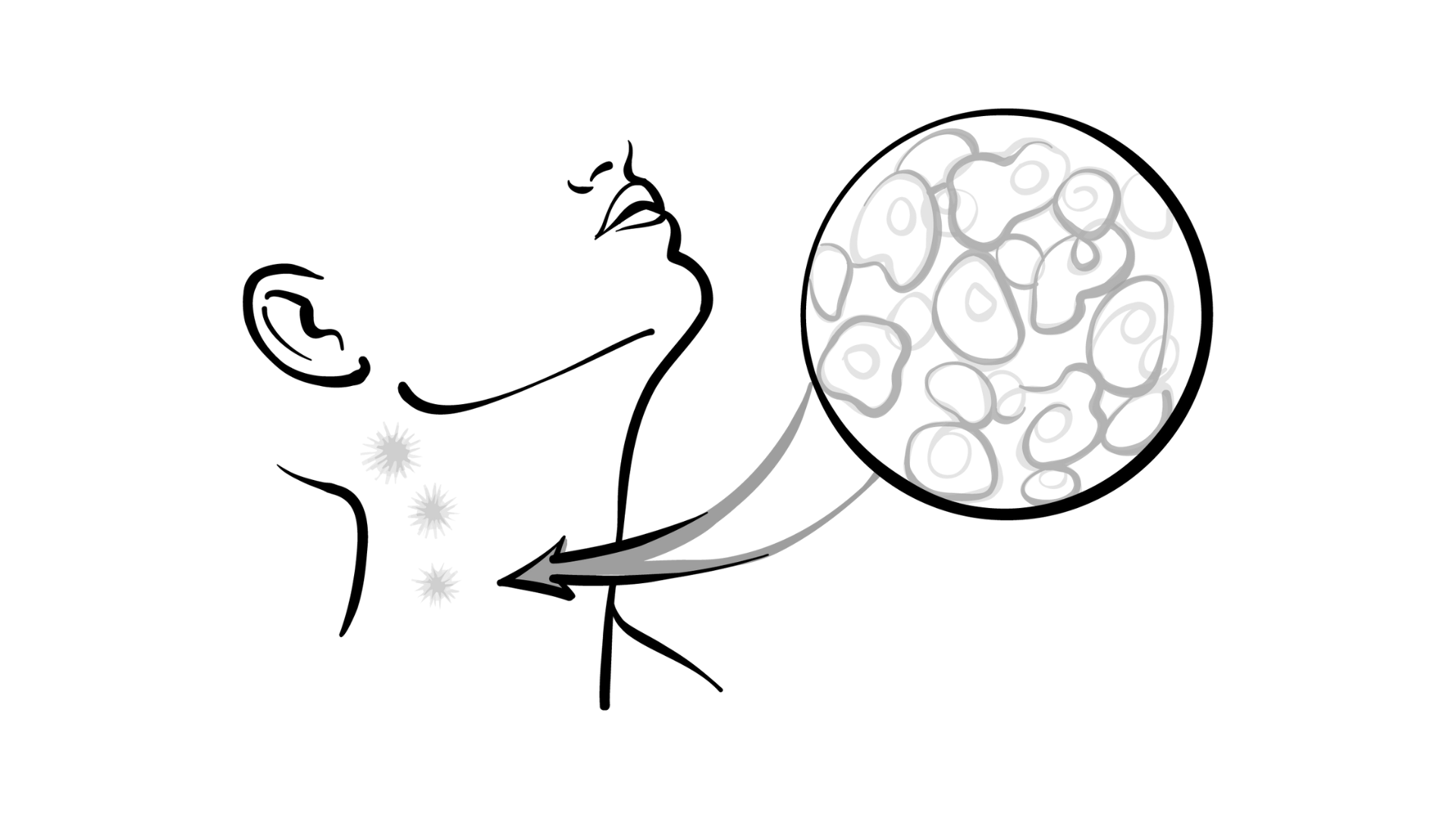
This had very prescriptive uptitration of the dose, and that is something that is very clear to me from using this for 4 or 5 years. Pushing the dose, you start at 1 mg/kg, and you want to use as little as possible, but you need to proactively uptitrate to 1.33 mg/kg and 1.75 mg/kg to make sure that you’re pushing the hemoglobin up. This is a late-stage maturation agent. We have a good handle on how it works, and there’s clearly a threshold level for some patients. The label says you go up every third dose [Figure3]. You [should] use your clinical judgment if you think it’s not working. I am aware of physicians who start at 1.75 mg/kg. I don’t do that, because I want to use it for as long as it can work.

