Management of Early Stage Hodgkin Lymphoma Requires “Balancing” Individual Risk
When choosing therapy for patients with early stage Hodgkin lymphoma, considering risk scoring systems and Deauville criteria for PET-adapted therapy are key conditions for optimizing survival rates, according to Ranjana H. Advani, MD.
Ranjana H. Advani, MD

When choosing therapy for patients with early stage Hodgkin lymphoma, considering risk scoring systems and Deauville criteria for PET-adapted therapy are key conditions for optimizing survival rates, according to Ranjana H. Advani, MD, who discussed the topic at the National Comprehensive Cancer Network (NCCN) Virtual Congress: Hematologic Malignancies, held October 9-10, 2020.1
“To understand prognosis is to understand how risk is defined,” said Advani, who is the Saul Rosenberg Professor of Lymphoma and physician leader of the Lymphoma Clinical Care Program at Stanford Cancer Institute in Palo Alto, California. Definitions of risk will vary based on which scoring system is used, such as the NCCN criteria, the German Hodgkin Study Group (GHSG), or the European Organisation for Research and Treatment of Cancer.
Advani said individual scoring system definitions of risk overlap2 ; however, it’s important to be aware of the difference between them. “As we apply results of trials…we have to understand the characteristics of the patients who have enrolled on these trials so that we can apply these results to an appropriate patient population,” she said. “The minute you have 3 sites of [nodal] involvement—[such as] bilateral neck and mediastinum—it suddenly becomes unfavorable by the [GHSG] criteria but remains favorable by the other 2.”
This is further demonstrated by looking at patients with bulky disease of 10 cm or more, which would be considered unfavorable risk per the NCCN criteria whereas both European systems would characterize the disease as favorable risk. “The point is that one sleeve does not fit all, and you have to individualize therapy, taking into account risk factors.”
Goals of Therapy
Advani went on to detail expected survival rates in patients with early-stage Hodgkin lymphoma who are treated with standard-of-care therapy, which includes involved-field radiotherapy (IFRT) plus 4 cycles of ABVD—or Adriamycin [doxorubicin],bleomycin,vinblastine, anddacarbazine. In stage I or II nonbulky disease, clinical trial data indicate freedom-from-progression rates over 90% and overall survival (OS) rates of up to 96% at 12 years3; in patients with bulky stage II disease, failure-free survival is around 85% and OS around 95% for the same relative period.4 However, some data, such as those from the NCIC-H6 trial (NCT00002561), show that patients with nonbulky disease may achieve comparable results with 4 or even 2 cycles of chemotherapy alone.5
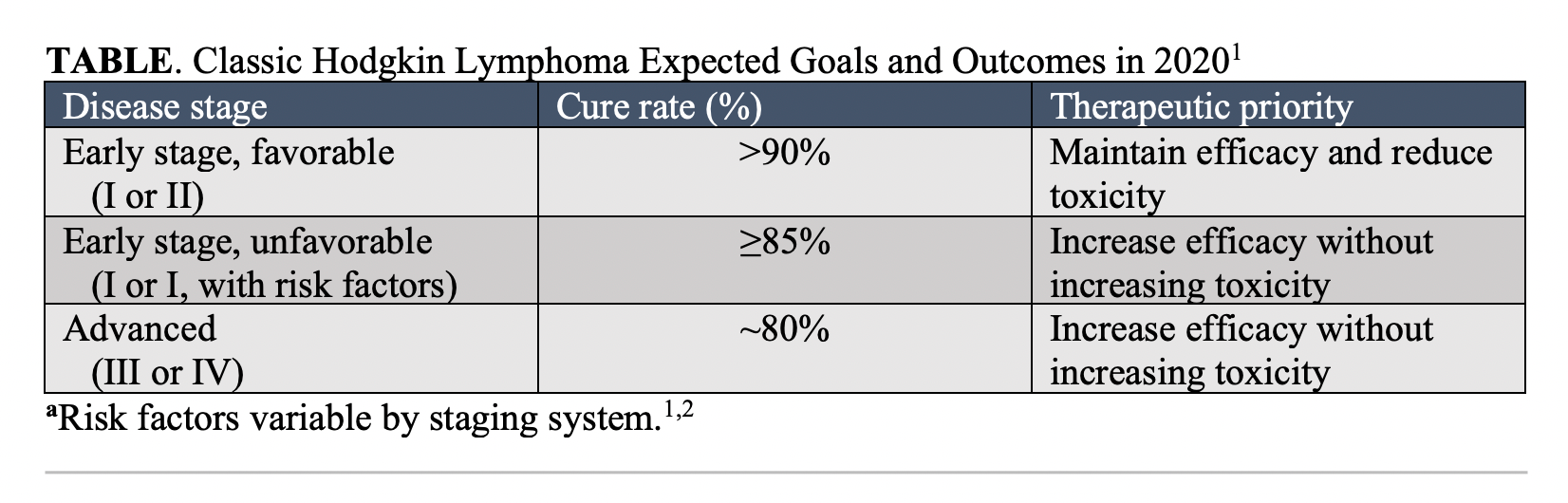
“In 2020, the goals of therapy in early stage favorable [disease] is a cure rate of 90% or higher,” Advani said. “The therapeutic priority is to maintain efficacy and reduce toxicity.” For patients with early stage unfavorable disease, cure rates are currently around 85% and the goals of therapy are for increasing efficacy without increasing toxicity. For patients with advanced-stage Hodgkin lymphoma, she said cure rates are lower, around 80%, and the goals of therapy are similar to those of patients in the unfavorable-risk disease category (TABLE1).
