Participants Discuss Frontline Immunotherapy Followed by ADC for Metastatic Cervical Cancer
During a Case-Based Roundtable® event, Ramez N. Eskander, MD, and participants discussed first and second-line therapy decisions for a patient with PD-L1–positive cervical cancer in the frontline metastatic setting.

Ramez N. Eskander, MD (MODERATOR)
Gynecologic Oncologist
Assistant Professor of Obstetrics, Gynecology, and Reproductive Sciences
UC San Diego Health
San Diego, CA

EVENT REGION Great Plains/Rocky Mountains
PARTICIPANT LIST Vinay Raja, MD | Shiven Patel, MD, MBA | Rao Mushtaq, MD | Benjamin Scheier, MD | Lin Hao, MD | Yan Ji, MD | Ariel Soriano, MD | Madhu Midathada, MD | Vinay Gupta, MD
ESKANDER: Is there a situation when you would not use pembrolizumab in conjunction with chemotherapy plus or minus bevacizumab?
RAJA: The data are compelling, so I would use it for all patients unless there is a contraindication. If the patient has an underlying immunological disorder, uncontrolled ulcerative colitis, Crohn disease, or rheumatoid arthritis, I would probably avoid it. Otherwise, I think this would be a go-to for me.
PATEL: Even with some autoimmune diseases, I’ve used it successfully. [I would not use it] if somebody could get a fatal exacerbation of myasthenia gravis or had a history of a liver or heart transplant. But it would be something dire like that for me to not use it.
MUSHTAQ: It’s the same for me. It has to be a vital organ transplant or uncontrolled, life-threatening multiorgan involvement autoimmune disease, not a well-controlled autoimmune disease.
ESKANDER: What factors do you consider when you decide to include or not include bevacizumab in frontline therapy for node-positive metastatic cervical cancer? Are you bevacizumab users in this population… or do you stick with chemotherapy or chemotherapy/IO [immunotherapy]?
SCHEIER: I think you wonder whether the benefit of the drug gets washed out when you’re using IO in the front line. I think if you’re using IO in the front line, I’m less compelled to add it and then use it in maintenance.
PATEL: I feel the exact opposite. I feel like across cancer, there is a lot of synergy between various VEGF agents and IO, so I try to use it any chance I get with anti–PD-L1 [therapy].
ESKANDER: KEYNOTE-826 [NCT03635567] built on a prior protocol, GOG 240 [NCT00803062], which was chemotherapy vs chemotherapy/bevacizumab, which showed a progression-free survival [PFS] and overall survival [OS] benefit.1 But KEYNOTE-826 left bevacizumab at physician’s discretion for some complicated study reasons. Of course, the BEATcc trial [NCT03556839] mandated bevacizumab with atezolizumab [Tecentriq], but that’s a separate anti–PD-L1 rather than anti–PD-1. Does anyone have any issues using bevacizumab or a bevacizumab biosimilar in your regions of the country in these patients? Some of these can be patients who are underfunded. Are there programs available for a regimen that clearly is quite expensive in your areas?
HAO: [In Colorado], I have no problems getting bevacizumab. I normally include it in the treatment unless the patient has an open wound, contraindication, or blood clots. Otherwise, I will use it routinely.
ESKANDER: Dr Ji, do you have any issues getting medications like this for your patients with cervical cancer?
JI: Not right now, but I wonder because in the KEYNOTE-826 study, the bevacizumab was not mandatory. Do you have any data on the 2 groups with or without bevacizumab?
ESKANDER: Yes, they’ve presented that. The patient cohort that receives bevacizumab appears to do better, but it is not appropriate because there are clinical variables that you could imagine may portend a patient who is not going to do as well clinically.2 Bevacizumab was omitted on the part of the physician. The trial was not intended to answer that question, but they did look at it because BEATcc mandated bevacizumab vs KEYNOTE-826, in which it was optional.
JI: We use atezolizumab/bevacizumab as a combination in hepatocellular carcinoma and in lung cancer. It sounds like that IO/VEGF combination has been showing that it is better than IO alone. But I’m not sure whether that is because of atezolizumab or is it because there is still a synergistic effect using pembrolizumab plus bevacizumab. But if it is an option and if the patient tolerates it fine, normally I don’t have any issue.
ESKANDER: Would you ever reserve pembrolizumab for second line, meaning you’re going to give chemotherapy/bevacizumab because you want to wait and hold on to pembrolizumab in case they recur and use pembrolizumab monotherapy based on the label?
JI: No, I normally don’t reserve it. I think most oncologists use the most effective treatments as a first line, because we see that it has an OS benefit, and there is nothing to argue you have to reserve it.
CASE UPDATE
The patient received pembrolizumab plus carboplatin, paclitaxel, and bevacizumab. She received maintenance pembrolizumab plus bevacizumab 15 mg/kg every 3 weeks and was monitored for treatment-related adverse events and therapeutic response. She was reevaluated every 3 months using stage-dependent imaging, complete blood counts, and a comprehensive metabolic panel.
