Liso-Cel Proves Cost-Effective for R/R DLBCL
A study evaluating healthcare expenses identified lisocabtagene maraleucel as a cost-effective second-line treatment for patients with diffuse large B-cell lymphoma.
Lymphomas: © immimagery - stock.adobe.com
Lisocabtagene maraleucel (liso-cel; Breyanzi), a chimeric antigen receptor (CAR) T-cell therapy, was identified as a cost-effective treatment option for patients with refractory or early relapse diffuse large B-cell lymphoma (DLBCL) following first-line chemoimmunotherapy.1,2
Patients treated with liso-cel demonstrated an average life expectancy of 5.34 years and gained 3.64 quality-adjusted life years (QALYs) compared with the standard of care, which resulted in an average 2.47-year average life expectancy and 1.62 QALYs. The incremental cost-effectiveness ratio (ICER) of liso-cel was $99,669 per QALY from a healthcare sector perspective and $68,212 from a societal perspective.
With the study’s $100,000 per QALY threshold and an acceptable upper-end of $150,000 per QALY in the United States, liso-cel demonstrated its cost-effectiveness. In some scenarios, investigators noted that, in some scenarios, the cost of liso-cel surpassed $100,000 but remained under $150,000.
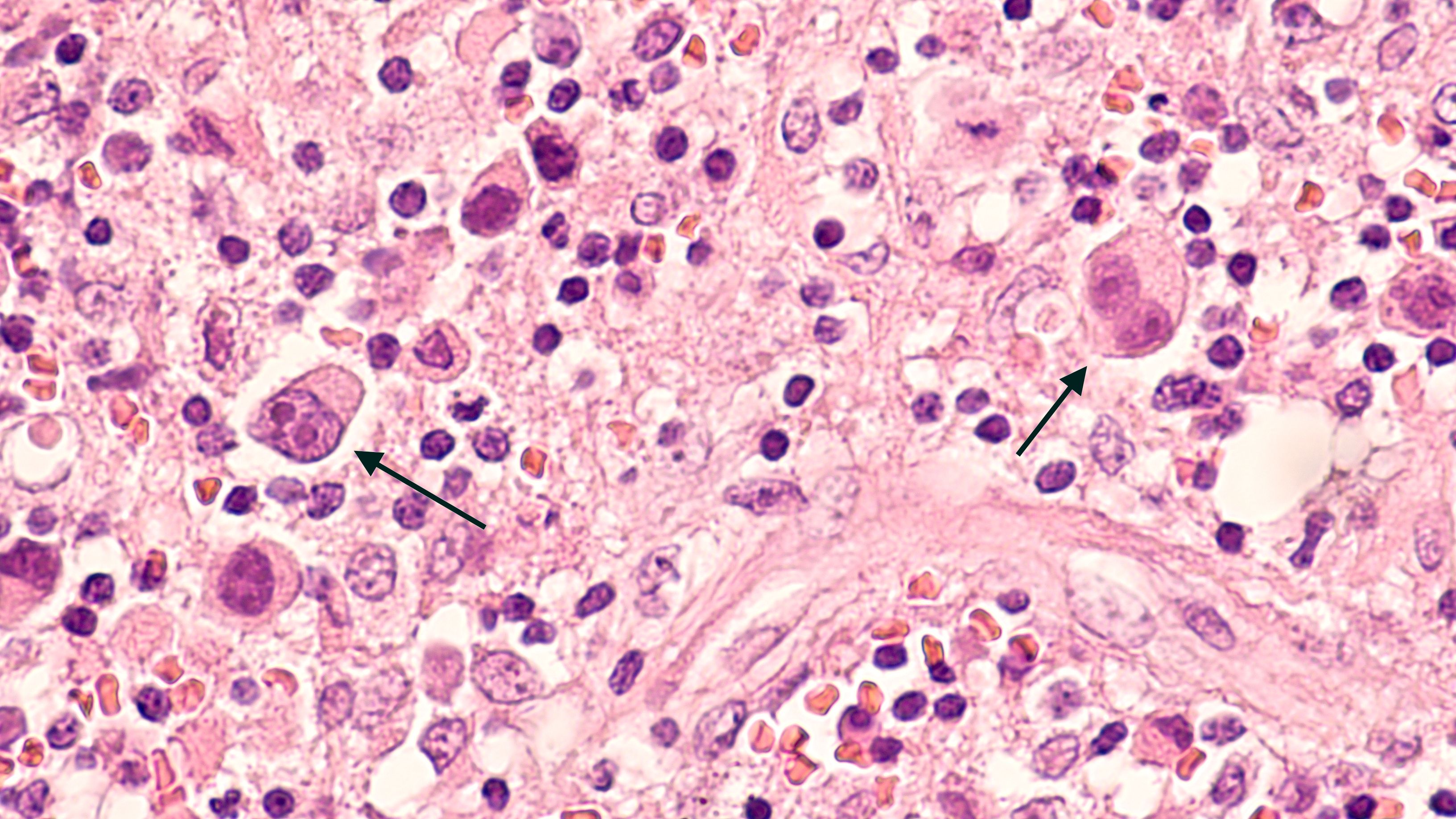
Lymphoma | Image Credit: © David A Litman - www.stock.adobe.com.jpg
Findings from the study were published in Blood Advances. The study calculated the ICER of liso-cel vs platinum-based chemotherapy followed by autologous hematopoietic stem cell transplantation using data from the TRANSFORM (NCT03575351) and TRANSCEND (NCT02631044) studies. Investigators identified a representative cohort of adult patients aged 60 years old and employed a partitioned survival model.
"In our study, we incorporated the often-overlooked societal costs associated with cancer treatment, which are typically neglected in cost-effectiveness analyses that focus solely on the healthcare sector related-expenses," explained Mohamed Abou-el-Enein, MD, PhD, MSPH, an associate professor of medicine at the Keck School of Medicine at the University of Southern California and the senior author of the study, said in a press release.1 “Cancer treatments can diminish quality of life, causing work absences and challenges in managing everyday activities, especially among the elderly. Treatments that improve quality of life not only benefit the patient but also reduce these broader societal costs, which is an important aspect of our cost-effectiveness evaluation,”
While treatments like liso-cel have promising survival outcomes in DLBCL, their costs are significant. In 2023, the acquisition cost of liso-cel was $447,227, rising from $410,300 the year before. The rising cost of liso-cel price could also mean that the drug will not continue to be as cost-effective in the future, according to study authors.
The total cost of treatment is also increased when considering hospitalization costs, post-treatment care, and adverse effect management. These costs can create serious barriers to access for patients, especially those with lower income or limited insurance coverage. However, even with these considerations, CAR T-cell therapies present an economic advantage over other treatment methods.
“[The findings] reaffirm the importance of evaluating CAR T-cell therapies beyond their immediate costs, emphasizing their long-term clinical and societal impacts for a more comprehensive assessment of their overall value,” study authors concluded.2
REFERENCES:
1. Liso-cel is a cost effective second-line treatment for common form of lymphoma. News release. American Society of Hematology. December 28, 2023. Accessed January 2, 2024. http://tinyurl.com/554hzptw
2. Choe J, Yu T, Abramson J, et al. Cost-Effectiveness of second-line lisocabtagene maraleucel in relapsed or refractory diffuse large B-cell lymphoma. Blood Adv. Published online December 28, 2023. doi:10.1182/bloodadvances.2023011793
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen