Piotrowska Looks at Amivantamab and Mobocertinib for Patients With Rare Driver Mutations in NSCLC
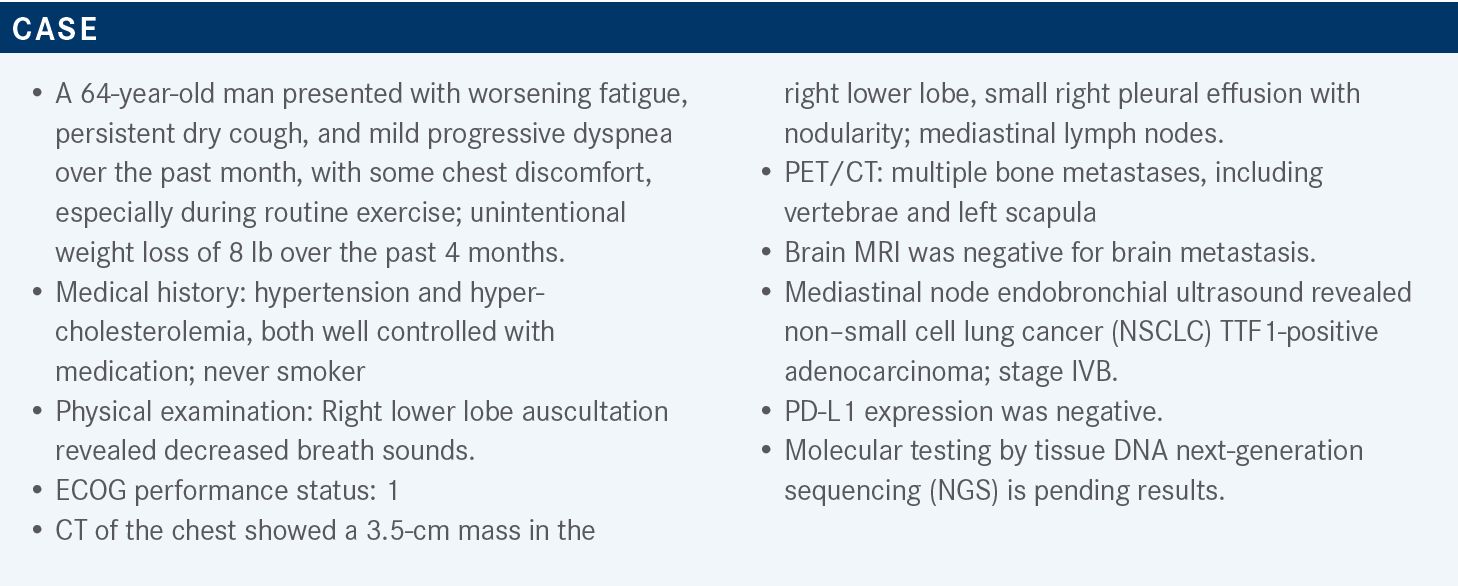
During a Targeted Oncology case-based roundtable event, Zofia Piotrowska, MD, MHS, discussed molecular testing for actionable mutations and recommended treatments for a patient with non–small cell lung cancer and an EGFR exon 20 insertion.
Zofia Piotrowska, MD, MHS
Massachusetts General Hospital
Assistant Professor, Medicine
Harvard Medical School
Boston, MA

Targeted OncologyTM: What is the protocol for molecular testing in lung cancer?
PIOTROWSKA: The updated NCCN [National Com-prehensive Cancer Network] guidelines are for patients with advanced or metastatic NSCLC.1 Certainly, if they have a nonsquamous tumor, they should be having molecular testing, and importantly, this testing should be conducted as part of broad molecular profiling now.
Of course, it also should include PD-L1 testing, but I think what the NCCN is trying to move away from is just doing individual tests and not doing the broad NGS, recognizing that sometimes we do the specific gene tests as part of a rapid panel and then move on to the NGS. But the point is you want to make sure you’ve covered all these targets even in squamous carcinomas.
