Physical Performance Predicts Outcomes in CAR T-Cell Therapy in NHL
Poor physical performance in patients with non-Hodgkin lymphoma receiving CAR T-cell therapy was linked to worse survival and increased risk of neurotoxicity in a cohort study.
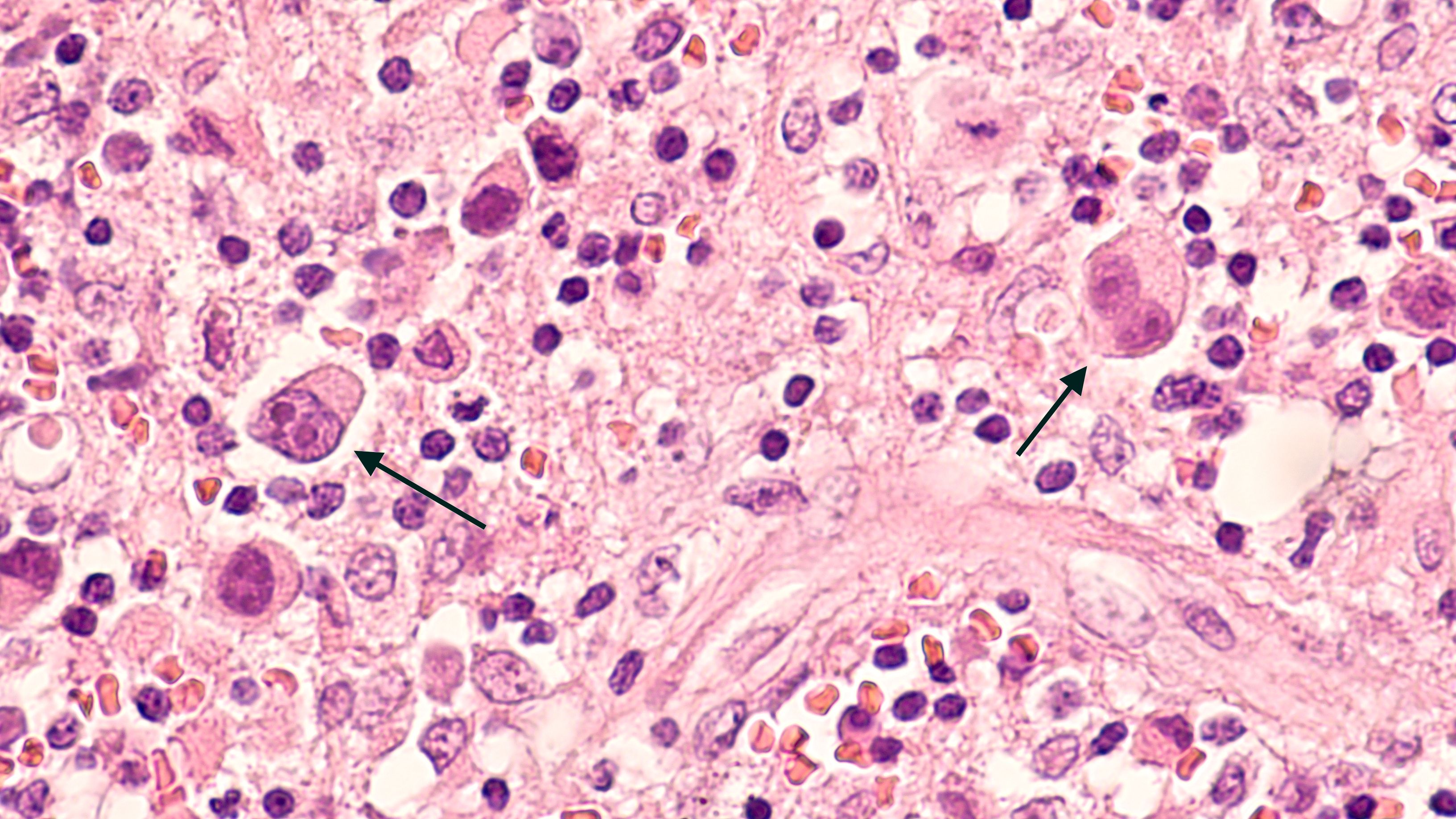
Lymphoma | Image Credit: © David A Litman - www.stock.adobe.com.jpg
A retrospective cohort study presented at the 2025 Tandem Meeting highlighted the prognostic significance of physical performance in patients with non-Hodgkin lymphoma (NHL) undergoing chimeric antigen receptor (CAR) T-cell therapy. Those with impaired physical function exhibited reduced overall survival and a heightened risk of immune effector cell-associated neurotoxicity syndrome (ICANS), underscoring the need for pre-treatment assessments to optimize patient selection and management strategies.1
An increased risk of ICANS was observed in patients who recently fell (odds ratio [OR], 5.2; 95% CI, 1.3-20.5; P = .02) and who weren’t able to balance on their left leg for 10 seconds (OR, 2.6; 95% CI, 1.1-6.2; P = .04). On this, presenting author Megan Herr, PhD, an associate member in the Department of Medicine at Roswell Park Comprehensive Cancer Center, said during the presentation, “These 2 measures, together, take less than a minute to implement. They’re easy, they’re cheap, and we can predict who is going to get neurotoxicity.”1
Of patients treated with axicabtagene ciloleucel (axi-cel; Yescarta) who had ICANS vs those who did not, 59% and 55%, respectively, were unable to balance on their left leg for more than 10 seconds. Of those who were treated with tisagenlecleucel (tisa-cel; Kymriah), 82% and 29%, respectively, were unable to balance. Of patients treated with axi-cel who had ICANS and who did not have ICANS, 26% and 0%, respectively, had a recent fall. Of those who were treated with tisa-cel, 27% and 13%, respectively, fell recently.