Honing Combined-Modality Therapy
“Fine tuning” of combined-modality therapy (CMT) has come into favor, whereby clinicians’ goals revolve around avoiding giving “too much” therapy to those patients who have favorable-risk disease and giving “too little” to those who are considered unfavorable, said Advani.
Long-term efficacy data from the GHSG trial HD10 (NCT00265018) showed that similar rates of progression-free survival (PFS) and OS were observed in patients with favorable risk disease who were treated with 4 cycles of ABVD plus 30 Gy IFRT versus those who received a less-intensive regimen of 2 cycles of ABVD plus 20 Gy IFRT.6
Conversely, Advani detailed data from trials testing alternative treated strategies in patients with unfavorable disease, which further supported the use of standard-of-care ABVD plus IFRT in these patients. She said strategies that involved more intensive chemotherapy, like escalated BEACOPP (bleomycin, etoposide, adriamycin, cyclophosphamide, vincristine, procarbazine, and prednisone), usually led to increased toxicity without much of an efficacy boost.6,7
Therapy Modifications Based on PET Scans
Whereas most of the data presented supporting the use of standard chemotherapy regimens in early-stage Hodgkin lymphoma were carried out in the era of CT scans, Advani said PET scan results need to be worked into the current prognosis equation. Use of PET scans for prognosis rely on the 5-point Deauville scoring system and collaboration between the oncologist and the nuclear medicine physician.
“The question arises, can modification of therapy be based on interim PET [scans] and have the ability to potentially select patients for treatment escalation of de-escalation,” Advani asked. “Moreover, can these modifications have the potential to improve outcomes?” To answer this, she said the negative-predictive value of this strategy needs to be high, meaning most patients who are selected for continuation or de-escalation of primary therapy should reach disease cure. In addition, patients with PET-positive results should be salvageable by alternative approaches.
PET-Adapted Therapy: 2 cycles ABVD ± 20 Gy
As such, investigators on the phase 3 HD16 trial (NCT00736320) attempted to determine if patients with early stage favorable disease who were PET negative after 2 cycles of ABVD, defined as having a Deauville score of 1 or 2, could avoid IFRT.8 The study results demonstrated that the PFS rates went from 93% to 85% with ABVD plus IFRT versus ABVD alone, respectively, which is not an acceptable result in a curable disease.
“In the scenario where you cut down on the chemotherapy, the radiotherapy is quite critical,” Advani said. “You can’t get away with just 2 cycles of ABVD, even in the most favorable patients.”
The HD16 trial also raised the issue of different outcomes observed based on Deauville scores by interim PET, since patients with a score of 4 had markedly reduced PFS versus patients with scores of 3 or below. “It’s probably not wise to just radiate those patients at that point and you should continue with 2 additional cycles of chemotherapy.”
PET-Adapted Therapy: 3 cycles ABVD ± 20 Gy
In the phase 3 RAPID trial (NCT00943423), investigators determined that in patients with nonbulky stage I or II disease who were PET negative (Deauville 1 or 2) after 3 cycles of ABVD and had no further IFRT experienced inferior 3-year PFS rates to those who went on to received radiotherapy, at 90.8% versus 97.1%, respectively, with a risk ratio of 2.36 (95% CI, 1.13-4.95) favoring the radiotherapy arm in the per protocol analysis. However, there was a nonsignificant difference in PFS rates in the intention-to-treat analysis and no difference in OS outcomes between the 2 groups.9
“One could argue [that] the magnitude of the difference wasn’t much when you look at the intention-to-treat analysis, but there was about a 4% difference per protocol,” Advani said. “For a patient for whom you are worried about late effects, you might accept a slightly lower cure rate.”
PET-Adapted Therapy: 4 cycles ABVD in Deauville 1/2 versus Deauville 3
Advani said prior research indicates that radiotherapy should only be excluded after a negative PET scan if patients are treated with further cycles of chemotherapy.
The phase 2 CALGB-50604 trial (NCT01132807) looked at 2 different treatment approaches for patients with nonbulky stage I or II disease who were treated with 2 cycles of ABVD with interim PET scans. Those with a Deauville score up to 3 were treated with an additional 2 cycles of ABVD whereas those with a positive result received 2 cycles of escalated BEACOPP plus IFRT.10
Results showed superior results for patients who were PET negative. However, further stratification of patients based on Deauville score indicated that those with a score of 3 had worse 3-year PFS rates than those with scores of 1 or 2, at 94% versus 77%, respectively.