Consider the molecular testing. We certainly have rarely seen these types of targets in squamous tumors. We’ll chat briefly about the fact that MET exon 14 [METex14] skipping [alterations], for example, can be seen in squamous and sarcomatoid histologies. I would say that most patients, at some point even the [patients with] squamous [disease], should have molecular testing performed.
[We have] all these different mutations and rearrangements, the latest kid on the block being KRAS G12C, but an important point is that we have the targeted therapies for all these patients. For patients who don’t have one of these targets, we usually act, at least in part, based on the PD-L1 status.
Again, molecular testing should include EGFR, ALK, ROS1, BRAF, NTRK, METex14 skipping, RET, and KRAS alterations.1 It should be conducted as part of broad molecular testing. PD-L1 testing—although I think that’s generally kind of reflex now, from pathology—is still important as well. The broad panels minimize tissue use and potential wastage, and they help us identify rare driver alterations, and, ultimately, they’re important for good patient care.
Another key point: For patients for whom you’re sending NGS, the DNA NGS can be limited in the detection of certain fusions and METex14 skipping, so consider adding RNA NGS.1 Some of the companies are doing both; but in some cases, it may just be DNA NGS. Whatever test you’re using, know whether they’re doing both. If they aren’t, and you have [a patient in whom] you’re looking for a driver and you don’t find anything on the DNA NGS, I think it’s worth sending the RNA NGS. Plasma testing should also be considered, and I tend to send this now at the time of diagnosis in parallel with the tissue, but certainly a staged approach is reasonable, too.
If…you’re waiting for molecular testing to come back, in general—and this is something I follow in my clinic—regardless of the PD-L1 status, if you have a patient who has not had the molecular testing done yet and you’re planning to give them either immunotherapy alone or chemotherapy plus immunotherapy, it’s recommended to withhold the immunotherapy until you get the NGS testing back.1
The reason is that there is a concern that if you start patients on immunotherapy and then identify, for example, an EGFR or ALK alteration and try to switch them to the targeted therapy, there is increased risk of toxicity. For example, there is an increased risk of pneumonitis with osimertinib [Tagrisso] and hepatitis with some of the ALK inhibitors, if patients have had prior immunotherapy.2
If you have a patient in those rare cases where they just can’t wait to start treatment, generally the recommendation is to give them a cycle of chemotherapy alone without the immunotherapy. Then once you have the NGS [results] back, you can always dial in the immunotherapy with cycle 2.
If you’re giving someone immunotherapy, should you wait a certain period of time before giving a targeted agent?
The answer is we don’t know. There are some retrospective data specifically from the EGFR space looking at the rates of toxicities with osimertinib, and it looked like 3 months was a marker, where the rates were much higher if immunotherapy had been given with it in 3 months and lower if you waited longer than that.
I don’t think it’s a magic number, and in those situations, the longer you can wait, the better. At the same time, I’ve had situations where you just can’t wait. The patient had immunotherapy, but they had an EGFR mutation and a ton of brain metastases—that might be a situation where you take the risk. The goal is to try to avoid that situation and certainly try to wait at least a few months if you can.
What do the NCCN guidelines say regarding a patient’s PD-L1 status?
The way that I read their guidelines is “regardless of PD-L1,” but I think sometimes the discussion comes down to other things beyond just PD-L1 [expression], like the smoking status. If you have a heavy smoker with high PD-L1 [expression], in that situation, many of us would say, “Let’s just go ahead with the immunotherapy.” If you have a patient with no smoking history, like this one, sometimes those patients will have a targetable alteration and high PD-L1 [expression], and we will still want to treat them with a targeted therapy.
Please discuss the various EGFR mutations clinicians should be aware of.
The key point here is that not all EGFR mutations in lung cancer are the same. The most common types of EGFR mutations are the EGFR exon 19 deletions and L858R point mutations, and those are the ones that are sensitive to drugs like osimertinib and that we treat with first-line osimertinib. Those make up about 85% of all EGFR mutations in lung cancer, but between 5% and 10% of all EGFR mutations are exon 20 insertions.3 The key thing is that historically these have not been sensitive to first- and second-generation EGFR inhibitors.
