Venetoclax Plus Low-Dose Cytarabine Fails to Improve OS in AML
The combination of venetoclax plus low-dose cytarabine did not demonstrate a statistically significant improvement in overall survival compared with LDAC plus placebo in patients with acute myeloid leukemia who were ineligible for intensive chemotherapy at the time of a planned analysis, missing the primary end point of the phase III VIALE-C trial.
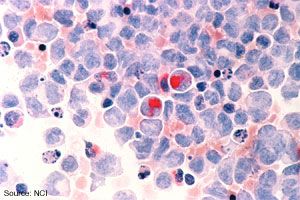
The combination of venetoclax (Venclexta) plus low-dose cytarabine (LDAC) did not demonstrate a statistically significant improvement in overall survival (OS) compared with LDAC plus placebo in patients with acute myeloid leukemia (AML) who were ineligible for intensive chemotherapy at the time of a planned analysis, missing the primary end point of the phase III VIALE-C (M16-043) trial (NCT03069352), AbbVie announced in a press release.
Overall, venetoclax plus LDAC had a median OS of 7.2 months resulting in a 25% reduction in the risk of death versus 4.1 months in the LDAC monotherapy arm (HR = 0.75; 95% CI, 0.52-1.07;P=.11). In the post hoc analysis after 6 additional months of follow up, the median OS in the venetoclax arm versus the LDAC arm was 8.4 months and 4.1 months, respectively (HR = 0.70; 95% CI, 0.50-0.99).
In terms of secondary outcomes, the complete remission (CR) rate was 27.3% in the venetoclax group versus 7.4% in the LDAC group. The CR with incomplete blood count recovery (CRi) was 47.6% in the venetoclax group compared with 13.2% in the LDAC group. The CR with partial hematologic recovery (CRh) was 46.9% in the venetoclax arm versus 14.7 in the LDAC arm. For the final outcome of CR with CRi by the initiation of cycle 2, the rate observed was 34.3% in the venetoclax group compared with 2.9% in the LDAC group.
For both drugs, the safety profile observed in this study were consistent with previous safety seen in phase I/II clinical trials. Venetoclax was approved by the FDA based on its safety profile and this indication remains unchanged to date.
The most common adverse events observed in the venetoclax and LDAC groups, respectively were febrile neutropenia (15.5%, 11.8%), neutropenia (45.8%, 17.7%), thrombocytopenia (40.9%, 36.8%), and anemia (26.1%, 22.1%). More AEs were considered serious in the venetoclax group than the LDAC group. There were no cases of serious neutropenia or anemia in the LDAC group.
VIALE-C (M16-043) is an active randomized, double-blind, placebo-controlled study in which oral venetoclax 600 mg daily plus LDAC 20 mg/m2on day 1 to 10 of each 28-day cycle are administered and compared with placebo plus LDAC in patients with AML who are ineligible for intensive chemotherapy.
The study included patients who are aged 75 or older or those 18 to 74 years of age who are not fit for intensive chemotherapy. Patients were required to have an ECOG performance status of 0 to 2 if aged 75 years or older or 0-3 if between the ages of 18 and 74. Patients were also required to have a projected life expectancy of at least 12 weeks and have adequate renal and liver function. Patients who received prior treatment for AML were excluded from the study, as were those with central nervous system involvement with AML, promyelocytic leukemia, human immunodeficiency virus, hepatitis B or C. The study also excluded individuals with cardiac disease, respiratory diseases, or a history of prior malignancies.
“We remain committed to AML patients and our research in AML and other blood cancers,” said Neil Gallagher, MD, PhD, chief medical officer and vice president of development, AbbVie. “The study results, while not statistically significant, are indicative of the clinical activity of venetoclax in combination with low-dose cytarabine.”
Reference:
AbbVie provides update from phase 3 study evaluating venclexta® (venetoclax) in combination with low-dose cytarabine in newly-diagnosed patients with acute myeloid leukemia (AML) [new release]. Chicago, Illinois: AbbVie; February 28, 2020.https://bit.ly/2Tg1bOH. Accessed March 2, 2020.