Real-World Data Confirms Efficacy of Tafasitamab for R/R DLBCL
In an interview with Targeted Oncology, Bruce Feinberg, DO, discussed the importance of real-world data, highlighting recent findings on tafasitamab for the treatment of patients with relapsed/refractory diffuse large B-cell lymphoma in the United States.
Bruce Feinberg, DO

While traditional clinical trials lay the groundwork for new approvals of agents, understanding their effectiveness in broader, more diverse patient populations remains crucial. According to Bruce Feinberg, DO, real-world data is needed to confirm the efficacy of an agent and its role in clinical practice.
At the 2023 American Society of Hematology Annual Meeting, Feinberg, vice president and chief medical officer at Cardinal Health, delved into the real-world performance of tafasitamab (Monjuvi), an immunotherapy for the treatment of patients with diffuse large B-cell lymphoma (DLBCL). Two studies showed encouraging results with the agent and showed that response rates observed with tafasitamab, as well as its safety profile, in the real world mirrored those observed in clinical trials.1,2
Notably, these positive outcomes extended to underrepresented patient groups often excluded from initial studies.
In an interview with Targeted OncologyTM, Feinberg discussed the importance of real-world data, highlighting recent findings on tafasitamab for the treatment of patients with relapsed/refractory DLBCL in the United States.
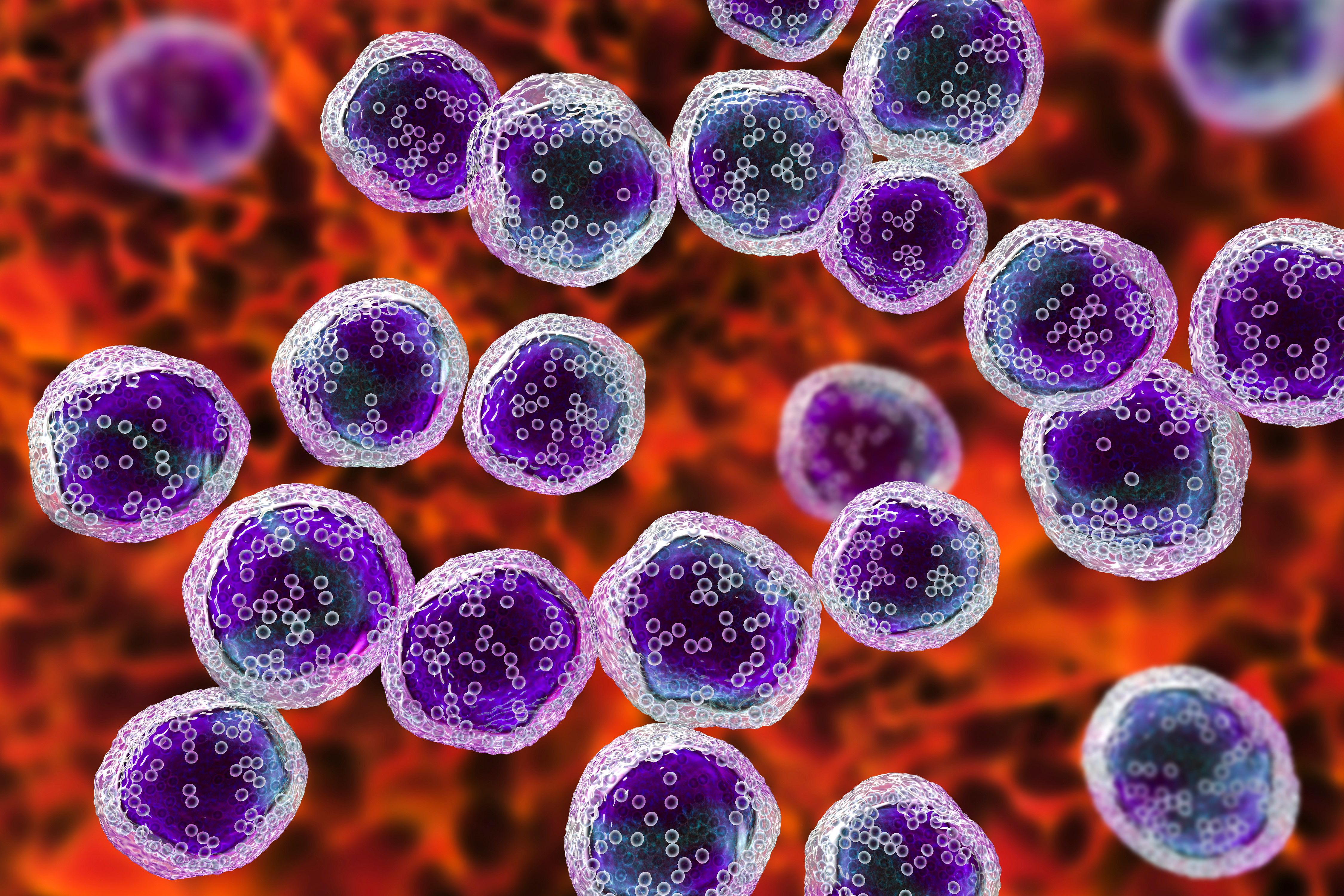
lymphoma cells : © Dr_Microbe - stock.adobe.com
Targeted Oncology:Can you elaborate on the background of immunotherapy and how it connects to this research?
Feinberg: Immunotherapy, in general, is the modern era of medicine, and certainly cancer medicine. If we think about cancer medicine, we most typically think about chemotherapy. That era of chemotherapy lasted 50 to 60 years. In the 2000s, a new era began with immunotherapy. Immunotherapy predominantly was around using antibody-based drug therapy. Could antibodies bind to cancer cells and with the immune system then, as a result of that antibody binding, helped destroy those cancer cells?
One of the original drugs of the first big 3 that came out of Genentech for that purpose was rituximab [Rituxan]. Rituximab is an anti-CD20 antibody, and these are cell surface receptors. These are proteins that are transmembrane, and when you bind to that protein, you can affect signaling from outside the cell to inside the cell that can then lead to cell death. Anti-CD20 antibodies became huge in the treatment of B-cell malignancies. Many lymphomas and types of leukemia are impacted by this. It was a blockbuster drug for decades.
