Boost in Survival Rates for Younger Patients With Melanoma Attributed to Immunotherapy Agents
“New therapies have increased the median survival for advanced-stage melanoma from approximately 9 months before 2011 to at least 2 years, based on [data from] clinical trials,” Elizabeth Ward, PhD, and colleagues wrote about their report on cancer burden in younger patients.
Despite increased rates of melanoma among men and women aged 20 to 49 years, death rates have declined, likely because of the introduction of targeted and immunotherapy agents for the treatment of advanced melanoma.
“New therapies have increased the median survival for advanced-stage melanoma from approximately 9 months before 2011 to at least 2 years, based on [data from] clinical trials,” Elizabeth Ward, PhD, of the North American Association of Central Cancer Registries (NAACCR), and colleagues wrote about their report on the cancer burden in younger patients.1
The report is based on data from the American Cancer Society, the US Centers for Disease Control and Prevention, the National Cancer Institute, and the NAACCR, and highlights trends and opportunities in cancer surveillance data to guide control efforts.
Melanoma Incidence Rate
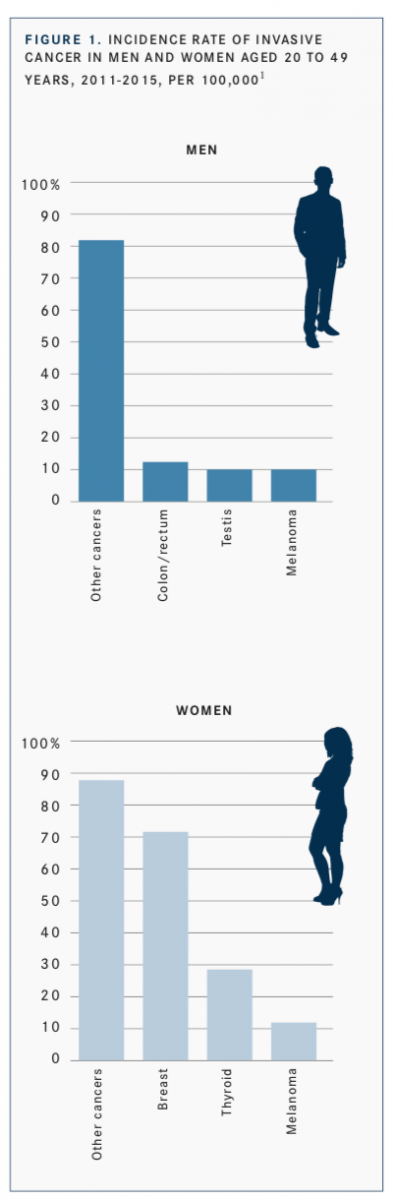
The incidence rates for all invasive cancers were lower among men than they were among women (115.3 vs 203.3 cases per 100,000). For both sexes, melanoma ranked among the 3 cancers with the highest incidence rates, following colorectal and testicular cancers in men and breast and thyroid cancers in women (FIGURE 1).
Incidence rates of melanoma increased 2.3% in men (P<.001) and 1.7% in women (P<.001) from 2011 to 2015. These rates represented the second-highest increases, following significant increases in liver cancers for both groups.
Melanoma Survival Rate
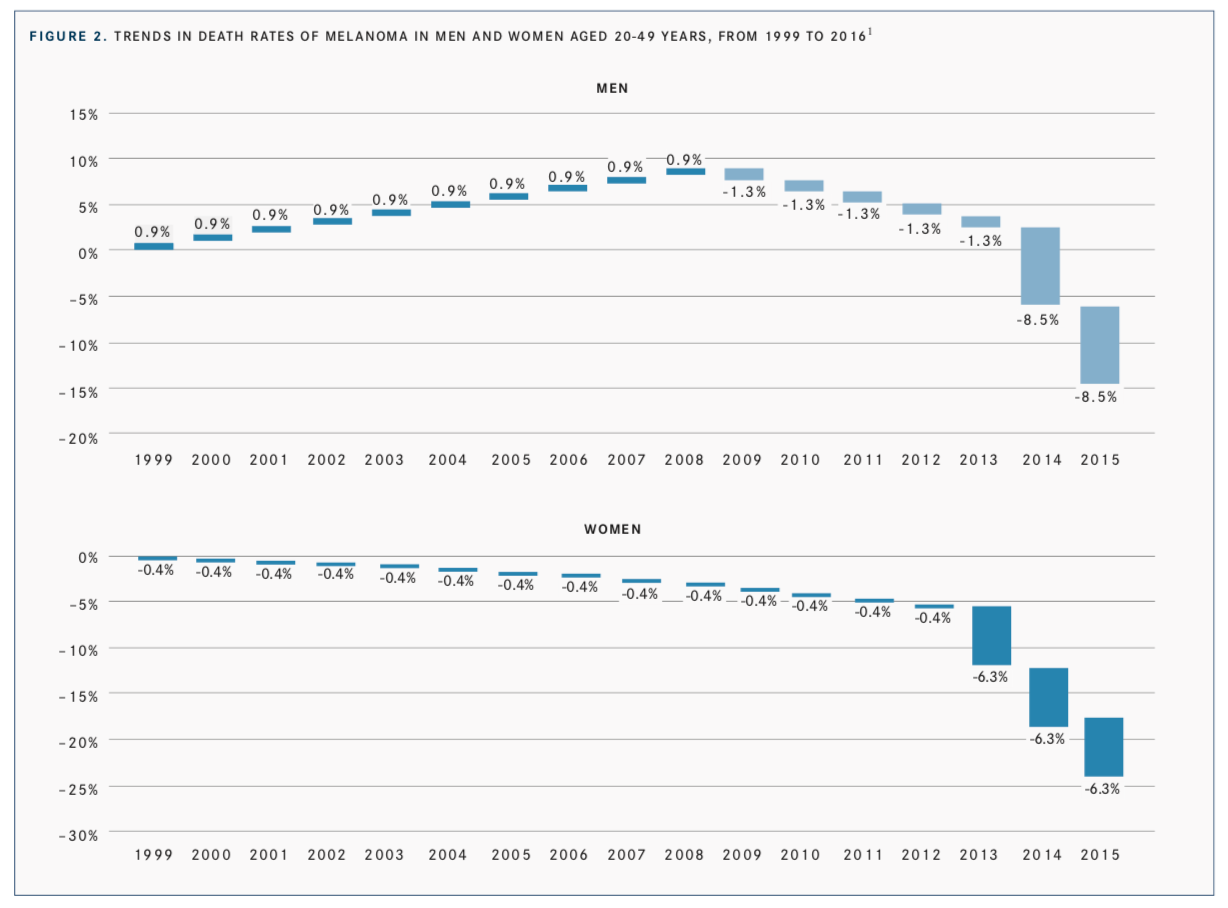
