A Multidisciplinary Approach Meets the Needs of Patients With Liver Cancer
Because of the complex nature of diagnosing, treating, and managing hepatocellular carcinoma, a multidisciplinary approach in the community setting can provide optimal care to patients with the disease.

Because of the complex nature of diagnosing, treating, and managing hepatocellular carcinoma (HCC), a multidisciplinary approach in the community setting can provide optimal care to patients with the disease. The disease’s relatively low incidence in the US population, which makes it an uncommon cancer encountered in the community setting, adds to the challenges facing the general oncologist. To better aid community cancer centers in the care of patients with HCC, the Association of Community Cancer Centers (ACCC) issued an environmental report of the current HCC landscape that promotes effective practices and considerations for community practices based on discussions with an expert advisory committee, partner organizations, and literature review.1
General oncologists need to “keep in mind that HCC is a disease that will increase in incidence given the hepatitis C epidemic in the United States,” said Philip A. Philip, MD, PhD, a member of the ACCC’s multidisciplinary hepatocellular cancer care advisory committee. “There is still a steep learning curve associated with HCC.”
HCC is the most common primary liver malignancy (80%-90% of cases in the United States) and is on the rise.2The incidence rate has doubled around the world since the 1970s and has been increasing rapidly in the United States over the past 20 years.3The estimated numbers of new US cases and deaths for 2018 are 42,220 and 30,200, respectively, with less than 18% of patients sur- viving at 5 years (based on data for HCC and intrahepatic bile duct cancer combined).2
The ACCC recommends 6 practices that community cancer centers can implement to improve care. These include the creation of a multidisciplinary team (MDT) or access to an external expert tumor board; regularly scheduled MDT evaluations of HCC cases; HCC screening through operational pathways that foster collaboration with other healthcare providers; adherence to national HCC guidelines; development of internal operational pathways to unify, streamline, and document care; and a focus on patient-centered care.
Creating an MDT might be beyond the scope of a community cancer center. Philip, the Kathryn E. Cramer M.D. Endowed Chair in Cancer Research and professor of medicine at Barbara Ann Karmanos Cancer Institute and Wayne State University in Detroit, Michigan, understands that tumor boards dedicated to HCC are usually not available in the community setting. He suggests as an alternate practice the establishment of a general gastrointestinal tumor board, which can discuss HCC cases. The idea is to establish “teams of people who have a special interest in managing patients with HCC, with the idea to benefit from the knowledge and expertise of others who treat the disease,” said Philip.
Along with offering best practice suggestions, the ACCC conducted a provider survey to determine how providers in the community setting are managing care for patients with HCC and to better understand effective tools, resources, challenges, and education needs (FIGURE).
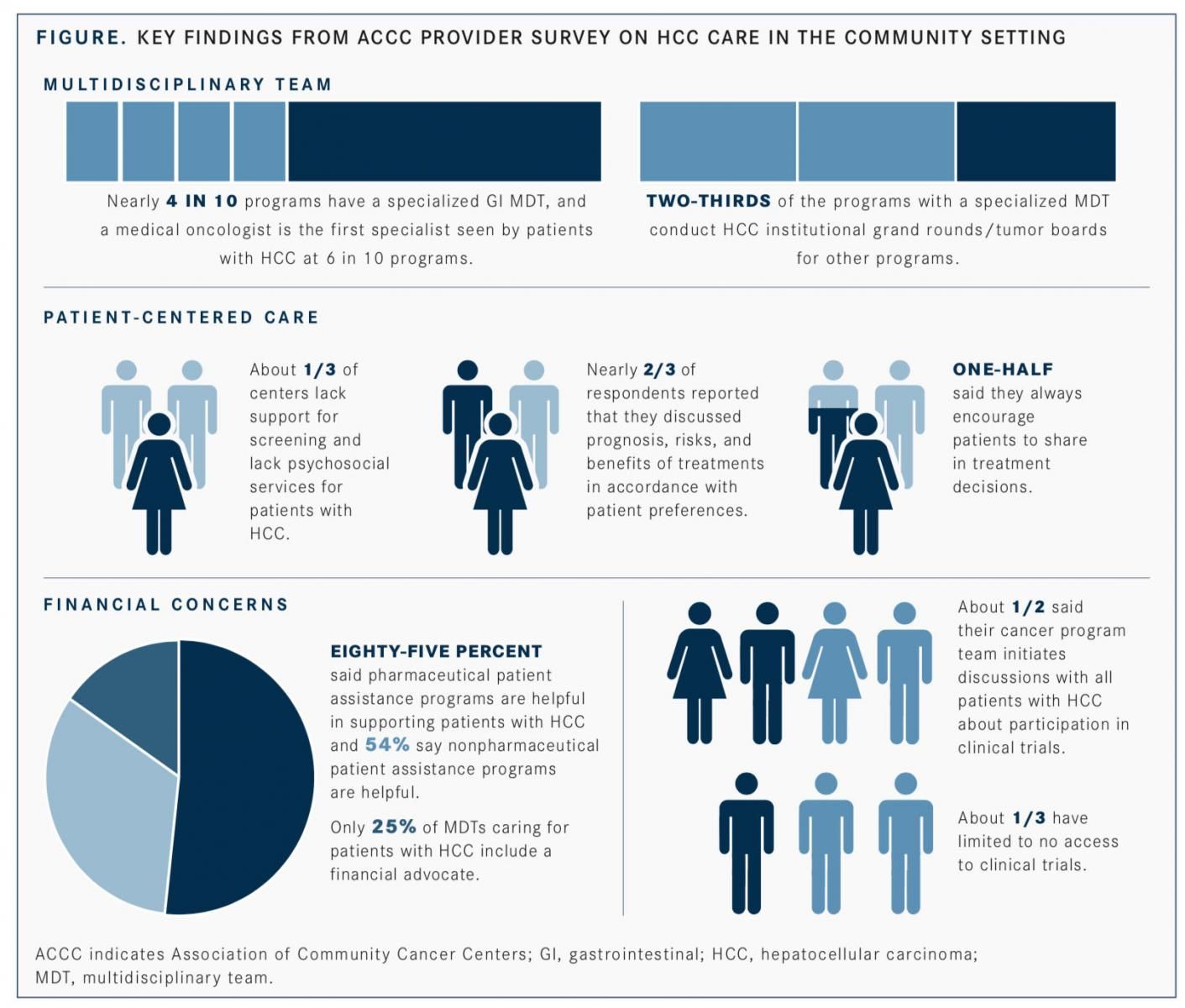
According to the survey, 4 in 10 community cancer centers have a specialized gastrointestinal MDT and a medical oncologist is the first specialist seen by a patient with HCC at 6 in 10 centers. In addition, the survey reported that the top provider education needs to include HCC guideline updates, criteria for screening, and the role of liver transplant for select patients.
Philip recommends that in addition to healthcare providers and allied health professionals, stakeholders, policy makers, insurers, patients, and patient advocacy groups read the report. “Many patient advocacy groups can encourage patients to seek additional medical opinions about their disease, its treatment, and prognosis,” Philip said.
Like many patients with other cancers, those with HCC need more accessible information about their diagnosis and treatment. In general, patient-centered care is an indicator of quality healthcare and contributes directly or indirectly to improved clinical outcomes and health-related quality of life. A patient-centered approach, according to the report, should help patients navigate to the care they need, respect their preferences, provide timely and relevant information, support the patient and family, involve the patient in decision making, and align evidence-based decision making.
A patient diagnosed with HCC should seek multiple expert opinions and explore the opportunity to enroll in clinical trials, said Philip.
