Tiragolumab/Atezolizumab Combo Fails to Meet Primary End Point in NSCLC Trial
The phase 3 SKYSCRAPER-01 trial of tiragolumab and atezolizumab in PD-L1-high non–small cell lung cancer did not meet its primary end point of overall survival.
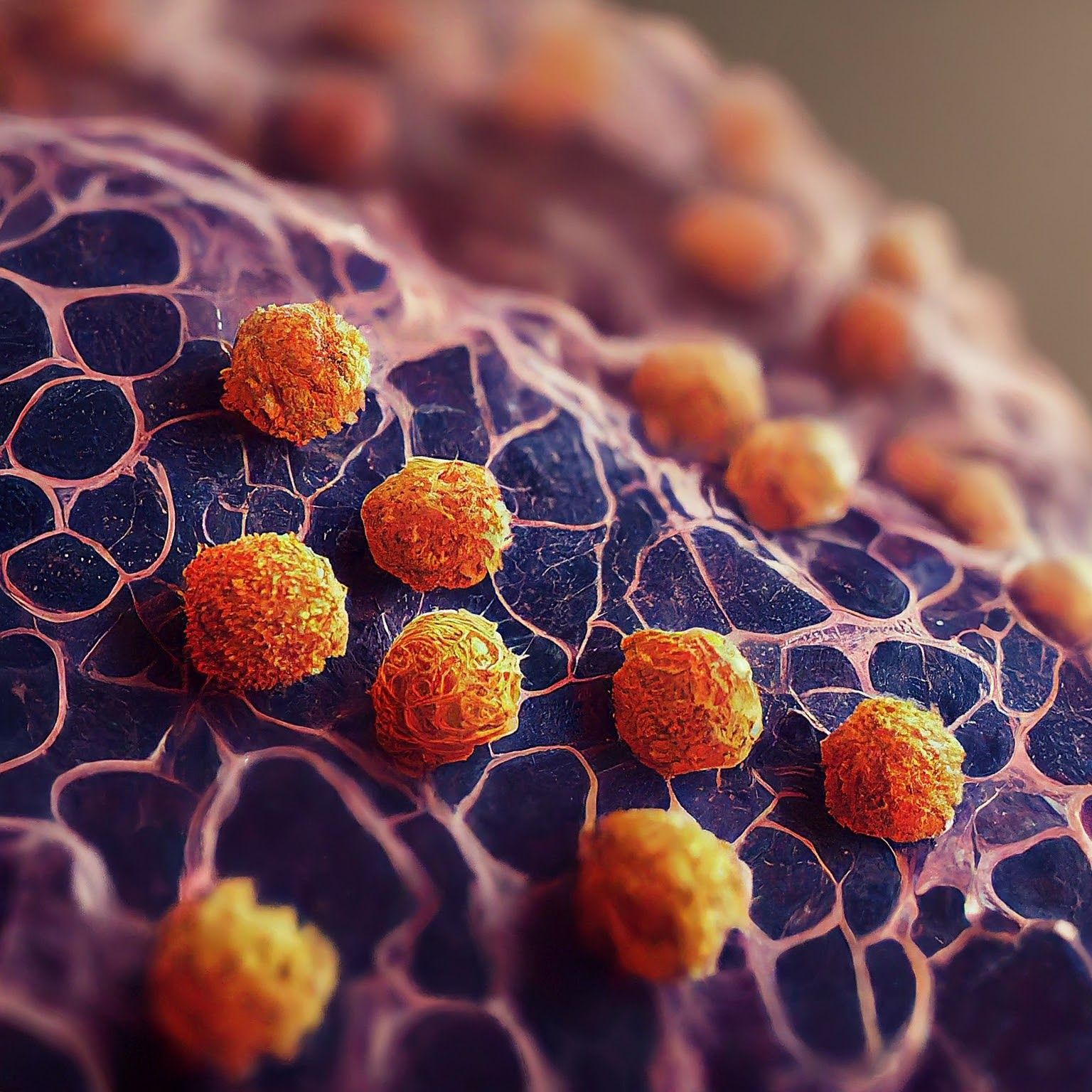
Microscopic image of non-small cell lung cancer - Generated with Google Gemini AI
The primary end point of overall survival (OS) at the final analysis was not met in the phase 3 SKYSCRAPER-01 study (NCT04294810), which evaluated the combination of tiragolumab and atezolizumab (Tecentriq) vs atezolizumab alone in PD-L1-high, locally advanced or metastatic non–small cell lung cancer (NSCLC).1
Further, the overall safety profile of the combination stayed consistent with longer follow-up, and there were no new safety signals identified.