We are now kind a few eras down from that birth of immunotherapy, and there are still questions on have we tapped out on all the possibilities of immunotherapy? There are other transmembrane proteins, which are being explored. One of them, also present in most B-cell lymphomas, is CD19. That is based on how it is clustered in the gene. These names are just symbolic determinations that came down from bench chemistry. These anti-CD19 antibodies are the basis for [chimeric antigen receptor] T cells, which has gotten a tremendous amount of attention over the past few years. But they were also the basis for drug development and in particular, the drug that was part of this research, tafasitamab. Similar to the way in which anti-CD20 antibodies like rituximab were being used in combination with chemotherapy, the question raised is, could we combine an anti-CD19 antibody with another active agent working by a different mechanism? That agent is lenalidomide [Revlimid], and that work was proven to be active.
What can you discuss about tafasitamab and its approval?
I was part of that original work that led to the FDA approval of tafasitamab, and that was my first involvement with working with the agent. Once the drug comes onto the market, a few things happen as part of the modern era as well. Often, drugs are approved for accelerated approval, which is shortening the time because historically it was taking 12 years to have a drug go from the bench to the bedside where it is being administered. How do we shorten that time down?
One of the ways was the FDA looking at accelerated approval, especially for novel agents, something like a CD19 antibody, which was brand new. But there is a requirement if 1 is going to do an accelerated approval, and that there [has to be] postmarket research that the FDA requires in order to prove that when you use that drug in much larger numbers of patients. It will also affirm that what we did see is valid. Postmarket research is what this research is a part of, proving that in the real world, not in this very specific clinical trial population, this drug works as we expected it to work, there were no unexpected signals that suggested a problem, and that it works across all types of patients.
Can you discuss the underrepresentation of patients in clinical trials?