Even osimertinib has little activity in these mutations, and very poor responses are seen. But there’s a diverse group of insertions here, and this is where I was saying it can get tricky on NGS reports, because sometimes you just get the amino acid sequence, and it’s up to [the clinician] to remember exactly whether that falls in exon 20 or not. So if you’re unsure, it’s worth asking the pathologist or phoning a friend, as some of these are more common than others, but they can span amino acid positions 761 to 774.
One key point is that targeted [polymerase chain reaction]–based approaches may underdetect this because of the heterogeneity of these mutations, so NGS testing is the best way to detect these.1 The one type of exon 20 insertion that’s important to remember is the FQEA insertion, because these are early in the exon and tend to behave like exon 19 deletions and are like classic EGFR mutations, but the majority of these are not.
Another somewhat minor point is that T790M mutation also occurs in exon 20, but that’s not an exon 20 insertion. That’s the resistance mutation that we treat with osimertinib. There are also some other mutations in exon 20, like S768I, that can be sensitive to standard EGFR inhibitors. So what we’re looking for is insertions in exon 20, and structurally these are different because this pushing of the C helix into the active confirmation causes steric hindrance that blocks the classic EGFR inhibitors from binding.4
How have new drugs affected the treatment landscape?
This is a new [treatment setting], and I think it’s one that takes a little time to get familiar with. The double dose of osimertinib is something that’s been explored in clinical trials, but it has modest activity, I would say.5 The response rate was 24%, and progression-free survival [PFS] was about 8 or 9 months in a small study of only about 20 patients. It is an option, but [compared] with amivantamab [Rybrevant] and mobocertinib [Exkivity], I think now that we have the data, [the reason for using amivantamab or mobocertinib] is a little stronger.
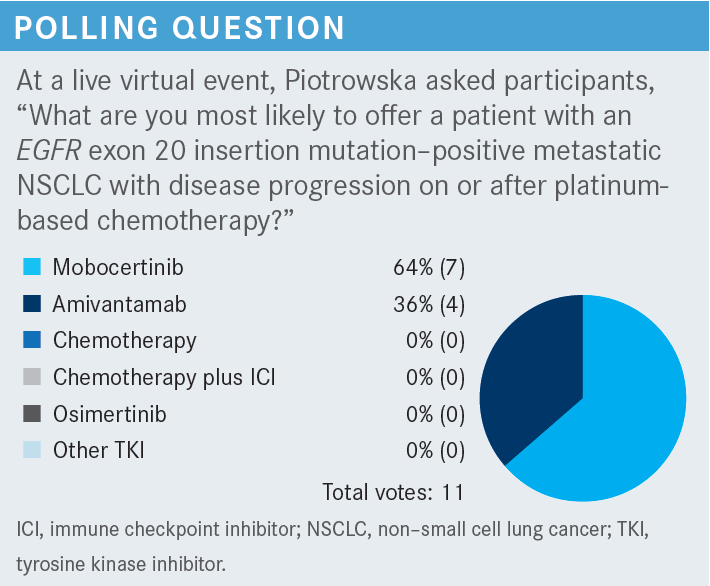
The NCCN guidelines for EGFR exon 20 insertion mutation–positive cancers show that the first line for these patients is still chemotherapy or chemoimmunotherapy. The approvals we have are only in the postchemotherapy setting. For patients like the one discussed today who progress on chemotherapy, you have 2 choices: amivantamab and mobocertinib, both approved within the past year or so.6,7 The nice thing about these drugs is that they have different mechanisms of action, so if you look at these 2 options, you can use them both in either sequence. We don’t know exactly what the optimal sequence here is, but we do now have 2 approved therapies for patients with these mutations.
What data show the efficacy of amivantamab therapy in this patient population?