This [trial’s comparator arm used] a much more European style of dosing epoetin alfa weekly, which is not how we always do it in the United States. But it’s still a strong comparator arm because all the Nordic data from the early 2000s uses epoetin alfa.
This was a positive trial. Its primary end point was…raising the hemoglobin at least 1.5 g/dL and being transfusion independent. I feel like we can trust that this is helping a patient. It’s not that all these patients went from 7.0 g/dL to 7.2 g/dL but didn’t [need] a transfusion. There is a clear difference at 12 weeks of RBC transfusion independence and raising the hemoglobin in the luspatercept arm compared with the epoetin alfa arm.4 The transfusion independence and the hematologic improvement are similar, which makes sense; these things should track together.
Looking at different durations of RBC transfusion independence past 12 weeks…it is more durable. If you respond to luspatercept, raise your hemoglobin, and become transfusion independent, it’s also going to last longer. But that effect is most prominent when you have ring sideroblast positivity at baseline and when you have an SF3B1 mutation. It’s also probably longer when you have received [fewer] red blood cells to begin with. We learned that from the relapsed/refractory phase 3 MEDALIST trial [NCT02631070] population that the heavily transfused patients are less likely to respond.5
Are there preclinical or clinical data for using both [luspatercept and epoetin alfa] together?
We’ve pushed for this a lot [in combination with] intravenous iron therapy and other things. There’s some resistance for obvious reasons. I am aware of a colleague who always uses them together. And I have to say the patients I see in consultation do well. It’s not how it’s intended, and it’s not on the label.… They’re working at different stages of hematopoiesis. At some point, though, there are only so many progenitors, there’s only so much marrow failure that can be stimulated, and so it’s going to have diminishing returns.
What additional toxicity was seen with luspatercept vs epoetin alfa?
I find luspatercept to be well tolerated. There is a little more fatigue with it [15% vs 7%], and I’ve had a couple patients where it was very clear that the fatigue was from the drug, not the anemia.4 I try to ask questions to [confirm] that, but mostly it’s well tolerated. Diarrhea was reported [15% vs 11%, respectively] any grade, but only a few higher grades [2 cases with luspatercept, 1 with epoetin alfa]; I have not had a problem with that in my patient population. [Hypertension is present, but] it’s not a black box label or anything like that. I try to make sure their blood pressure for either of these agents is reasonably under control, because we know it goes up, and…I put them on antihypertensives on occasion.
Can you give a brief summary of the phase 2/3 IMerge trial (NCT02598661) of the newly approved agent imetelstat (Rytelo)?
Imetelstat is an intravenous drug given every 4 weeks, and this study was placebo controlled, looking at 8-week transfusion independence. When this was designed, that was an acceptable end point, [but] the field is moving toward more meaningful end points like a rising hemoglobin and a longer metric, because a patient who goes every 3 months without a transfusion might just hit the window [of 8 weeks without supportive care], and then your drug looks very good.
This was a positive trial. It met its primary end point of transfusion independence for 8 weeks or greater very clearly.6 On the weeks of red cell transfusion independence, imetelstat looks much better than placebo, and it’s durable. There are laboratory correlates that show in SF3B1-mutated [disease], this is a disease-modifying drug because the variant allele frequencies of mutations decrease.
This is a more toxic drug. There is much more hematologic toxicity, but these are refractory patients, so they will probably tolerate more toxicity. Three-quarters of the patients had profound neutropenia and thrombocytopenia, because most of it was grade 3 or 4. Most of that toxicity resolves if you hold it for 4 weeks, but even still, we have to decide as a field what we think of [this toxicity].
The other signal was alanine aminotransferase increase in 12%. The diarrhea is less than that with luspatercept, but it’s mainly the hematologic toxicity [that is a concern]. As hematologist-oncologists, we are willing to tolerate that, but there is something to think about with this drug. I think it’s because it truly is treating the disease a little bit more.
