Study of Tislelizumab/Chemo Meets Primary End Points in Resectable NSCLC
Major pathological response and pathological complete response data from the phase 3 RATIONALE 315 study in NSCLC will be presented at the European Society for Medical Oncology Congress 2023.
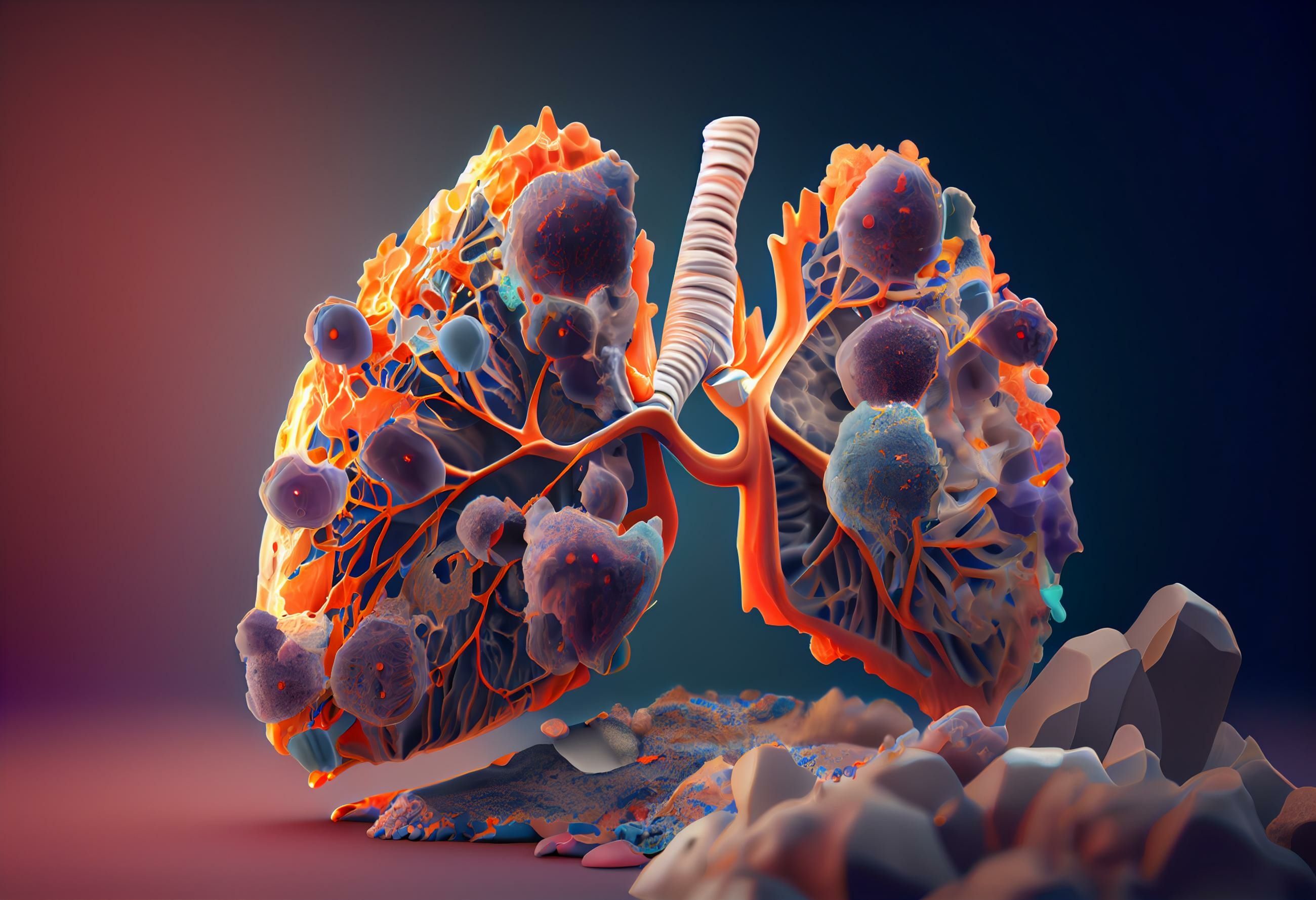
KRAS G12C mutation in non-small cell lung cancer: © Aiden - stock.adobe.com
The dual primary end points of major pathological response (MPR) by blinded independent pathology review and event-free survival (EFS) by blinded independent central review (BICR), have been met in the phase 3 RATIONALE 315 study (NCT04379635) evaluating tislelizumab (BGB-A317) in combination with chemotherapy prior to surgery and as a single agent after surgery in patients with resectable stage II or IIIA non–small cell lung cancer.1
Tislelizumab with chemotherapy before surgery and as a single agent after surgery was compared with neoadjuvant chemotherapy plus placebo followed by placebo after surgery and led to statistically significant and clinically meaningful improvements in MPR and EFS, as well as a statistically significant improvement in pathological complete response (pCR) after neoadjuvant therapy, a key secondary end point of the study.