Amivantamab is given [intravenously and is a] bispecific antibody that targets EGFR and MET in the patient’s tumor. It is approved only in patients with EGFR exon 20 insertion mutations who have progressed on platinum chemotherapy. The approval comes from this cohort from the phase 1 CHRYSALIS trial [NCT02609776], and you can see this was a standard phase 1 dose escalation.8
They established the RP2D [recommended phase 2 dose] to be this weight-based dosing: either 1050 mg for less than 80 kg or 1400 mg for more than 80 kg. Initially, for cycle 1, it’s given weekly, and afterward it’s given every other week. In CHRYSALIS, [cohort D comprises] patients with EGFR exon 20 insertions.
There were 81 patients with EGFR exon 20 insertions.8 In terms of demographics, about 53% of [these patients] were nonsmokers, 47 patients had a smoking history, and the majority had adenocarcinoma. Interestingly, many of these patients were pretreated and had a median of 2 prior lines of therapy. All of them had had prior chemotherapy, about half had prior immunotherapy, and only a small number had prior EGFR inhibitors—largely first-, second-, or third-generation EGFR inhibitors—because these data were before these drugs were approved, so [we] didn’t have access to other exon 20–targeted therapies.
Efficacy for amivantamab among these patients showed a response rate of 40% by blinded independent review [95% CI, 29%-51%]. The clinical benefit rate here was 74% [95% CI, 63%-83%]. The median duration of response was 11 months, and median PFS was 8.3 months.
Sometimes what comes up is that there may be some slight differences in how these patients respond, depending on where in the exon the mutations arise. There are some hints that near-loop mutations may have a little more sensitivity, but I would say let’s not get too bogged down in that. I think it’s important enough that we recognize these mutations as their own distinct entity rather than worry about exactly where in the exon they fall, until we have more data on that point.
What are the relevant safety signals for amivantamab?
[They] fall into a few categories.8 There are some dermatologic toxicities such as rash and paronychia, with rash seen in 78% of the patients. Looking at all the patients treated at the recommended phase 2 dose, there were mostly grade 1 and 2 toxicities, with few grade 3 toxicities. Paronychia was seen in 40% at a largely low grade, and there was some edema and hypoalbuminemia, which are related to MET inhibition. The other one to be aware of is infusion-related reactions, and about two-thirds of these patients will have infusion-related reactions. We had a patient in our clinic today who was starting and had an infusion-related reaction, but [importantly, these reactions] tend to occur… on day 1 of cycle 1. There are guidelines in the package insert for premedications with steroids for cycle 1, day 1, and cycle 1, day 2.9
The drug is given as a split dose between the first 2 days with the first infusion because that’s when the infusion-related reactions are most likely to occur. And even among patients who do have infusion-related reactions, generally when they come back on day 2 and [later], these don’t recur.
For [clinicians] who treat other nonlung cancers, I’ve been told this is more like a rituximab [Rituxan]-type reaction than it is like a paclitaxel [Taxol] hypersensitivity reaction, where you must keep worrying about it. I haven’t used rituximab myself in a long time, but I think the concept is the same.
I think this is something important to be aware of and to counsel patients about, but it is manageable. Also, it is important to warn and educate your nursing staff. Moreover, grade 3 toxicities were seen in 39% of the patients, but dose discontinuation related to treatment was only in 7%, and only 10% needed dose reduction.8
Which efficacy and safety data back up the use of mobocertinib?
Mobocertinib is the second agent that’s approved for EGFR exon 20 insertions, and this is, unlike the other intravenous antibody-based therapy, an oral EGFR inhibitor.10 This is also improved in the same kind of setting: postchemotherapy second line for exon 20 insertions. Mobocertinib was first developed specifically to target EGFR exon 20 insertions. The data for the approval come from this phase 1/2 study, again looking at a cohort of specifically [patients with] EGFR exon 20 insertions who had prior immunotherapy.
This group was 114 patients all with prior platinum chemotherapy.10 They had a similar patient population, similar breakdown, a little more never smokers, and, again, a heavily pretreated population with a similar distribution of prior therapies.
