Testing the Sensitivity of T790M Mutation Detection Across Platforms
Heather Wakelee, MD, discusses T790M mutation detection among different platforms in an analysis from the TIGER-X trial
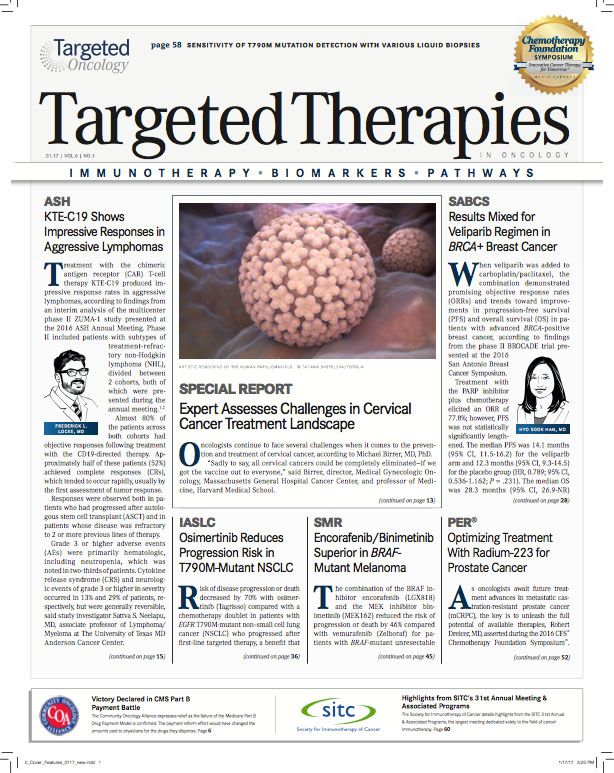
Heather Wakelee, MD
Mutation detection using plasma- and urine-based circulating tumor DNA (ctDNA) assays is growing in frequency among the ever-expanding field of liquid biopsies, especially for identifying patients with nonsmall cell lung cancer (NSCLC) with anEGFRT790M resistance mutation.
“Looking for T790M is something that’s an area of active investigation and there are a lot of different platforms being developed,” Heather Wakelee, MD said.
Wakelee, an associate professor of medicine in the Division of Oncology at Stanford University Medical Center, and colleagues examined T790M mutation detection among different platforms in an analysis from the TIGER-X trial that was presented at the International Association for the Study of Lung Cancer 17th World Conference on Lung Cancer.
Examining molecular diagnostic results from 174 matched tissue samples and plasma and urine ctDNA specimens, researchers found that 170 of these patients (97.7%) tested positive for the T790M mutation, which was discovered by any one of the 3 methods. Plasma ctDNA testing alone identified 142 total cases (81.6%), urine ctDNA testing identified 139 (79.9%), and combined urine and plasma ctDNA testing identified 165 cases (94.8%). Further, combination testing identified T790M in 92.7% of patients with intrathoracic disease and in 95.8% of patients with extrathoracic disease (P = .47).
In an interview withTargeted Therapies in Oncology(TTO), Wakelee discusses the sensitivity of plasma and urine ctDNA platforms and the benefits of each, as well as the possibility for combined plasma and urine ctDNA testing for T790M mutation detection.
TTO: How was T790M mutation detection analyzed between different platforms?
Wakelee:
The study was an additional analysis from the TIGER-X trial. That was a study looking at the drug rociletinib, which is no longer in development now, but was at the time. It’s anEGFR- specific drug, designed for the T790M resistance mutation. The patients who went on the trial all hadEGFR-mutated lung cancer and had progressed on a standard first-generation drug. With that, the patients who were enrolled all theoretically had T790M.
We had tissue from over 500 patients, plasma from almost as many, and then we had urine from over 200 patientsthe urine was a secondary test so not all of the patients participated—but we looked to see if we could find the T790M mutation in different platforms. We had 2 different tests for the plasma—one was the BEAMing assay, which is a bit more standard, and the other one was the Trovera next-generation sequencing (NGS) analysis; it was that same technology that also looked for the urine T790M. For tissue testing, it was the more standard cobas or Qiagen. We then looked across these different platforms for how frequently we could find T790M.
TTO: How did the results differ between each of the platforms?
Wakelee:
The sensitivity of all the assays is quite good. We could find about 80% sensitivity for T790M with either of the plasma assays, as well as with the urine assay. What’s particularly interesting is when you look at how they all intersect. For most of the patients, we were able to find T790M by all 3 assays. But there were some subsets of patients where we only found it with the plasma assay or only with the urine assay or only in the tissue. When we looked back to see how that correlated with drug response, it didn’t matter how you found T790M; whatever way you found it predicted for drug response.
TTO: What is the significance of this finding according to each of the platforms?
Wakelee:
It tells us that it’s not that you’re getting false positives, it’s more that there’s some false negatives. For tissue, that’s more likely [due to] tissue heterogeneity, where you might have a specific piece of tumor biopsy but that’s not necessarily where T790M is. With both the plasma and urine assays, it has more to do with the sensitivity of the test.
From a practical standpoint, I think what it tells us is that we can definitely consider doing either the urine or a plasma assay to look for T790M in our patients with EGFR mutations who are now becoming resistant. But if we don’t necessarily find T790M that way we shouldn’t say "Oh, they don’t have it,’ but we should then think about doing the tissue analysis.
TTO: What sets the urine platform apart from the plasma assays?
Wakelee:
Looking for T790M is something that’s an area of active investigation and there are a lot of different platforms being developed. This is really the first urine assay, which is what’s unique about it. I’ve had examples in my clinic where a patient will come in and they’ve already had their blood drawn before they come see me, and then we see the scan result that shows progression, so then we talk about T790M testing and many of them say, "I really don’t want to go back and get my blood drawn," so that’s one particular utility of the urine.
One other thing, especially in a subset of patients where the progression is not everywhere but just in the lungsthe M1a patients— for those, the sensitivity of the plasma was a little bit lower for the M1a patients versus the M1b patients, where there were more extensive metastases. But with the urine assay it didn’t seem to matter as much. When you combine the urine and the plasma together, the sensitivity for the M1a patients was over 90%, and for the M1b patients it was over 95%. So that’s really good. If we could do a urine and a plasma test, you’re going to increase your sensitivity such that we’ll be able to do a biopsy for the majority of patients, hopefully.
TTO: What remaining challenges in the area of T790M testing in patients with NSCLC would you like to see addressed in the future?
Wakelee:
I think that one of the remaining challenges is that no assay that we have for T790M is perfect, and so I think continuing to improve the sensitivity, specificity, also bringing cost down for patients, I think that that’s where we have room for development. Remaining research questions are going to be: how often should we test, if you find T790M in a patient before they have clinical progression what does that mean, and when do we think about making those switches in our therapies.
Reference:
Wakelee H, Melnikova V, Karlovich CA, et al. A highly sensitive next-generation sequencing platform for detection of NSCLC EGFR T790M mutation in urine and plasma. Presented at: IASLC 17th World Confer- ence on Lung Cancer; December 4-7, 2016; Vienna, Austria. Abstract MA08.01.