Roundtable Discussion: Treating DTC in the Front Line
During a virtual Targeted Oncology Case-Based Roundtable event, Marcia S. Brose, MD, PhD, led a peer discussion about frontline treatment of a patient with differentiated thyroid cancer.

During a virtual Targeted Oncology Case-Based Roundtable event, Marcia S. Brose, MD, PhD, director, Center for Rare Cancers and Personalized Therapy and director, Thyroid Cancer Therapeutics Program at Abramson Cancer Center, University of Pennsylvania, led a peer discussion about frontline treatment of a patient with differentiated thyroid cancer.
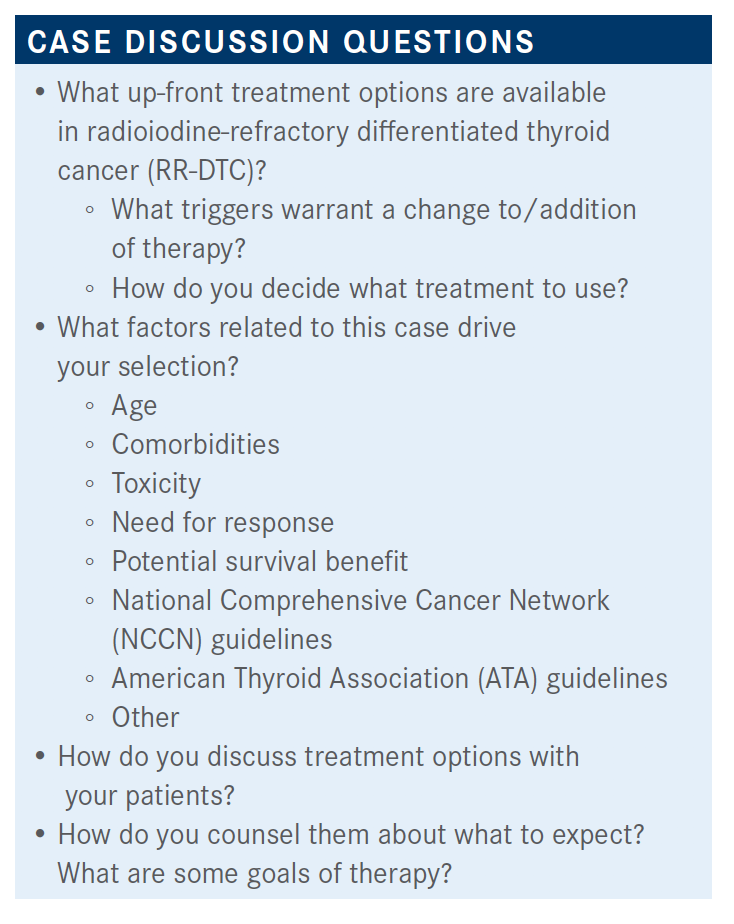
BROSE: What factors usually drive your treatment the most?
NEENOS ALNOOR, MD: I think for me it’s comorbidity.
YACOUB G. FAROUN, MD: I think a response rate and the duration of response [(DOR) are] important here provided that it’s a high dose of lenvatinib [Lenvima] up front, but later on we might reduce the dose. It depends on the] tolerance [of the patient], but DOR and response rate are important factors.
BROSE: I agree with the response rate being important, especially in a symptomatic patient. Interestingly, in a patient who is not symptomatic—unlike other cancers that are really aggressive—with thyroid cancer, I tend to [look at data for] progression-free survival [PFS] and DOR because I find that most of my patients are asymptomatic. If youvdon’t get them until they are symptomatic, you don’t have a choice. But if you have an opportunity to intervene before their disease gets symptomatic, [starting therapy is] a good thing to do because once they develop symptoms, they don’t always completely reverse on systemic therapy.
What [helps is to] get a sense of when you think they are about to get symptoms and try to jump in before that happens. You can predict if they are going to have symptoms [if] they have bone metastases, the next one could be a fracture. Or are they symptomatic because they have a lot of pleural disease, and now are at risk of symptoms from that perspective? You have to try to imagine what’s going\ to probably [affect] them first.
As an oncologist, I find the NCCN guidelines are much more informative and useful than the ones that are written by ATA, probably because the person who wrote them from ATA was looking at it more from an endocrine perspective where they don’t want to start anything [for] as long as possible. Sometimes that can mean the patients end up symptomatic. That can be a problem, which is one of the reasons why I believe oncologists need to be treating these patients, not the endocrinologists.