The efficacy with mobocertinib showed an objective response rate [ORR] by blinded independent review of 28% among these 114 patients [95% CI, 20%-37%], and ORR was 35% by investigator review [95% CI, 26%-45%]. The median PFS here was 7.3 months, but the median duration of response [DOR] was 17.5 months among those responders, and median [overall survival] was 24 months.
Again, ORR of 28% by blinded review and median DOR of 17 months. The main kind of toxicities to remember and be aware of are the [gastrointestinal] toxicities. Diarrhea is seen in 91% of these patients, including 21% who have grade 3 or higher diarrhea, so significant rates there.10
Forty-five percent of these patients had rash, although largely these were low grade, and again you can see paronychia. QT prolongation with this agent was seen in about 11%, but you can also rarely see cardiomyopathy or heart failure in about 3% of patients and interstitial lung disease or pneumonitis in about 4%, but these are all toxicities that we see with osimertinib as well.
Now, the mechanisms of action of these drugs are quite different, and the administration is different. Amivantamab is given intravenously initially with frequent visits, so again you give the split dose with cycle 1, day 1 and day 2, and then weekly visits for the first 4 weeks, and after that, it’s every other week.9 Whereas mobocertinib is an oral agent, but it’s given at 160 mg, with or without food.11
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Non-small cell lung cancer, version 3.2022. Accessed March 16, 2022.https://bit.ly/3G0Re06
2. Schoenfeld AJ, Arbour KC, Rizvi H, et al. Severe immune-related adverse events are common with sequential PD-(L)1 blockade and osimertinib. Ann Oncol. 2019;30(5):839-844. doi:10.1093/annonc/mdz077
3. Meador CB, Sequist LV, Piotrowska Z. Targeting EGFR exon 20 insertions in non-small cell lung cancer: recent advances and clinical updates. Cancer Discov. 2021;11(9):2145-2157. doi:10.1158/2159-8290.CD-21-0226
4. Vyse S, Huang PH. Targeting EGFR exon 20 insertion mutations in non-small cell lung cancer. Signal Transduct Target Ther. 2019;4:5. doi:10.1038/ s41392-019-0038-9
5. Piotrowska Z, Wang Y, Sequist LV, Ramalingam SS. ECOG-ACRIN 5162: a phase II study of osimertinib 160 mg in NSCLC with EGFR exon 20 insertions. J Clin Oncol. 2020;38(suppl 15):9513. doi:10.1200/ JCO.2020.38.15_suppl.9513
6. FDA grants accelerated approval to mobocertinib for metastatic non-small cell lung cancer with EGFR exon 20 insertion mutations. FDA. September 15, 2021. Updated September 16, 2021. Accessed November 8, 2022. https:// bit.ly/3UTkLwY
7. FDA grants accelerated approval to amivantamab-vmjw for metastatic non-small cell lung cancer. FDA. May 21, 2021. Accessed November 8, 2022. https://bit.ly/3Fgo8Ij
8. Park K, Haura EB, Leighl NB, et al. Amivantamab in EGFR exon 20 insertion-mutated non-small-cell lung cancer progressing on platinum chemotherapy: initial results from the CHRYSALIS phase I study. J Clin Oncol. 2021;39(30):3391-3402. doi:10.1200/JCO.21.00662
9. Rybrevant. Prescribing information. Janssen; 2021. Accessed July 21, 2022. https://bit.ly/3Y7RIbE
10. Zhou C, Ramalingam SS, Kim TM, et al. Treatment outcomes and safety of mobocertinib in platinum-pretreated patients with EGFR exon 20 insertion-positive metastatic non-small cell lung cancer: a phase 1/2 open-label nonrandomized clinical trial. JAMA Oncol. 2021;7(12):e214761. doi:10.1001/ jamaoncol.2021.4761
11. Exkivity. Prescribing information. Takeda; 2021. Accessed July 21, 2022. https://bit.ly/3Ph8AbK

Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More