“Doing just 2 additional cycles of ABVD if you’re a Deauville 3 doesn’t seem wise because the PFS [rate at 3 years for these patients] is just 77%,” Advani said. “Yes, you can salvage them if they relapse, but it’s [not a reasonable approach] for Deauville 3.”
Moving Forward
According to Advani, clinicians should carefully consider scoring systems used in clinical trials to be able accurately assess which patients are appropriate for the indicated therapy. Furthermore, patients’ Deauville scores for PET-adapted therapy need to be taken into account when determining who is eligible for de-escalated treatment.
“Outcomes for [patients with a] Deauville score of 3 are suboptimal for ABVD for 4 cycles alone,” Advani said, whereas “patients with a negative PET treated with the 2 + 2 regimen [4 cycles of ABVD] have excellent outcomes without radiotherapy.”
With the current treatment strategies employed for these patients, radiotherapy continues to be an appropriate approach for those with a positive interim or end-of-therapy PET scans for preventing relapse.
Advani concluded by reviewing clinical trials investigating the incorporation of novel agents, such as brentuximab vedotin (Adcetris), into frontline treatment strategies for early stage Hodgkin lymphoma.
The phase 2 BREACH trial (NCT02292979) is comparing brentuximab vedotin plus doxorubicine, vinblastine, dacarbazine versus ABVD in patients with stage I/II unfavorable risk disease and PET negative results after 2 chemotherapy cycles. Results indicate that outcomes were similar between the 2 arms, but Advani said long-term efficacy results are still needed as this study is still ongoing.2
“You have to balance risk and benefit for individual patients,” Advani said. “You have the highest cure rate with primary therapy, but you have to optimize survivorship.”
References:
1. Advani RH. Controversies in the management of early-stage Hodgkin lymphoma. Presented at: National Comprehensive Cancer Network Virtual Congress: Hematologic Malignancies; October 9-10, 2020; Virtual.
2. Klimm B, Goergen H, Fuchs M, et al. Impact of risk factors on outcomes in early-stage Hodgkin's lymphoma: an analysis of international staging definitions. Ann Oncol. 2013;24(12):3070-3076. doi: 10.1093/annonc/mdt413
3. Bonadonna G, Bonfante V, Viviani S, Di Russo A, Villani F, Valagussa P. ABVD plus subtotal nodal versus involved-field radiotherapy in early-stage Hodgkin's disease: long-term results. J Clin Oncol. 2004;22(14):2835-2841. doi: 10.1200/JCO.2004.12.170
4. Advani RH, Hong F, Fisher RI, et al. Randomized phase III trial comparing ABVD plus radiotherapy with the Stanford V regimen in patients with stages I or II locally extensive, bulky mediastinal Hodgkin lymphoma: a subset analysis of the North American Intergroup E2496 Trial. J Clin Oncol. 2015;33(17):1936-1942. doi: 10.1200/JCO.2014.57.8138
5. Meyer RM, Gospodarowicz MK, Connors JM, et al; NCIC Clinical Trials Group; Eastern Cooperative Oncology Group. ABVD alone versus radiation-based therapy in limited-stage Hodgkin’s lymphoma. N Engl J Med. 2012;366(5):399-408. doi: 10.1056/NEJMoa1111961
6. Sasse S, Bröckelmann PJ, Goergen H, et al. Long-term follow-up of contemporary treatment in early-stage Hodgkin lymphoma: updated analyses of the German Hodgkin Study Group HD7, HD8, HD10, and HD11 Trials. J Clin Oncol. 2017;35(18):1999-2007. doi: 10.1200/JCO.2016.70.9410
7. von Tresckow B, Plütschow A, Fuchs M, et al. Dose-intensification in early unfavorable Hodgkin's lymphoma: final analysis of the German Hodgkin Study Group HD14 trial. J Clin Oncol. 2012;30(9):907-913. doi: 10.1200/JCO.2011.38.5807
8. Fuchs M, Goergen H, Kobe C, et al. Positron Emission Tomography-Guided Treatment in Early-Stage Favorable Hodgkin Lymphoma: Final Results of the International, Randomized Phase III HD16 Trial by the German Hodgkin Study Group. J Clin Oncol. 2019;37(31):2835-2845. doi: 10.1200/JCO.19.00964
9. Radford J, Illidge T, Counsell N, et al. Results of a trial of PET-directed therapy for early-stage Hodgkin’s lymphoma. N Engl J Med. 2015;372(17):1598-1607. doi: 10.1056/NEJMoa1408648
10. Straus DJ, Jung SH, Pitcher B, et al. CALGB 50604: risk-adapted treatment of nonbulky early-stage Hodgkin lymphoma based on interim PET. Blood. 2018;132(10):1013-1021. doi: 10.1182/blood-2018-01-827246
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen