Major Programs Under Way in Immuno-Oncology
Following recent approvals by the US Food and Drug Administration (FDA) of pembrolizumab and nivolumab, numerous programs to develop and expand use of immunotherapies have ensued.
Following recent approvals by the US Food and Drug Administration (FDA) of pembrolizumab and nivolumab, numerous programs to develop and expand use of immunotherapies have ensued.
Checkpoint Inhibitors
Following recent approvals by the US Food and Drug Administration (FDA) of pembrolizumab and nivolumab,1,2numerous programs to develop and expand use of immunotherapies have ensued. Below is an overview of some of these programs.Merck/Eisaiannounced a clinical trial collaboration on March 4, 2015, to evaluate Merck’s programmed death 1 (PD-1) inhibitor pembrolizumab in combination with several of Eisai’s lead compounds for oncology, including the microtubule inhibitor eribulin for triple-negative breast cancer and the multi-receptor tyrosine kinase (RTK) inhibitor lenvatinib for select solid tumors.3
AstraZeneca| A programmed death ligand 1 (PD-L1) inhibitor, MEDI4736, is in phase III trials for non-small cell lung cancer (NSCLC).
Genentech |Another PD-L1 inhibitor, MPDL3280A, achieved consecutive breakthrough status designations from the FDA for treatment of bladder cancer in mid-2014, then for treatment of NSCLC on February 2, 2015.4
Bispecific T-Cell Engagers (BiTE)
Adoptive T-Cell Therapy
Merck/Amgen |After successful combination trials of talimogene laherparepvec (TVEC), its oncolytic viral immunotherapy treatment for melanoma, with the cytotoxic T-lymphocyte antigen 4 (CTLA-4) inhibitor ipilimumab, Amgen is now engaged in trials combining TVEC with the PD-1 inhibitor pembrolizumab.5Amgen. Blinatumomab, an immunotherapy monoclonal targeting the CD19 antigen for treatment of acute lymphoblastic leukemia (ALL), received accelerated FDA approval in December 2014.6Juno Therapeutics|The Seattle startup, after initiating several clinical trials within just a year of launching the company, raised $265 million in its December 2014 IPO, less than a month after the FDA granted breakthrough status to JCAR015, one of Juno’s chimeric antigen receptor (CAR) therapies. In Security and Exchange Commission filings, Juno indicated that FDA approval could come as soon as 2017. Juno has 5 ongoing phase I trials testing CAR agents as treatment for ALL, non-Hodgkin lymphoma (NHL), and chronic lymphocytic leukemia (CLL). Almost all of the therapies involve CARs targeting CD19, a hematologic cancer antigen, although one trial involves modified T-cell receptors (TCRs) to treat acute myelogenous leukemia (AML), chronic myelogenous leukemia (CML), and NSCLC. The IPO also came shortly after Juno made a deal with National Cancer Institute (NCI) partnered with Opus Bio to license a CAR targeting CD22,7a protein common in lymphomas. This transaction immediately added a CAR clinical candidate to Juno’s portfolio, since NCI has already begun enrollment in a phase I study of ALL and NHL using the CD22 CAR.
Kite Pharma| Another notable mover in the CAR arena is Kite Pharma in Santa Monica, California. Kite’s current pipeline has CARs recognizing CD19, with one candidate already in phase II/III study for B-cell malignancies and another in phase I for NHL. A Kite CAR against epidermal growth factor receptor variant III (EGFRvIII) is in phase I trials for treatment of glioblastoma. Last June, Kite obtained an exclusive, worldwide license from NCI as part of a Cooperative Research and Development Agreement (CRADA) for TCRs developed against NY-ESO-1, an antigen expressed in numerous tumor types. NCI is in phase II clinical trials with such a TCR, and Kite has 3 more TCRs via the CRADA in phase I trials on various tumors. Kite signed a deal with Amgen on January 5, 2015, to develop CAR therapies for Amgen cancer targets on Kite’s platform, with Kite receiving $60 million up front and a potential $525 million in milestones, plus funding for R&D costs.8
bluebird bioof Cambridge, Massachusetts, is also a player in the CAR space, although much of its pipeline involves gene therapy. Bluebird is entering the third year of a collaboration with Celgene to develop CARs, but all products are still preclinical.