DISCUSSION QUESTIONS
- What has been your experience with progression of disease in a patient with cervical cancer?
- What is the average time frame for disease progression in these advanced cases?
ESKANDER: What has been your experience in patients who experience progression on these systemic therapies? There are different buckets these patients are going to fall into, if they complete maintenance IO or if they experience progression on treatment. Of those who have used it, can I ask if you normally see these patients experience progression on maintenance therapy, or do you see them completing their maintenance therapy, say 2 years of it, and then experiencing progression after?
SORIANO: So far my patients have done well and right now they’re still on maintenance. The only change I’ve made with the maintenance is I’ve had to stop the bevacizumab because a patient was having recurrent hematuria because she was on anticoagulation at the same time.
ESKANDER: If you look at the Kaplan-Meier curves for KEYNOTE-826 for PFS while getting the pembrolizumab plus chemotherapy and bevacizumab at physician’s choice, the 12-month PFS rate was approximately 50%.3 Is that what you’re seeing in clinical practice or are you seeing better outcomes in clinical practice than what we saw on the trial? It sounds like Dr Soriano is alluding to some good responses.
SCHEIER: My experience has generally been [in] the 12- to 15-month or 12- to 18-month range, a bit better than the median in the studies but during maintenance therapy.
ESKANDER: Do you also check TMB [tumor mutational burden] on these patients? I’ve had some patients with TMB-high cervical cancers in clinical practice who have had dramatic responses to systemic chemotherapy/ IO and IO/bevacizumab maintenance. It makes me wonder. There is heterogeneity in these patients. Is that impacting some of the clinical outcomes that we see? Do you check TMB?
MIDATHADA: I think some of the next-generation sequencing results give the TMB as part of the panel, so I tend to get that whether I ask for it or not.
ESKANDER: But I’m then inferring that for these recurrent metastatic cervical cancers, you’re sending next-generation sequencing.
MIDATHADA: Yes.
ESKANDER: It sounds like that’s universal. Great.
CASE UPDATE
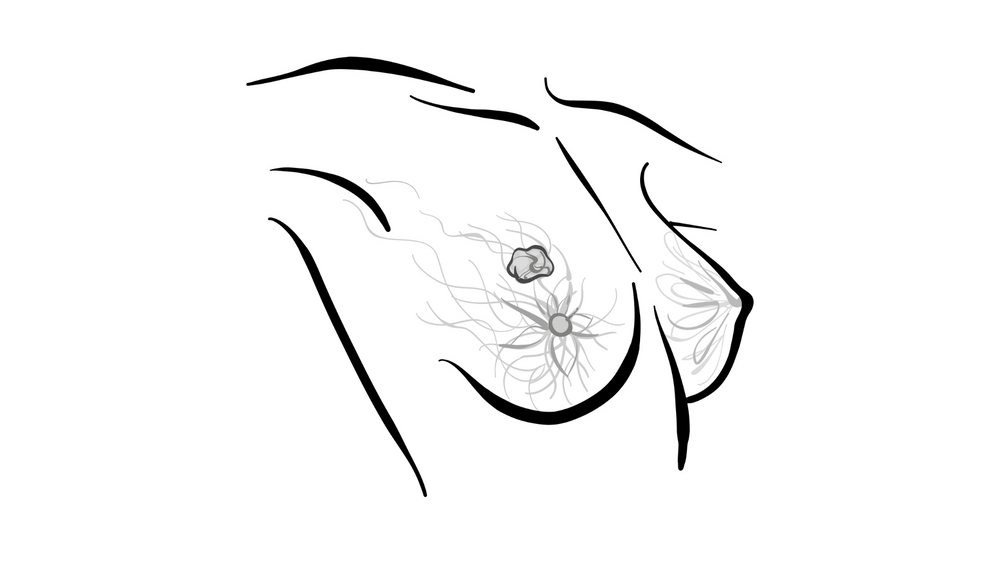
On reevaluation, the patient complained of dyspnea on mild exertion, persistent, nonproductive cough, and fatigue . Physical examination showed tachypnea, diminished breath sounds, monophasic wheezing, and scattered crackles. Contrast-enhanced CT of the chest, abdomen, and pelvis revealed a heterogeneously enhancing mass of 7.5 cm × 4 cm × 6 cm arising from the left upper lobe bronchus and bilateral hilar lymphadenopathy, with a short axis of 3 cm in diameter. A lung biopsy showed histopathology consistent with poorly differentiated, metastatic adenocarcinoma of the cervix. She had avid fludeoxyglucose F 18 uptake in the left upper lobe of the lung and hilum with no evidence of osseous or hepatic metastases.
DISCUSSION QUESTION
- What experience have you had with tisotumab vedotin (Tivdak) in the treatment of recurrent or metastatic cervical cancer?