Despite these increases, survival rates have risen alongside higher disease incidence rates. Among men, death rates for melanoma had a 5-year decrease of 5% between 2012 and 2016; in women, that rate was 4.9%. These were the steepest decreases observed in each group by cancer type. (FIGURE 2).1
Shift in Survival With Modern Therapies
According to the Surveillance, Epidemiology, and End Results Program2 database (SEER-18), 1-year overall survival rates in patients with metastatic melanoma were significantly better in patients treated in the era following the introduction of targeted therapies (38.9%) than they were in patients treated before targeted therapies were available (36.8%); the 2-year over- all survival rates were 28.3% versus 23.5% (P= .001). The report3 defined the “pretargeed era” as 2004 to 2010 and the “posttargeted era” as 2011 to 2014.
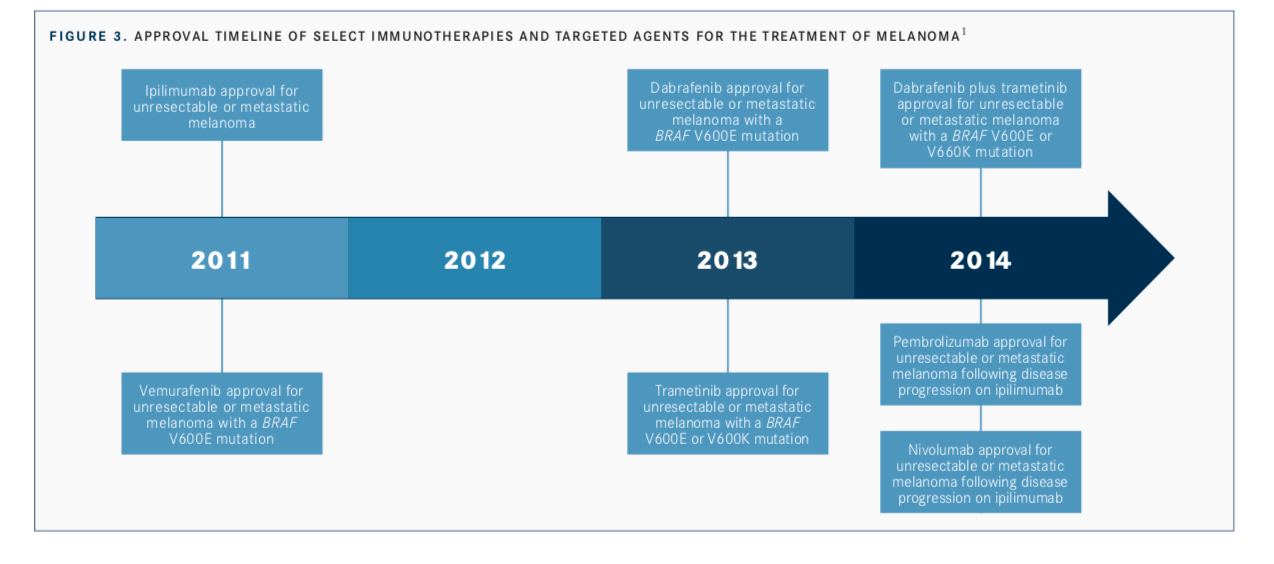
Between those years, numerous targeted agents, such as dabrafenib (Tafinlar) and trametinib (Mekinist), and immunotherapies, such as nivolumab (Opdivo), were approved for the treatment of metastatic melanoma (FIGURE 3).1These approvals included monotherapy and combination indications.
Overall, the investigators saw these rapid declines in death rates from melanoma as an integral factor of declines observed in all cancer sites in this population subset.
References
- Ward E, Sherman RL, Henley SJ, et al. Annual report to the nation on the status of cancer, 1999-2015, featuring cancer in men and women ages 20-49 [published online May 30, 2019].J Natl Cancer Inst. doi: 10.1093/jnci/djz106.
- Uprety D, Bista A, Chennamadhavuni A, Niroula A, Jafri SIM, Smith A, Arjyal L Survival trends among patients with metastatic melanoma in the pretargeted and the post-targeted era: a US population-based study. Melanoma Res. 2018;28(1):56-60. doi: 10.1097/ CMR.0000000000000394.
- Luke JJ, Flaherty KT, Ribas A, Long GV. Targeted agents and immunotherapies: optimizing outcomes in melanoma.Nat Rev Clin Oncol. 2017;14(8):463-482. doi: 10.1038/nrclinonc.2017.43.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More