Immunocore| An Oxford, United Kingdom company, Immunocore has major development collaborations with Genentech, GlaxoSmithKline (GSK), and AstraZeneca to develop CARs on the Immunocore development platform. Immunocore’s own lead product, a CAR called IMCgp100, is in a phase I/II dosing study for late-stage melanoma.9Adaptimmune, a sister company to Immunocore with access to the same development platform but for TCRs only, has 6 indications in phase I/II trials for its TCR against NY-ESO as part of a GSK collaboration.
Indoleamine-2,3-dioxygenase (IDO) Inhibitors
Novartis| Novartis has been developing CAR therapies with the University of Pennsylvania as part of a global research and licensing agreement struck in 2012. Ongoing clinical trials evaluating a CAR therapy known as CTL019 have yielded promising results in patients with ALL, leading to the FDA granting breakthrough status for CTL019 in July 2014. On February 18, 2015, Novartis announced the beginning of a phase I trial of a University of Pennsylvania CAR against EGFRvIII for treatment of glioblastoma on the basis of encouraging preclinical results.10Bristol-Myers Squibb/Flexus. On February 23, 2015, BMS announced a $1.25 billion deal to acquire the IDO inhibitor assets of Bay Area startup Flexus, a program that is still Pre-Investigational New Drug (IND).11Flexus management intends to start a new company with its remaining assets; these include current personnel and facilities and FLX925, an inhibitor of Fms-like tyrosine kinase 3 (FLT3) and CDK4/6 just beginning phase I trials, and a non-IDO immunotherapy focusing on regulatory T cells.
Future Directions for Immuno-Oncology
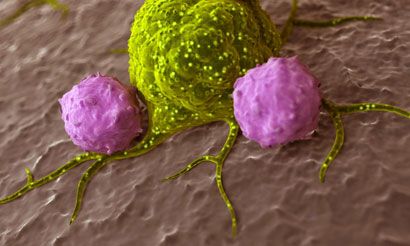
Amgen/NewLink Genetics. The BMS/Flexus agreement came just 4 months after Amgen announced a potentially billion-dollar plus deal with NewLink Genetics to license IDO pathway inhibitor NLG919 and launch a research collaboration to discover additional compounds for IDO-tryptophan-2,3-dioxygenase (TDO) therapy. The total deal could mean more than $1 billion to NewLink.12Surface Oncology| A startup seeded in 2014 with another $35 million in backing as of January 8, 2015, this Cambridge, Massachusetts, company may define a new category, next generation immuno-oncology. Like Flexus, Surface Oncology is also looking at manipulating regulatory T cells, but wants to exploit other immune system targets to aid recognition and destruction of tumors. Next generation immuno-oncology could modify not only T cells but also antigen-presenting cells (APCs), tumor associated macrophages, and others, helping the immune system to destroy tumors by improving antigen presentation for efficient activation or by blocking the activity of various suppressor cells in the tumor microenvironment.
immatics| A German company, immatics, is also involved in the antigen-presentation process for the activation of T cells. Combining a proteomics approach using mass spectrometry to directly identify antigens overexpressed on tumor cells, immatics prepares cancer vaccines derived from these tumor-associated antigens. Depending on the length of the peptides derived from tumor antigens, vaccines can be designed to activate either cytotoxic T cells or T-helper cells. The company’s lead product for treatment of renal cancer is in phase III trials, with another for colorectal cancer having recently completed phase II trials; a third therapy for glioblastoma is beginning phase I trials. On the basis of a partnership with Roche established a year ago to develop immunotherapies using the immatics platform, the company also has active early-stage programs in gastric cancer, NSCLC, and prostate cancer. On March 2, 2015, the Cancer Prevention and Research Institute of Texas (CPRIT) awarded immatics a $20 million grant for the development of adoptive T-cell therapies in collaboration with the MD Anderson Cancer Center, Houston, Texas, at a new US-based subsidiary of immatics.
Roswell Park Cancer Institute| This Buffalo, New York, facility received a $12 million grant on January 14, 2015, from the New York State Stem Cell Science Program to fund development of a stem-cell based treatment for ovarian cancer.13Like Kite and Adaptimmune, RPCI is focusing on the tumor antigen NY-ESO-1, and intends to express a cloned TCR with specificity for NY-ESO-1 into hematopoietic stem cells removed from patients. A portion of the stem cells infused back into the patients will develop into mature T cells with specificity for NY ESO 1.
