Scheduling Tool Improves Infusion Center Efficiency
Coordinating appointments between the physician office suite and infusion center improved dramatically with the use of a scheduling optimization tool at the Cowell Family Cancer Center in Traverse City, Michigan. Specifically, the investigators observed a 6% reduction in median office-visit time and a 43% reduction in patient wait time in the infusion chair before infusion began.
The CFCC infusion suite was experiencing challenges during the midday peak period, when the nursing staff was busy with a steadily growing number of patients. Additionally, the staff had so much to do that they frequently missed lunches and finished the workday late. Many infusion centers face similar challenges, creating an urgent need for solutions that use existing resources more efficiently. Scheduling optimization, grounded in advanced data science, is based on a data-driven analysis of operations. The technique relies on the concept ofheijunka, the Japanese word for “leveling.” Heijunka evens out the peaks and valleys of patient flow throughout the day. Leveling the flow is the key to reducing wait times for chairs, addressing the patient demand, and reducing strain on nursing staff.
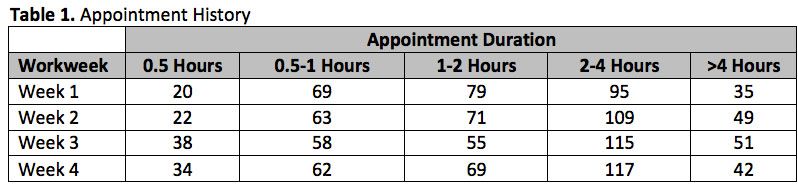
CFCC’s multidisciplinary team, including frontline staff from the scheduling department, leadership members, infusion nurses, and a nurse practitioner, implemented the optimization technique. The team extracted a data set from the electronic medical record (EMR) that included the history of completed patient appointments over the previous 4 months, excluding cancellations and no-shows. The analysis produced a 4-month operational breakdown of appointments, showing duration and volume. A snapshot of the analysis for a 4-week sample is shown inTable 1.
The operational analysis was further developed to produce an optimal volume mix for each day of the workweek, factoring in constraints such as chair availability, nurse staffing, hours of operation, and operational limitations such as infusion pharmacy hours. The optimal volume mix was then translated into scheduling templates that were incorporated directly into the EMR’s scheduling component and balanced the workload among nurses. This helped move the infusion center to a more evenly loaded workday.
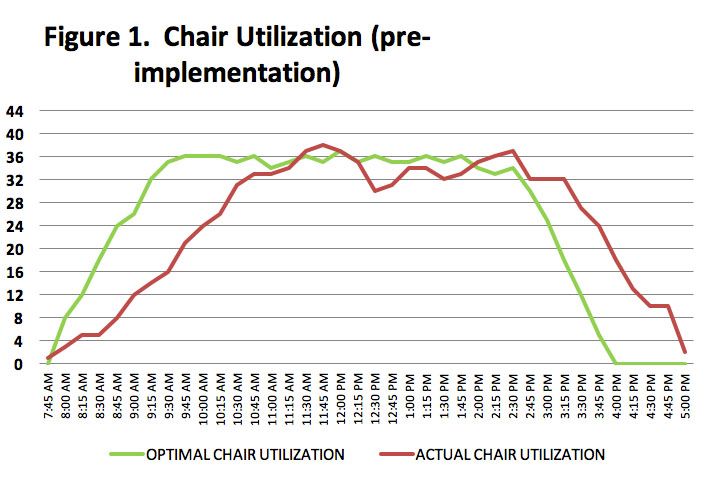
The graphs below, which compare a typical day before implementation with one after, illustrate the improved workflow that resulted from the rebalanced workload.
Pre-implementation
InFigure 1, the red line represents actual infusion chair utilization. It shows underutilization between 7:45 AM and 10:30 AM. Between 11:30 AM and 12:15 PM, optimal chair utilization, represented by the green line, was exceeded. After 2:15 PM, chair utilization was widely in excess of the optimum level, a sustained pace that contributed to a hectic, late finish to the workday. The day ended past 6:00 PM, stretching nursing activities well beyond operational hours.
Post-implementation
InFigure 2, the red line represents actual chair utilization. It shows a sharp increase in the morning until 9:30 AM but tracks closely with the green line, the optimal chair utilization curve. The remainder of the day was evenly loaded, with patient volume spread uniformly and following the optimal curve. After 9:30 AM, there was capacity to add patients to the schedule if needed. In addition, the nursing staff took scheduled lunch breaks and end their workday by 5:30 PM.
Results
After implementing the evenly loaded scheduling template, we reported a 15% increase in daily capacity at the infusion center. This translated to approximately 12 more patients per day without the addition of staffing, equipment, or labor hours.
Despite the increased daily volume, the center maintained a ratio of 7 or 8 patients per nurse per day. Typically, this ratio is higher9 to 12 patients per day—among infusion centers or physician practices offering infusion services. Thus, even though the daily volume was higher, we did not have to compromise on our commitment to safe care teams and safe patient care.