ESKANDER: In the context of using the KEYNOTE-826 regimen, you have had a response, but they experience progression. Have you used tisotumab vedotin? What’s your impression in clinical practice? Are there any issues regarding safety? How are you managing the ocular aspects in the various areas in which you practice?
SCHEIER: We’re ramping up the use of antibody-drug conjugates [ADCs] across a variety of cancers.… We’re getting more comfortable. Even with the interstitial lung disease concerns in some drugs and with the ocular toxicities in others, we’re generally comfortable sending the preemptive consultation. I work in more of an integrated delivery–type model…and so it’s easy to get patients in with ophthalmology for some baseline assessments and easy communication and follow-up, so I think that’s well mitigated by that ease of referral for me.
ESKANDER: So is everyone very comfortable with tisotumab vedotin? Does anyone face issues with the ocular aspects of care?
JI: It is a burden for the patient. The patient I treated was in a rural area, and she had to make efforts to see the ophthalmologist. We got a very good ophthalmologist for her, but still [it requires] driving there every other cycle and getting all the eye drops. Every time we saw her she started complaining, but she still did it, which is pretty amazing. Supportive care and patient education play a very important role.
ESKANDER: What do you do in clinical practice if the patient walks in your office, they’re due for their tisotumab infusion that afternoon, and they say, “I didn’t see the optometrist this week. I don’t have any symptoms. I don’t have blurry eyes.” You look at them, and their eyes look good. Would you treat her, or would you say, “No, I’m going to defer you a week. You have to see the optometrist next week.” What are you doing pragmatically in your practice if that happens?
GUPTA: I have experience with other ADCs, and I have an ophthalmologist right next door [I can send them to].
ESKANDER: What if [the ophthalmologist] were not there because they’re on vacation?
GUPTA: I wouldn’t treat patients without regular eye exams. We make it very clear from day 1, it has to be done. That toxicity is very difficult. Once it happens, and you are the person who has brought it on that patient, it is very difficult to manage patient expectations after that. We like to educate and reinforce. We have an ophthalmologist who plays along very nicely with us.
JI: In this case, if she has no complaints and there is no conjunctivitis from my basic exam, I think I feel comfortable to treat her and I encourage her to see the ophthalmologist as soon as possible.
PATEL: I agree. This is different from other things like mirvetuximab soravtansine-gynx [Elahere], where it affects the cornea, and that’s harder to see unless you’re a dedicated eye doctor doing the eye exam. Most of us know what conjunctivitis and conjunctiva inflammation look like just by looking at the patient. I feel very comfortable, if they’re asymptomatic and their eyes look normal, to treat them. I would feel less comfortable with a different ADC that causes corneal problems, for example, for which I would have a much harder time because I don’t do slit lamp or fluorescein dye tests. It’s a different mechanism of action, a different toxicity from ocular toxicities of other ADCs, so I feel comfortable with this one.
ESKANDER: Has anyone had to take a patient off for ocular toxicity rather than disease progression?
MIDATHADA: I had to do that for 1 patient, but this was not on this drug, it was a different ADC for a different cancer.
ESKANDER: I want to clarify: Tisotumab can cause corneal [adverse events], including corneal ulcers, so it is part of the adverse event profile of the medication [From the Data4]. But…in clinical practice, I have had patients who live 2 or 3 hours away…. They drive in, the optometrist canceled their appointment the day before, they’re completely asymptomatic, and I have to make a decision whether I treat them or whether I subject them to waiting. If they’re completely asymptomatic, I’ll talk to them about the potential risk, but I have treated in that setting as well.

CASE UPDATE
The patient initiated tisotumab vedotin intravenously every 3 weeks and experienced a partial response . Her follow-up plan included monitoring for continued therapeutic response and tolerability , returning to the office every 3 weeks, and ophthalmologic examination for the first 9 cycles of therapy.
REFERENCES
1. Tewari KS, Sill MW, Penson RT, et al. Bevacizumab for advanced cervical cancer: final overall survival and adverse event analysis of a randomised, controlled, open-label, phase 3 trial (Gynecologic Oncology Group 240). Lancet. 2017;390(10103):1654-1663. doi:10.1016/S0140-6736(17)31607-0
2. Lorusso D, Colubo N, Dubot C, et al. Pembrolizumab plus chemotherapy for advanced and recurrent cervical cancer: final analysis according to bevacizumab use in the randomized KEYNOTE-826 study. Ann Oncol. Published online October 10, 2024. doi:10.1016/j.annonc.2024.10.002
3. Monk BJ, Colombo N, Tewari KS, et al. First-line pembrolizumab + chemotherapy versus placebo + chemotherapy for persistent, recurrent, or metastatic cervical cancer: final overall survival results of KEYNOTE-826. J Clin Oncol. 2023;41(36):5505-5511. doi:10.1200/JCO.23.00914
4. Vergote I, González-Martín A, Fujiwara K, et al. Tisotumab vedotin as second- or third-line therapy for recurrent cervical cancer. N Engl J Med. 2024;391(1):44-55. doi:10.1056/NEJMoa2313811