FDA Approves Ensartinib in ALK-Positive NSCLC
The FDA has granted ensartinib approval for adult patients with ALK-positive non–small cell lung cancer.
- Ensartinib has received FDA approval for the first-line treatment of anaplastic lymphoma kinase (ALK)-positive locally advanced or metastatic non–small cell lung cancer (NSCLC).
- Ensartinib is a next-generation oral tyrosine kinase inhibitor.
- Data from the phase 3 eXalt3 study (NCT02767804) support this approval.
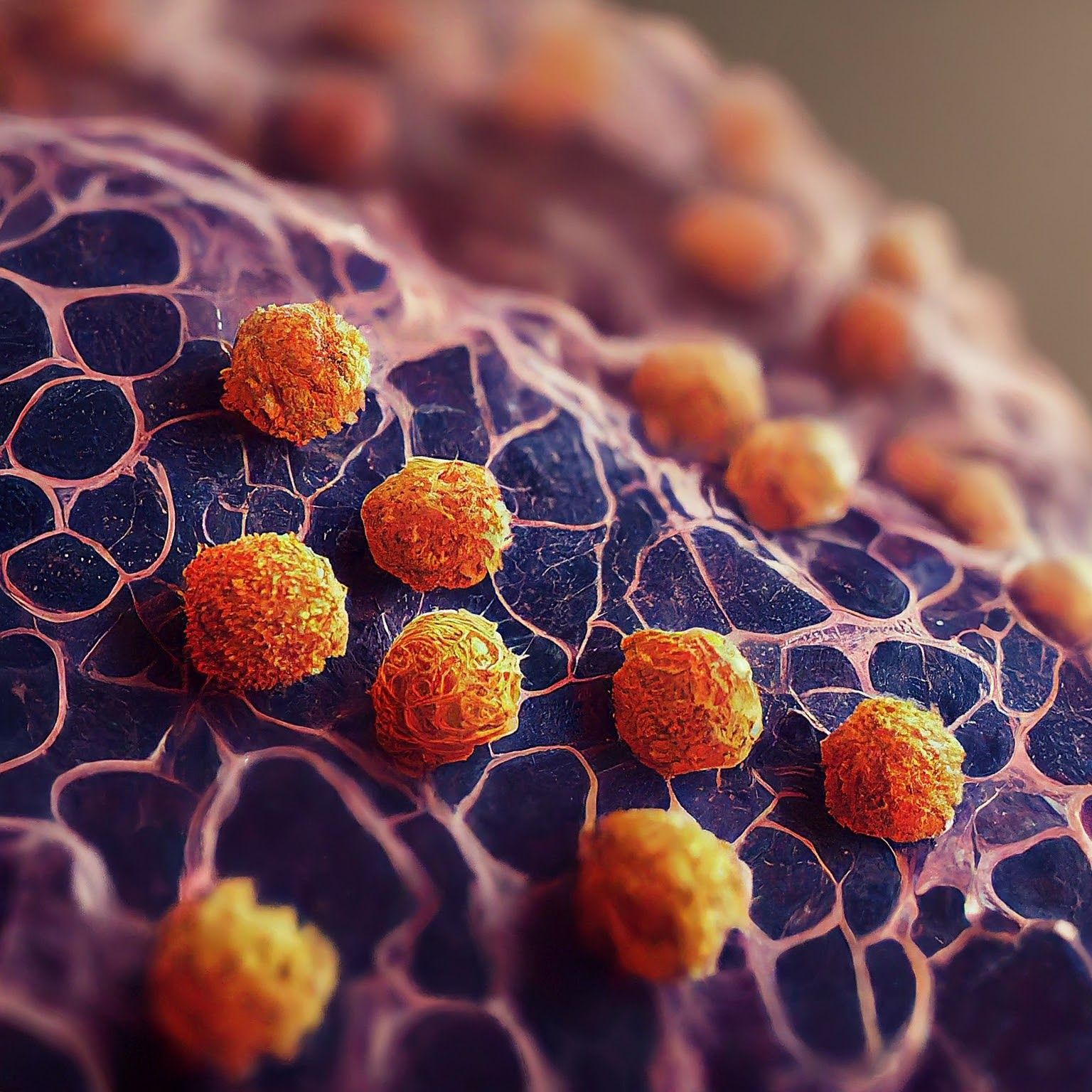
Microscopic image of non-small cell lung cancer - Generated with Google Gemini AI
The FDA has approved ensartinib for the first-line treatment of patients with ALK-positive locally advanced or metastatic NSCLC who have not previously received an ALK-inhibitor.1
Findings from the phase 3, randomized eXalt3 trial published in JAMA Oncology support this regulatory decision. The trial’s primary end point of progression-free survival (PFS) was met with ensartinib leading to a significantly longer median PFS than compared with crizotinib (Xalkori) at 25.8 months vs 12.7 months.2 The confirmed intracranial response among patients with brain metastases was 64% with ensartinib vs 21% with crizotinib.
For safety, the most common adverse effects (AEs) related to ensartinib included rash (67.8%), increased aspartate aminotransferase (37.8%), increased alanine aminotransferase (48.3%), pruritus (26.6%), nausea (22.4%), constipation (20.3%), edema (21.0%), anemia (14.0%), vomiting (11.9%), increased blood alkaline phosphatase (13.3%), increased blood creatinine (14.0%), increased γ-glutamyl transferase (13.3%), and decreased appetite (11.2%). While the majority of AEs were grade 2 or lower, grade 3 rash was observed in 11.2% of patients and was managed with dose modification. Additionally, 11 patients (7.7%) had serious treatment-related AEs.
For crizotinib, the most commonly observed AEs included toxic liver effects, nausea, edema, and constipation. Further, 9 patients (6.1%) experienced serious treatment-related AEs.
About the eXalt3 Trial
In the open-label eXalt3 trial, 290 patients with advanced, recurrent, or metastatic ALK-positive NSCLC who had not received prior treatment with an ALK inhibitor were enrolled. The study was conducted at 120 centers in 21 countries.
Patients were randomly assigned in a 1:1 fashion to receive either 225 mg of oral ensartinib once daily or 250 mg of crizotinib twice daily. Patients continued to receive treatment until disease progression or unacceptable toxicity, and no crossover was permitted. At the physician’s discretion, treatment could continue beyond progression.
The primary end point of the trial was blinded independent review committee-assessed PFS, and secondary end points included systemic and intracranial response, time to central nervous system progression, and overall survival.
REFERENCES:
1. FDA approves ensartinib for ALK-positive locally advanced or metastatic non-small cell lung cancer. News release. FDA. December 18, 2024. Accessed December 18, 2024. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-ensartinib-alk-positive-locally-advanced-or-metastatic-non-small-cell-lung-cancer
2. Horn L, Wang Z, Wu G, et al. Ensartinib vs crizotinib for patients with anaplastic lymphoma kinase−positive non–small cell lung cancer: a randomized clinical trial. JAMA Oncol. 2021;7(11):1617–1625. doi:10.1001/jamaoncol.2021.3523
Roundtable Roundup: Lung Cancer Molecular Testing and ALK-Targeted Treatment
January 18th 2025In separate, live virtual events, Vincent K. Lam, MD, and Chul Kim, MD, MPH, discuss molecular assays and treatment options for a patient with metastatic non–small cell lung cancer (NSCLC), with participants.
Read More