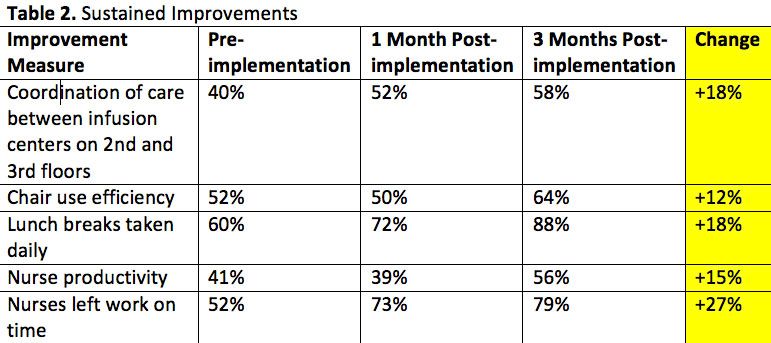
A number of patients have an appointment with their medical provider first, then proceed to the infusion suite for treatment, which requires coordination. The goal is to minimize patients’ wait time between the 2 same-day appointments and ensure a seamless patient flow. We surveyed the nurses about coordination of care, efficiency of infusion chair use, and whether they could take lunches daily and finish work on time. All those measures showed improvement, which is indicated in the “Change” column inTable 2.
Before, the nurses rarely took lunch breaks or finished the workday on time. Because of this project, we dramatically improved the nursing environment and have sustained the improvements. The floor nurses were surveyed before, 1 month after, and 3 months after implementation.Table 2summarizes the sustained improvements.
We created a tool that allows the staff to visualize the workday and preview the week ahead. As a result, staff can make informed decisions regarding adding patients, anticipate bottlenecks, and make other changes to the schedule. A snapshot of the visualization tool is shown inFigure 3.
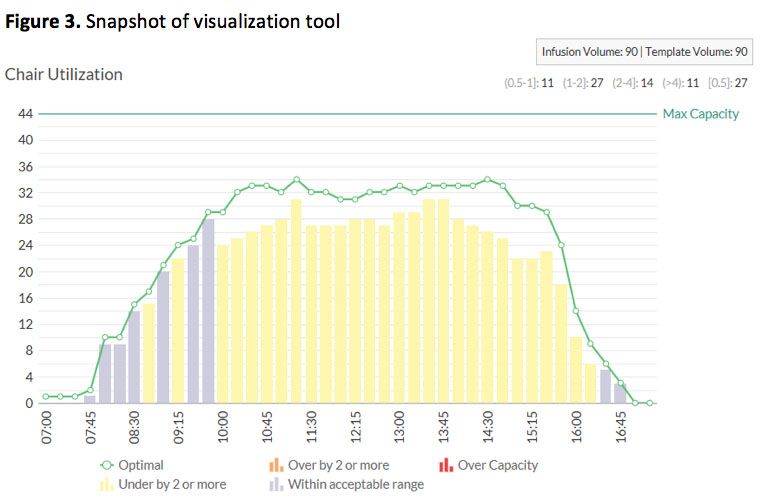
In this example, the patient volume maximum for the day is 90, and 90 patients have been scheduled. Between 7:45 AM and 9:45 AM, optimal capacity is neared, denoted by the green curve. Between 10 AM and 4 PM, there is potential to add more patients without disrupting the overall clinic flow. The day is expected to close at 5 PM.
Conclusion
Physician offices typically operate under heavy financial constraints, rising costs, and low reimbursementfactors that limit the ability to hire staff, support more overtime hours, expand facilities, and purchase additional equipment. Yet, it’s possible to see significantly more patients, increase revenue without incurring additional costs, and significantly improve throughput times to enhance the patient experience. Scheduling optimization offers a novel solution that delivers this Triple Aim by using a data-driven process typically applied only in industrial settings. It shows a new possibility to reimagine operations and dramatically increase the office productivity. Most important, it can be replicated by any practice, across a variety of settings, to maximize patient throughput.
The results were achieved without adding full-time employees, extending work hours, acquiring capital equipment, or physically expanding facilitiesfinancial headwinds that constrain most operations. In today’s operational environment, staff are commonly challenged to meet greater demands with fewer resources.
AI Continues to Push the Field of Radiation Oncology Forward
March 19th 2023In an interview with Targeted Oncology, Matthew Manning, MD, FASTRO, discussed the many radiation oncology tasks that have been improved with AI and its prospective utility in cancer diagnosis and treatment decisions.
Read More
ACCC Releases New Oncology Practice Transformation and Integration Center (OPTIC) Resource Library
December 23rd 2022The Association of Community Cancer Centers is announcing the release of a new tool intended to facilitate education and adoption of new clinical and technological advancements in diagnosis, staging, and treatment of cancer.
Read More