Novel CAR T-Cell Therapy Trial Advances to Third Cohort in Ovarian Cancer
A phase 1 trial evaluating FSHR-targeting CAR T cells for patients with ovarian cancer has dosed the first patient in its third cohort.
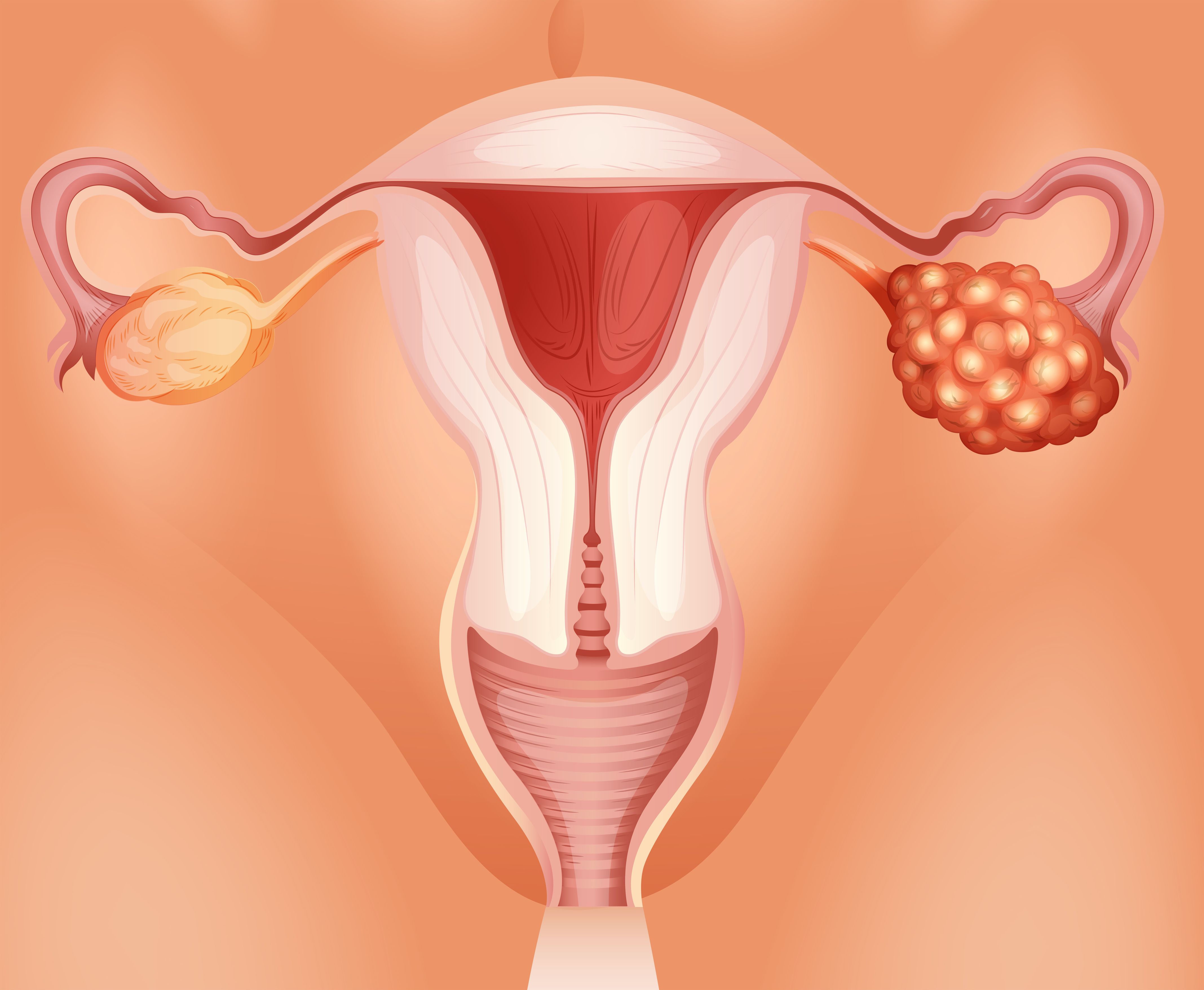
Illustration of ovarian cancer: © blueringmedia - stock.adobe.com
The first patient has been dosed with a novel chimeric antigen receptor (CAR) T-cell therapy in the third cohort of an ongoing phase 1 trial for patients with ovarian cancer.1
The first-in-human study, which is being conducted through a research partnership with Moffitt Cancer Center, is evaluating the safety of treatment with autologous T cells genetically modified to express a chimeric endocrine receptor (CER) targeting the follicle-stimulating hormone receptor (FSHR), with or without conditioning chemotherapy, in patients with ovarian cancer.1,2
In the initial cohort which included 3 patients, there were no dose-limiting toxicities (DLT) reported.The same was true for the second 3-patient cohort, where patients were given a CAR T-cell dose triple that of the first cohort.1
Following the required 1-month observation period to evaluate DLT and review all safety data, the trial has progressed to dosing its first patient in the third cohort. Here, investigators are administering a tenfold increase over the initial dose.