One of the problems we have with clinical trials is that for them to have become the gold standard that they are, there is a strictness about the way they are conducted. That often makes the patients who are part of those trials not representative of the general population. It became clear and in fact, ASCO [the American Society of Clinical Oncology] itself stated in 2016 at the ASCO Annual Meeting that the patients in clinical trials are healthier, younger, less diverse, and not necessarily representative of the patients who are being seen day-to-day in doctors offices.
One of the things that we can be doing about that is looking at real-world evidence. That would be looking in the real world at patients being treated outside of a clinical trial; 97% of the patients with cancer are happening outside of a clinical trial. We are making decisions based on a 3% unrepresentative population, and we hope it is going to apply to the 97%. We underrepresented women, we underrepresented by age, [and] we underrepresented by ethnicity, and these under representations could be meaningful, so we do work like this.
Can you discuss the 2 abstracts looking at tafasitamab you were a part of at ASH 2023?
In 1, we wanted to see that the drug did perform, as the trial suggested it would, both in terms of its toxicity profile and its efficacy profile. Then, we also wanted to know that it performs that way in more typical patients. To give an example, I was in practice for 25 years before I became chief medical officer at Cardinal, and in my cancer practice, we were excited about a new drug in colon cancer. The year was 1999 and the new drug was irinotecan. The trial came out of [Memorial Sloan Kettering Cancer Center] in New York City. It demonstrated the first new drug activity that we had seen in 20 years in colorectal cancer. Doctors in my practice were so excited, the patients were so excited, and it was almost as if everybody was just waiting on pins and needles hoping the patient would live long enough and be well enough that they could get the new drug. The drug came out after the ASCO meeting and got approved, [and] became available. Every doctor in my practice had at least a patient waiting, hoping to get that drug.
My first patient ended up in the intensive care unit 3 weeks later. I was on rounds that weekend and in the bed next to my patient was my partner's patient who had received the exact same drug at the same time that first week it was available. For me, in the new era of electronic medical records, we had just implemented our own in 1999 in my practice. I am asking questions. Are we seeing something that we did not see in the clinical trial? I said to the doctor who was responsible for looking at data in electronic medical records, ‘You've got to take a look at this.’ We had 20 patients at that point who had just finished their first month of treatment, and 17 ended up hospitalized. We knew then there was a problem. When we looked at our patients vs the patients in the trial, the average age of the patient in the trial was 62 and in our practice, it was 72. What is the average age of colorectal cancer in the SEER national database? Seventy-two. The patients in the trial were younger. The standard drug is 5-FU [5-Fluorouracil]and in the trial, only 10% of the patients had had it. In our practice 100% had previously been treated with 5-FU.
We started to see all the differences between that real-world population and that trial population. We made a decision then, in the beginning of 2000, that based on that experience, there was a French way that drug was being given that seemed to be safer, and we converted. For that regimen, the way it had come out of Memorial Sloan Kettering, it was not until 2004, 4 years later, that the article ran in the [Journal of Clinical Oncology], suggesting that the experience in the trial may not be representative in the real-world.
The idea of real-world data, big data, finding out what's unlocked within this 97%, has now finally come to reality. The question is, how can you conduct research that allows us to truly compare what happens in the real-world to what happens in a clinical trial? Real-world datasets, like claims and medical records in general, do not allow the same measurements to be used as in a clinical trial. We do not scan patients every 8 weeks on a schedule. They get scanned more haphazardly. We are not dotting all the i's and crossing all the t's the way it is done in a trial. Part of this work is not just in terms of that it needs to be done because we need to get a more representative view. It is also about developing new methods that allow us to get those kinds of comparisons that allow us to compare apples to apples, not apples to oranges.
In these specific studies of tafasitamab, what real-world findings were observed in regard to overall response rate, complete response rate, etc.?
What we saw on the trial with tafasitamab plus lenalidomide is that in these patients, who at that point in the trial were relapsed/refractory patients, many with diffuse large B-cell lymphoma or sometimes just called large B-cell lymphoma, are cured with their initial treatment, which includes rituximab, CHOP [cyclophosphamide, hydroxydaunorubicin, vincristine (Oncovin), and prednsione], [rituximab], and that when they fail, if they were eligible, they would be autologously transplanted. That would cure half of those who failed. So a 70%, cure rate 60% to 70% with that frontline, and maybe half of them cured with then autologous transplant-based therapy as a high-dose intensification. Now, [we were] trying to figure out what you're going to do for that 20%.