Are there any data on patients whose anemia failed to respond to luspatercept and are then given imetelstat?
This is going to be the problem we have in terms of sequencing. Because of the enrollment period for this, only [6 patients in the experimental arm and 7 in the placebo arm] had received luspatercept. We can now give luspatercept up front. What if imetelstat doesn’t work after that, [although] this is our refractory drug, and then we [must] use an ESA in the third line? I think we just don’t know.… Sequencing is going to become a problem that we have in the MDS space if we have more drugs.

What other data give insight on practical use of luspatercept?
There was an interest in understanding some longer-term outcomes of the luspatercept data. [Based on] a real-world retrospective [analysis], approximately 60% were not using dose escalations.7 Most don’t do dose reductions either [93.7%]. Approximately one-third of patients had discontinued it [Table 17]. The reasons were worsening of disease and lack of hematologic improvement, but relatively few due to toxicity or patient choice. Maybe these are the adverse outcome [data] that matter. You can look at the trial AEs, but if most patients in the real world are not discontinuing it for those reasons, I think that’s helpful.
[Based on] the follow-up COMMANDS data that came out at the 2023 Society of Hematologic Oncology meeting, looking at the reduction of the transfusion burden and the dose titration, it came out of the trial data, but it’s very comparable to the real-world data, which I do find reassuring in that regard [Table 28].

Is there a cutoff in how many transfusions are considered a treatment failure?
We know we can rescue a few patients with adding back iron if we overly deplete them. I just saw my first patient who was clearly iron deficient because of luspatercept. That can happen there too. I hadn’t seen it yet because nobody had been on it long enough. ESA [can also trigger iron deficiency]. If you have enough selective pressure for erythropoiesis, you use up all your building blocks.
REFERENCES:
1. Garcia-Manero G. Myelodysplastic syndromes: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98(8):1307-1325. doi:10.1002/ajh.26984
2. van de Loosdrecht AA, Cremers EMP, Alhan C, et al. Determinants of lenalidomide response with or without erythropoiesis-stimulating agents in myelodysplastic syndromes: the HOVON89 trial. Leukemia. 2024;38(4):840-850. doi:10.1038/s41375-024-02161-6
3. Reblozyl. Prescribing information. Celgene Corporation; 2024. Accessed June 28, 2024. https://tinyurl.com/56xpjakw
4. Platzbecker U, Della Porta MG, Santini V, et al. Efficacy and safety of luspatercept versus epoetin alfa in erythropoiesis-stimulating agent-naive, transfusion-dependent, lower-risk myelodysplastic syndromes (COMMANDS): interim analysis of a phase 3, open-label, randomised controlled trial. Lancet. 2023;402(10399):373-385. doi:10.1016/S0140-6736(23)00874-7
5. Fenaux P, Platzbecker U, Mufti GJ, et al. Luspatercept in patients with lower-risk myelodysplastic syndromes. N Engl J Med. 2020;382(2):140-151. doi:10.1056/NEJMoa1908892
6. Platzbecker U, Santini V, Fenaux P, et al. Imetelstat in patients with lower-risk myelodysplastic syndromes who have relapsed or are refractory to erythropoiesis-stimulating agents (IMerge): a multinational, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2024;403(10423):249-260. doi:10.1016/S0140-6736(23)01724-5
7. Mukherjee S, Brown-Bickerstaff C, Falkenstein A, et al. Treatment patterns and outcomes with luspatercept in patients with lower-risk myelodysplastic syndromes: a retrospective US cohort analysis. Hemasphere. 2024;8(1):e38. doi:10.1002/hem3.38
8. Komrokji RS, Platzbecker U, Della Porta M, et al. MDS-234 reduction of transfusion burden (TB), hemoglobin increase, and dose titration in the COMMANDS study of luspatercept versus epoetin alfa (EA) in erythropoietin-stimulating agent (ESA)-naive patients with transfusion-dependent (TD) lower-risk myelodysplastic syndromes (LR-MDS). Clin Lymph Myel Leuk. 2023;23(suppl 1):S184. doi:10.1016/S2152-2650(23)00608-0