Full findings are expected to be presented at a medical meeting in 2025.
According to the press release, Roche, the developer of tiragolumab, will evaluate its ongoing studies of the agent to determine if adjustments are necessary. Additional phase 3 data from various tumor types are anticipated next year.
A Closer Look at Tiragolumab and Atezolizumab
Tiragolumab is an investigational immune checkpoint inhibitor with an intact Fc region, designed to selectively bind to TIGIT, a novel inhibitory immune checkpoint receptor, with the aim of potentiating anti-tumor immune responses.
Atezolizumab, a monoclonal antibody, is engineered to bind to PD-L1, a protein expressed on tumor cells and tumor-infiltrating immune cells, thereby blocking its inhibitory interactions with PD-1 and B7-1 receptors. This blockade can potentially reactivate T cells and enhance antitumor immune responses.
Behind the SKYSCRAPER-01 Trial
SKYSCRAPER-01, a global, phase 3, randomized, double-blind trial, is evaluating the combination of tiragolumab plus atezolizumab vs atezolizumab alone.2 A total of 534 patients with PD-L1-high previously untreated, locally advanced, unresectable or metastatic NSCLC were enrolled and randomly assigned 1:1 to receive either the combination with tiragolumab or atezolizumab alone until disease progression, loss of clinical benefit, or unacceptable toxicity.
The experimental arm of the study administered 1200 mg atezolizumab intravenously (IV) plus 600 mg tiragolumab IV on day 1 of each 21-day cycle to patients whereas those in the placebo comparator arm received a matching dose of atezolizumab alone.
Patients aged 18 years and older with histologically or cytologically documented locally advanced or recurrent NSCLC who are not eligible for curative surgery and/or definitive radiotherapy with or without chemoradiotherapy were eligible for enrollment in the study. Additional enrollment criteria included having no prior systemic treatment for metastatic NSCLC, high tumor tissue PD-L1 expression, measurable disease per RECIST v1.1, adequate hematologic and end-organ function, and an ECOG status of 0 or 1. Those included in the extended enrollment in China are required to be a current resident of mainland China or Taiwan and of Chinese ancestry.
In addition to OS, a primary end point was progression-free survival (PFS), which was also not met. Other primary end points were percentage of patients with adverse events, and cytokine release syndrome.
Secondary end points included investigator-assessed PFS in the secondary analysis set, OS in the secondary analysis set, investigator-assessed confirmed objective response rate, investigator-assessed duration of response, investigator-assessed PFS rates at 6 and 12 months, OS rates at 12 and 24 months, and time to confirmed deterioration.
REFERENCES
Roche reports update on phase III SKYSCRAPER-01 study results. News release. Roche. November 26, 2024. Accessed November 26, 2024. https://tinyurl.com/yzzwadny
A study of tiragolumab in combination with atezolizumab compared with placebo in combination with atezolizumab in patients with previously untreated locally advanced unresectable or metastatic PD-L1-selected non-small cell lung cancer (SKYSCRAPER-01). ClinicalTrials.gov. Updated October 10, 2024. Accessed November 26, 2024. https://clinicaltrials.gov/ct2/show/NCT04294810.