Patients with an assistive device (HR, 2.6; 95% CI, 1.3-5.2; P <.01), a positive Romberg test (HR, 3.1; 95% CI, 1.2-7.7; P = .02, and less than 5 of 5 strength (HR, 2.3; 95% CI, 1.2-4.5; P = .01) all showed reduced overall survival on an adjusted model. Of patients with elevated CAR-HEMATOTOX scores and at least 2 adverse physical functions, 1-year OS was 9% (P = .0002).
“[Patients who received CAR T] who have adverse physical performance have worse OS and are at higher risk for ICANS. Our proposed scoring system for CAR-T recipients improves identification of patients at risk of these unfavorable outcomes,” Herr stated.
The trial evaluated data from 91 patients who had NHL between 2018 and 2023; 56% of patients were older than 60 years at adoptive cell transfer, 67% were male, 89% were White, 96% had diffuse large B-cell lymphoma, 62% were treated with axi-cel and 38% with tisa-cel, 82% received fludarabine and cyclophosphamide, 72% were treatment resistant at ACT, and 81% had a Karnofsky performance status of 70.
CAR T treatment resulted in complete responses (CR) in 45% of patients and 55% did not achieve a CR, cytokine release syndrome (CRS) of any grade occurred in 64% of patients, ICANS of any grade occurred in 50%, severe ICANS was noted in 18%, and at 1 year, 57% of patients were alive.
Physical function measures included recent falls within the past 6 months, gait speed, strength and motor deficits, the Romberg test, baseline and peak heart rates, assistive device, self-reported pain or neuropathy, balance on right and left legs, and recovery time, among others.
The study authors noted 2 previously established indices that correlate with OS after CAR T-cell therapy—CAR-HEMATOTOX and CT-CI.2,3 CAR-HEMATOTOX established platelets, absolute neutrophil count, hemoglobin, C-reactive protein, and ferritin as indices, and CT-CI established diabetes, hepatic abnormalities, pulmonary dysfunction, renal insufficiency, infection, and body mass index as indices. In both the original paper and in this presented study, the CAR-HEMATOTOX and the CT-CI was not associated with ICANS, however, 1-year OS was associated with CT-CI in the original study but not in this presentation’s study population.