A total of 56.2% of patients with NSCLC who received tislelizumab with chemotherapy before surgery achieved MPR vs 15.0% of patients given chemotherapy alone, making for a difference of 41.1% (95% CI, 33.2-49.1; P <.0001). Further, 40.7% of patients treated with the tislelizumab combination achieved pCR vs 5.7% of patients treated with chemotherapy alone for a difference of 35.0% (95% CI, 27.9-42.1; P <.0001).
The combination of tislelizumab plus chemotherapy was generally well-tolerated, and no new safety signals were identified.
“The data from RATIONALE 315 are encouraging and demonstrate that early integration of tislelizumab into the treatment paradigm may help both improve responses at the time of surgery and reduce the recurrence risk for these patients. These results add to the growing evidence suggesting the potential benefits of tislelizumab in treating patients with NSCLC,” said Mark Lanasa, MD, PhD, chief medical officer, Solid Tumors at BeiGene, in a press release.
In addition, a subsequent interim analysis conducted by the independent data monitoring committee from RATIONALE 315 showed that the addition of tislelizumab to neoadjuvant platinum-based chemotherapy followed by adjuvant tislelizumab monotherapy led to a statistically significant improvement in EFS vs neoadjuvant chemotherapy alone in this patient population.
The interim results from this study will be submitted for presentation at an upcoming medical conference, and the MPR and pCR data will be presented as a late-breaking mini oral presentation on October 23 at the European Society for Medical Oncology Congress 2023.
"Lung cancer remains the most common type of cancer and the leading cause of cancer-related death worldwide. Despite available treatment options, rates of recurrence within 5 years remain unacceptably high, underscoring the need for innovative new neoadjuvant and adjuvant interventions to help improve patient outcomes,” said Lanasa, in a press release.
RATIONALE 315 is a randomized, double-blind, placebo-controlled, phase 3 trial where investiagtors are evaluating the efficacy and safety of neoadjuvant tislelizumab with platinum-based doublet chemotherapy, followed by surgery and subsequent adjuvant tislelizumab, compared with placebo and neoadjuvant platinum-based doublet chemotherapy followed by surgery and subsequent adjuvant placebo for the treatment of patients with resectable stage II or IIIA NSCLC.2
The trial enrolled a total of 453 patients and randomized them in a 1:1 fashion to receive either tislelizumab or placebo in combination with chemotherapy.
Patients with histologically confirmed stage II or IIIA NSCLC who have an ECOG performance status of 0 or 1, measurable disease as assessed per RECIST v1.1, and eligibility for an R0 resection with curative intent were eligible for enrollment in the study.1
The study excludes patients who have received any prior therapy for current lung cancer, including chemotherapy, or radiotherapy; those who have an EGFR mutation or ALK gene translocation; any condition requiring systemic treatment with either corticosteroids or other immunosuppressive medications within 14 days before randomization; active autoimmune diseases or history of autoimmune diseases that may relapse; or a history of interstitial lung disease, non-infectious pneumonitis, or uncontrolled diseases including pulmonary fibrosis, acute lung diseases, etc.
Investigators are assessing the dual primary end points of MPR rate and EFS by BICR, along with the secondary end points of pCR, overall survival, objective response rate, disease-free survival, and investigator-assessed EFS.
REFERENCES:
BeiGene announces the phase 3 RATIONALE 315 trial met primary endpoints of major pathological response rate and event-free survival for tislelizumab plus chemotherapy in patients with resectable non-small cell lung cancer (NSCLC). News release. BeiGene, Ltd. October 17, 2023. Accessed October 18, 2023.https://tinyurl.com/yzts832r
Comparing the efficacy and safety of a new additional treatment with tislelizumab in non-small cell lung cancer (NSCLC). ClinicalTrials.gov. Updated March 2, 2023. Accessed October 18, 2023. https://tinyurl.com/bdfyx2ps
Roundtable Roundup: Lung Cancer Molecular Testing and ALK-Targeted Treatment
January 18th 2025In separate, live virtual events, Vincent K. Lam, MD, and Chul Kim, MD, MPH, discuss molecular assays and treatment options for a patient with metastatic non–small cell lung cancer (NSCLC), with participants.
Read More