References
- Merck Receives FDA Breakthrough Therapy Designation for KEYTRUDA® (pembrolizumab) in Advanced Non-Small Cell Lung Cancer. http://www.businesswire.com/news/home/20141027005286/en/Merck-Receives-FDA-Breakthrough-Therapy-Designation-KEYTRUDA%C2%AE#.VQB_CpU5DIU. October 27, 2014. Accessed March 15, 2015.
- FDA Expands Approved Use of Opdivo (nivolumab) to Treat Lung Cancer. http://www.drugs.com/newdrugs/fda-expands-approved-opdivo-nivolumab-lung-cancer-4179.html. March 4, 2015. Accessed March 15, 2015.
- Eisai and Merck Enter Collaboration to Explore Novel Combination Regimens of Anti-PD-1 Therapy With Multi-targeting RTK Inhibitor and Microtubule Dynamics Inhibitor in Multiple Types of Cancer. http://www.mercknewsroom.com/news-release/prescription-medicine-news/eisai-and-merck-enter-collaboration-explore-novel-combinatio. March 4, 2015. Accessed March13, 2015.
- FDA Grants Breakthrough Therapy Designation for Genentech’s Investigational Cancer Immunotherapy MPDL3280A (anti-PDL1) in Non-Small Cell Lung Cancer. http://www.gene.com/media/press-releases/14583/2015-02-01/fda-grants-breakthrough-therapy-designat. February 1, 2015. Accessed March 11, 2015.
- New Trial Initiated Evaluating Amgen’s Talimogene Laherparepvec in Combination With Merck’s Anti-PD-1 Therapy KEYTRUDA® (Pembrolizumab) for Advanced Melanoma. https://www.amgen.com/media/media_pr_detail.jsp?year=2014&releaseID=1995881 . December 8, 2014. Accessed March 15, 2015.
- FDA Approves BLINCYTO™ (Blinatumomab) Immunotherapy for the Treatment of Relapsed or Refractory B-Cell Precursor Acute Lymphoblastic Leukemia. http://www.amgen.com/media/media_pr_detail.jsp?releaseID=1994704. December 3, 2014. Accessed March 10, 2015.
- Juno Therapeutics Executes License for Phase I Car T Product Candidate Targeting CD22 for Hematological Malignancies. https://junotherapeutics.com/juno-therapeutics-executes-license-for-phase-i-car-t-product-candidate-targeting-cd22-for-hematological-malignancies/. Accessed March 12, 2015.
- Amgen and Kite Pharma Announce Strategic Cancer Immunotherapy Collaboration to Advance the Application of Novel Chimeric Antigen Receptor (CAR) T Cell Therapies. http://www.amgen.com/media/media_pr_detail.jsp?releaseID=2002967. January 5, 2015. Accessed March 9, 2015.
- IMCgp100 in Clinical Development. http://www.immunocore.com/pipeline/imcgp100/. Accessed March 13, 2015.
- Penn Medicine Study Describes Development of Personalized Cellular Therapy for Brain Cancer. http://www.uphs.upenn.edu/news/News_Releases/2015/02/maus/. February 18, 2015. Accessed March 10, 2015.
- Bristol-Myers Squibb Co Expands Cancer Treatment Pipeline With $1.25 Billion Purchase of Flexus Biosciences. http://www.ibtimes.com/bristol-myers-squibb-co-bmy-expands-cancer-treatment-pipeline-125-billion-purchase-1825010. February 23, 2015. Accessed March 13, 2015.
- Genentech, NewLink Launch $1.15B Cancer Collaboration. http://www.genengnews.com/gen-news-highlights/genentech-newlink-launch-1-15b-cancer-collaboration/81250487/. October 20, 2014. Accessed March 15, 2015.
- New York State Awards Grant for First Stem-Cell Immunotherapy Trial in Ovarian Cancer. http://www.targetedonc.com/articles/New-York-State-Awards-Grant-for-First-Stem-Cell-Immunotherapy-Trial-in-Ovarian-Cancer. January 15, 2015. Accessed March 14, 2015.
<<<
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More