It turns out that a lot of patients are not eligible for transplant. They have comorbid conditions, another thing that is not represented well within the clinical trial world because those patients are often excluded from eligibility to participate. It turns out there probably is a larger number of patients who are outside of that. The question is, can [we] meet that high bar? Can [we] get response rates in the 60% to 70% range? Can [we] get durable responses that usually are somewhat predicted based on high complete remission rates? What we saw were overall responses in more than 2/3rdsof the patients. We could not look at durability yet because this is a relatively new drug. What we looked at in the case of the trial data was at patients who were on the drug for 3 years. Being relatively new, we did not have that much of a time window. What we could say is that of the patients, there was a high response rate and of those responders, 82% were still on the drug. That likely will mean that those that level of response will even go higher, stable patients will become partial remissions [PRs], and those PRs will become complete remissions.
The problem with the numbers is that we are looking at a point in time snapshot that is not complete, but they are encouraging and consistent with what was seen in the trial. They were not only consistent, which is another interesting part of the research and why there's a second abstract, but they were consistent across these different, poorly represented subgroups. They were consistent in those who were Hispanic, Latin, African American, Black. We are not just seeing a phenomenon because those populations are often poorly represented in clinical trials for a whole host of reasons that would require a different exercise, but they also had similar, high levels of response, and durable responses. It is likely that we will be repeating this analysis in another year in order to get that longer term follow-up. If [we] were to match this point in time with the same point in time in the clinical trial, we will see consistent results with new data showing that that consistency applies across the various subgroups that are often poorly represented.
How does this safety profile compare with other agents in this space?
It is very similar and looks safe. One of the things that has made immunotherapy kind of the breakthrough that it was at the time is that we had this era of classical chemotherapy in the background. Now, we have drugs that are active that do not produce hair loss, do not produce nausea and vomiting, that are not toxic to the bone marrow, cause low blood counts, cause infections and bleeding or the need for transfusion. That's not present with immune-based therapies. Similarly, we're not seeing that in the CHOP/rituximab experience, which was combining it with chemotherapy. In this particular study, it was combined with another immunomodulatory drug, called lenalidomide. We did not see any of those classical chemotherapy type [adverse] effects. We did see [adverse] effects, and the [adverse] effects were not different than what we saw on the trial. For the most part, they were not serious in that there was the level of grade 3 and 4, were not significantly elevated above the trial levels, and we weren't seeing deaths from the drug which would be a grade 5.
What are the key messages that oncologists should take away from this research and managing patients who are in the receiving stage?
Those in the community should not discount their own experience. Doctors every day are making observations about new therapies and new drugs they are using, and new regimens they are using. There is almost like a whisper that happens where we start seeing modifications, where even though a drug was approved at this dose, at this schedule, doctors in the community within a year or 2 are doing it differently. They are giving it, instead of 3 weeks out of 2 weeks out of 3. So there's the extra week off in the 6-week time period, or 4-week time period, or they're doing a 20% ad hoc dose reduction.
These are problematic in a way, because we make these wholesale changes, we do not know if it is going to compromise the activity. What we need to do is not make them wholesale. In a way that is not. That's not what's the word I want for this in a way that we want to treat it like research, make the observation and then apply that observation in a research design to validate it. Rather than just doing these kinds of ad libs and ad hoc changes. That may seem to work. But we're not looking at the full picture.
REFERENCES:
Saverno K, Zimmerman Savill KM, Feinberg B, et al. Tafasitamab for the treatment of relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL) in the US real-world setting. Blood. 2023;142(suppl 1):265. doi:10.1182/blood-2023-173143
Epperla N, Nastoupil LJ, Zimmerman Savill KM, et al. Real-world use of tafasitamab (tafa) for relapsed or refractory (R/R) diffuse large B-cell lymphoma (DLBCL) among racial and ethnic minorities in the United States. Blood. 2023;142(suppl 1):2415. doi:10.1182/blood-2023-174543
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More