"With no dose-limiting safety issues observed in the first and second patient cohorts, we have advanced to the next cohort to evaluate a 10x higher dose compared with the starting dose. As the trial continues, our aim is to demonstrate the tolerability of our CAR T but we are optimistic and hopeful about seeing efficacy in this solid tumor—a challenging area for traditional CAR T therapies, which have shown efficacy mainly in hematologic tumors and lymphomas. We are very encouraged how the trial has progressed and our observation in one patient from the first cohort who had relative stability and even some mild improvement for well over a year after her infusion,” said Robert Wenham, MD, principal investigator of the study and chair of the Department of Gynecologic Oncology at Moffitt, in a press release.
About the Phase 1 Study
Patients will receive 1 infusion of FSHR T cells at varying dose levels and through different administration methods. For the intraperitoneal treatment arms, patients are being given these T cells at 5 dose levels, with the first group receiving a dose of 1 x 105. The infusion will be delivered through a thin membrane of the abdominal cavity. The second dose level will involve 3 x 105 FSHR T cells, again administered intraperitoneally. The third dose level will increase to 1 x 106 FSHR T cells, followed by a fourth dose level of 3 x 106 FSHR T cells. The fifth dose level will involve the highest dose of 1 x 107 FSHR T cells, all via intraperitoneal infusion.2
In the intravenous (IV) treatment arms, patients will receive the FSHR T cells in a similar fashion, given at the same dose levels but administered via IV infusion. Dose Level 1 will involve 1 x 105 FSHR T cells, followed by 3 x 105 at dose level 2. The third dose level will be 1 x 106 FSHR T cells, with the fourth dose level at 3 x 106 cells. The final dose level will consist of 1 x 107 FSHR T cells administered IV.2
Enrollment in the study is open to patients 18 years of age and older with a pathologically confirmed diagnosis of high-grade epithelial ovarian cancer, primary peritoneal cancer, or fallopian tube carcinoma. Patient’s disease must be serous, endometrioid, clear cell, mucinous, mixed epithelial, or undifferentiated and those with tumors that are substantially high-grade carcinoma and have focal elements of lower grade tumors or sarcomatous elements are eligible for enrollment. Further, patients are required to have measurable or detectable disease, carcinoma that expresses the FSHR antigen, an ECOG performance status of 2 or better, a life expectancy of at least 3 months, and adequate bone marrow, renal, and hepatic function.
Additional inclusion criteria requires patients to have had 1 previous platinum-based chemotherapeutic regimen for the management of ovarian, primary peritoneal, or fallopian tube carcinoma and at least 2 prior chemotherapy regimens, be considered platinum- refractory or resistant, deemed unlikely to have significant benefit from any standard therapies by the treating investigator, and have received no anticancer therapy in the 3 weeks prior to infusion with the T-cell. Patients must not have received prior immunotherapy with checkpoint blockade in the 6 months before the T-cell infusion, and those with a known germline or somatic BRCA pathogenic mutation should have received a prior PARP inhibitor and subsequent progression, unless they have a documented history of intolerance or inability to swallow oral medications.
While not required, patients are allowed to receive up to 6 additional prior chemotherapy treatment regimens or biologic/targeted therapy alone or as part of their treatment regimens. Further, patients must agree to undergo the placement of an interventional radiologically placed or surgically placed peritoneal port.
The primary end point is to determine the maximum tolerated dose of FSHR T cells and secondary end points include duration of response, duration of stable disease, and overall survival.
“This is highly unusual for a platinum resistant multiply treated ovarian cancer. A tumor biopsy showed necrosis and T-cell infiltration. Based on these findings, we recently submitted an amendment to the trial protocol to allow patients who may benefit from an additional dose. Generally, we expect higher cell doses to increase efficacy, although we also anticipate a second dose may further improve response rates and durability. We are proud of the progress to date and look forward to treating additional patients in the third cohort,” added Wenham in the press release.1
REFERENCES:
Anixa Biosciences initiates dosing in third cohort in its ovarian cancer CAR-T clinical trial. News release. Anixa Biosciences, Inc. November 18, 2024. Accessed December 13, 2024. https://tinyurl.com/mse3ntt8
Infusion of autologous T cells engineered to target FSH receptor in recurrent ovarian cancer. ClinicalTrials.gov. Updated November 29, 2024. Accessed December 13, 2024. https://clinicaltrials.gov/study/NCT05316129?tab=tabl