Right now, we have had the approval of sorafenib [Nexavar] and lenvatinib [in the front line] . If the patient has a high mutation load, microsatellite instability high, they could get pembrolizumab [Keytruda]. There are also BRAF inhibitors available. Right now, the BRAF inhibitors are phase 2 data. Pembrolizumab has the tumor-agnostic data.
BROSE: Do any [treatment options or trials] affect which therapy you would choose? How do you pick?
MICHAEL ROTKOWITZ, MD: I would just add that the data [help me pick]. They're all PFS [data], but I think [for lenvatinib it] is 19 months versus 11 months [with sorafenib]. I think there is a difference. They were both in placebo-based studies.
The biggest thing I discuss with patients is that the treatment tends to be a bit more bacteriostatic than bactericidal. The goal is to look for regression, but it’s really to slow progression so the stability of disease is not a negative notion; that’s what I try to warn patients. I think it’s definitely above all to do no harm. Dose modifications are pretty tolerable for both [lenvatinib and sorafenib], but the data support clinical benefit with lenvatinib. There was never a cross comparison between trials…but the data support lenvatinib for me.
BROSE: The other thing to know is that long-term patients [will] probably end up getting both, so I would caution against being too negative about the sorafenib. I would also choose lenvatinib first, but sorafenib might still be in their future. You have to tread lightly a little bit. You can say why you pick one first but to make sure you don’t knock any of them [completely] because later on sorafenib does have some activity; it may be that they will end up needing it because maybe their blood pressure and other things will make it impossible for them to tolerate [lenvatinib].
I think if my point [of treating before symptoms arise] is well taken, most people are not going to need big shrinkage or symptom relief, although there is definitely that with lenvatinib and even with sorafenib—but more importantly, we want this to be a marathon, not a sprint. We try to keep patients on a dose as long as possible, but we still need to maximize that dose to get the best effect possible. We don’t want to dose reduce to the point where this is an inactive agent.
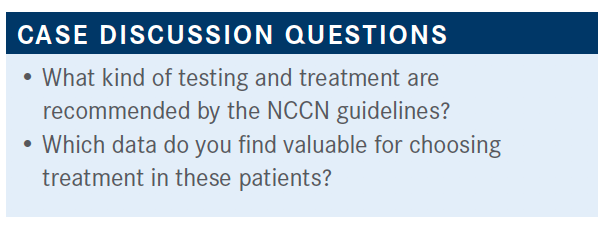
BROSE: We do genetic testing…we do somatic testing. What do we look for? Patients can have TRK fusions and [they] can be in up to 20% [in thyroid cancers]. They can have RET fusions, which can also be quite prevalent in papillary thyroid cancer. They can also have BRAF mutations. Papillary thyroid cancer has 50% [rate of] BRAF mutations. Would I use a BRAF inhibitor in the first line? Absolutely not. There are phase 2 data only, many fewer patients, and the response rate was not that great. It was about 20% or 26%.
I would never replace one of our phase 3–proven, FDA-approved drugs with a BRAF inhibitor up front, but I want to know whether that’s going to be an option because down the line…it might make the difference between whether I want to try to push through some of those toxicities or switch to another agent. Doing genetics up front, I think, is absolutely important. Sorafenib and lenvatinib are both approved. I think lenvatinib was approved a bit over sorafenib from the NCCN [perspective], just on the basis of the response and some of the other data.
The SELECT trial [NCT01321554] was designed shortly after the DECISION trial [(NCT00984282) of sorafenib] was designed, but the randomization was made 2:1.1 Lenvatinib’s starting dose was 24 mg daily versus placebo. One difference [from the DECISION trial] was that it had a central review—so in other words, patients were not put on unless the central reviewers felt that they were absolutely progressing. I had a patient [who] turned it down based on that; it seemed like the reviewers were really [trying] to see if there’s any way possible you could get 5 RECIST [criteria] nodules that would not be progressing. If they could do that, the person did not get on. I’ll tell you how we know that in the data in a second.
The other difference was, because this trial came second, it allowed for 1 line of VEGF [vascular endothelial growth factor] receptor inhibitor therapy. We were able to get data both in the front line and also in the second-line setting. The end points were similar to the DECISION trial [of PFS as the primary and response rate, overall survival (OS), and safety as secondary end points]. There was a stratification for age of 65 years. This became important later in the trial.
The PFS hazard ratio was 0.24 [95% CI, 0.17-0.35; P <.0001], and [a median of] 19.4 months with lenvatinib and placebo with 3.7 months. So clearly a very active drug, and I think even though you don’t do side-by-side comparisons, the magnitude of this response is what got everybody excited to use lenvatinib.
There was a beautiful response rate of 64.8%—clearly a really nice response, very good for our symptomatic patients. The only thing that you should be careful about is if you have a patient who has invasion into the trachea; although this is good and will shrink things fast, I think there is also a high risk of [the patient] getting a fistula. If you have an advanced patient, you might go with the slower [treatment] instead of the faster [treatment]. That’s what we have been doing in our practice with our advanced patients.
The rate of all grades of adverse events [AEs] was 97.3%, and grade 3 or higher was 75.9%. A majority of those were from grade 3 or 4 hypertensive episodes. That was the vast majority of that toxicity. Serious AEs [were observed in] 49.8% of patients; again, mostly because of hypertension. The placebo had 22.9% of patients with serious AEs… meaning that these were patients who were likely to get sick. Almost a quarter of them at a serious AEs due to their underlying disease.
Hypertension—that’s what you need to know about lenvatinib, and most importantly, you want to have patients well controlled on hypertensive medication before the start [of treatment]. In addition, if they already have hypertension, you want to make sure that you have a way [to check on them] in the first 24 to 48 hours of being treated and if they are checking the blood pressure daily. If you don’t check them in the first 24 to 48 hours, the emergency department will, because they often can get spikes in their blood pressure that cause them to be symptomatic, [such as] fairly severe headaches.
I gave lenvatinib to patients on my Thursday clinic, and that was a disaster because every weekend I started a patient, I was then talking them through their blood pressure management. What we ended up doing was starting all of our patients on a Monday for the simple reason that we knew that they would have 5 days of being able to reach us in the clinic or my nurse practitioner to manage that. Then we can quickly advance to hypertensive regimens and try to keep them out of the emergency department, instead of having them go back and forth, because emergency departments will always tell them to stop the lenvatinib; the blood pressure goes down and then you’re right back at square one.
JOSE A. SILVA JR, MD: In terms of the hypertension related to the VEGF-mediated pathway, is there any specific antihypertensive class that you favor using for controlling the blood pressure?
BROSE: That’s a good question. In general, the calcium channel blockers tend to work well, but because there’s also proteinuria at a significant rate in patients receiving lenvatinib, we tend to use an angiotensin converting enzyme [ACE] inhibitor first. We will use an ACE inhibitor often at every 12 hours, but the peak of the blood pressure happens at 10 hours, so they might take a morning dose of an ACE inhibitor; maybe before dinnertime they take the calcium channel blocker, and then take the second ACE inhibitor at night.
The other thing is that I tried to stay away from amlodipine because a lot of people are having trouble with swelling in their legs, so I’ll try to use something else. It’s a question of management. With ACE inhibitors you have to manage the cough. Some patients are much happier with a bit of a cough that they can ignore, and they sometimes pick it based on symptoms themselves because they don’t like the swelling that they get in their legs. Sometimes I would even e-scribe it and tell them [if they need to] go pick it up; it’s already there at the pharmacy when they are ready for it. Very few patients don’t need blood pressure medicine; about 20%.
SILVA: I am getting this with one of my patients [with ovarian cancer] on lenvatinib right now. I am going to review her chart tomorrow to see what we are doing right now. In endometrial, the doses of lenvatinib can be quite high. I never had a patient on 24 mg, but 14 mg seems to be my maximum; beyond that the patient starts having issues with either blood pressure or getting too tired.
BROSE: Are you doing the lenvatinib plus pembrolizumab or lenvatinib alone?
SILVA: This patient has Lynch syndrome and progressed on pembrolizumab first. She got to pembrolizumab by itself last year, then I moved her back to chemotherapy and she eventually progressed. She progressed on pembrolizumab monotherapy very quickly. Then she progressed on chemotherapy again. Now we have the combination approved for\ endometrial cancer, so we went back and used that, and she's responding.
BROSE: Yes, I have had a patient like that. I was doing an analysis for the PFS by age [in the SELECT trial] because I wanted to talk about it at a geriatric conference. We were looking at the AEs, and it was what you would expect for the most part—pretty even, a bit more comorbidities in the older patients and a bit more dose reduction in the older patients. Then I realized it didn’t really matter if we did not know how active it was. The Kaplan-Meier curves were pretty much superimposable. No matter what the age was, there were the same risks and benefits as far as lenvatinib goes with these criteria.
The OS curves by age were overlapping because we had crossover. When patients progressed at 2 or 4 months, they were able to get the lenvatinib. [After] crossover, the older patients had a statistically significant OS benefit. That means delaying this crossover by 2 or 4 months was enough for them to die of their disease at a higher rate. Why was that? Well, when they get older and they have other comorbidities, they don’t tolerate progression as well as a younger person; they don’t have as much buffer and margin for error. So because of this, all of my patients over 65 are going to start on lenvatinib. It was an unexpected result. I think everybody would have expected the older patients, given all of what I said about hypertension, to do worse. As it turns out, they didn’t. These patients started at 24 mg of lenvatinib, though we are more likely to require dose reductions, either to 20 mg or a bit lower.
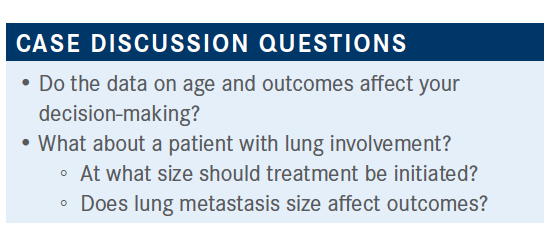
GABOR VARADI, MD: The age data are really interesting and impressive. Size [of metastases for initiation of treatment] is usually 2 or 3 cm.
I also wanted to ask you, both in sorafenib and mainly in lenvatinib, [how] to keep this 24-mg dose. I mainly use, for example, lenvatinib in patients with liver cancer, but even 8-mg or 12-mg doses they can hardly tolerate.
BROSE: In general, I tend to try to start higher. It is true that a lot of people got nervous putting it at a higher dose.
I agree with the 2-cm [size for lung metastases]. We have talked a bit about different criteria for size. It didn’t matter what size patients had [in the SELECT trial]. There was definite improvement of PFS and OS with lenvatinib.
There was a study [done] because everybody was afraid of starting patients at 24 mg. So, the study [NCT02702388] looked at starting patients at 18 mg instead….As it turned out, this was negative.2 [Compared with] the 24-mg dose, noninferiority was not demonstrated. In other words, 18 mg was inferior. When they started people on the 18-mg dose… the patients had a statistically different response. They responded last. The end point was response at 6 months. They clearly had responded last, but interestingly the grade 3 treatment-emergent AEs were the same between 24 mg and 18 mg.
This was a blinded study. Everybody treated the AEs the same way. So if you’re not biased in knowing that somebody’s on 18 mg versus 24 mg, and you address the AEs in a consistent way, you can get a better result still starting at 24 mg with the same safety for the patient. That was not what any of us expected when they did the study. Everybody expected safety to be improved and overall response would be virtually the same, but the opposite was true. So that’s the great thing, as this was a blinded study.
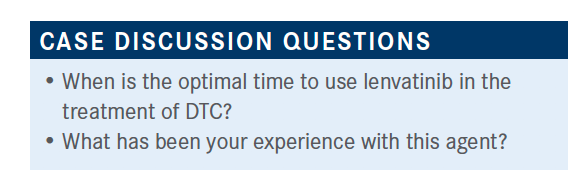
JOSHUA STRAUSS, MD: Lenvatinib is now becoming approved for so many other different cancers, so I think that’s certainly something speaking toward its use here, too. We’re becoming much more comfortable using it, whether it’s an endometrial cancer or hepatocellular carcinoma, and [it’s approved] in renal cell carcinoma. I think in general it’s becoming a drug that is so much more comfortable for medical oncologists who may not see so many of these types of patients.
BROSE: Yes, and the same thing happened when we started with sorafenib. It really has changed significantly.
SILVA: Be watchful for heart failure. I had a patient who had a completely normal ejection fraction who was responding nicely, and all of a sudden, his ejection fraction was 15% and he was in heart failure.
BROSE: I had 1 patient like that. One of the things that I started doing, even with sorafenib and even if patients are asymptomatic, is getting an echocardiogram before I start [treatment] sometimes, especially if they have a lot of hypertension. Then I’ll get them [another] at 6 months or a year to check in and make sure it’s not slipping without me knowing. I don’t do it on everyone, but there are some people that I do. Interestingly, I had one woman that was off the drug for about 8 months, then had no choice but to go back on it. We started a low dose and she got another year out of it.
VARADI: What are you doing to those patients who develop QT prolongation?
BROSE: Interestingly, we don’t have that much in lenvatinib. That’s common in other drugs that we use in thyroid cancer, but not in lenvatinib or sorafenib.
References:
1. Schlumberger M, Tahara M, Wirth LJ, et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med. 2015;372(7):621-630. doi:10.1056/NEJMoa1406470
2. EISAI announces topline results from Study 211 supporting 24 mg as the appropriate starting dose for Lenvima (lenvatinib) in patients with differentiated thyroid cancer. News release. Eisai. August 11, 2020. Accessed March 3, 2021. https://bit.ly/3bbrDlq
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen