Ide-Cel Shows Clinically Meaningful PFS Improvement in Triple-Class-Exposed RRMM
The phase 3 Karmma-3 trial of ide-cel in patients with triple-class-exposed relapsed/refractory multiple myeloma generated significantly improved progression-free survival and overall response rates vs standard regimens.
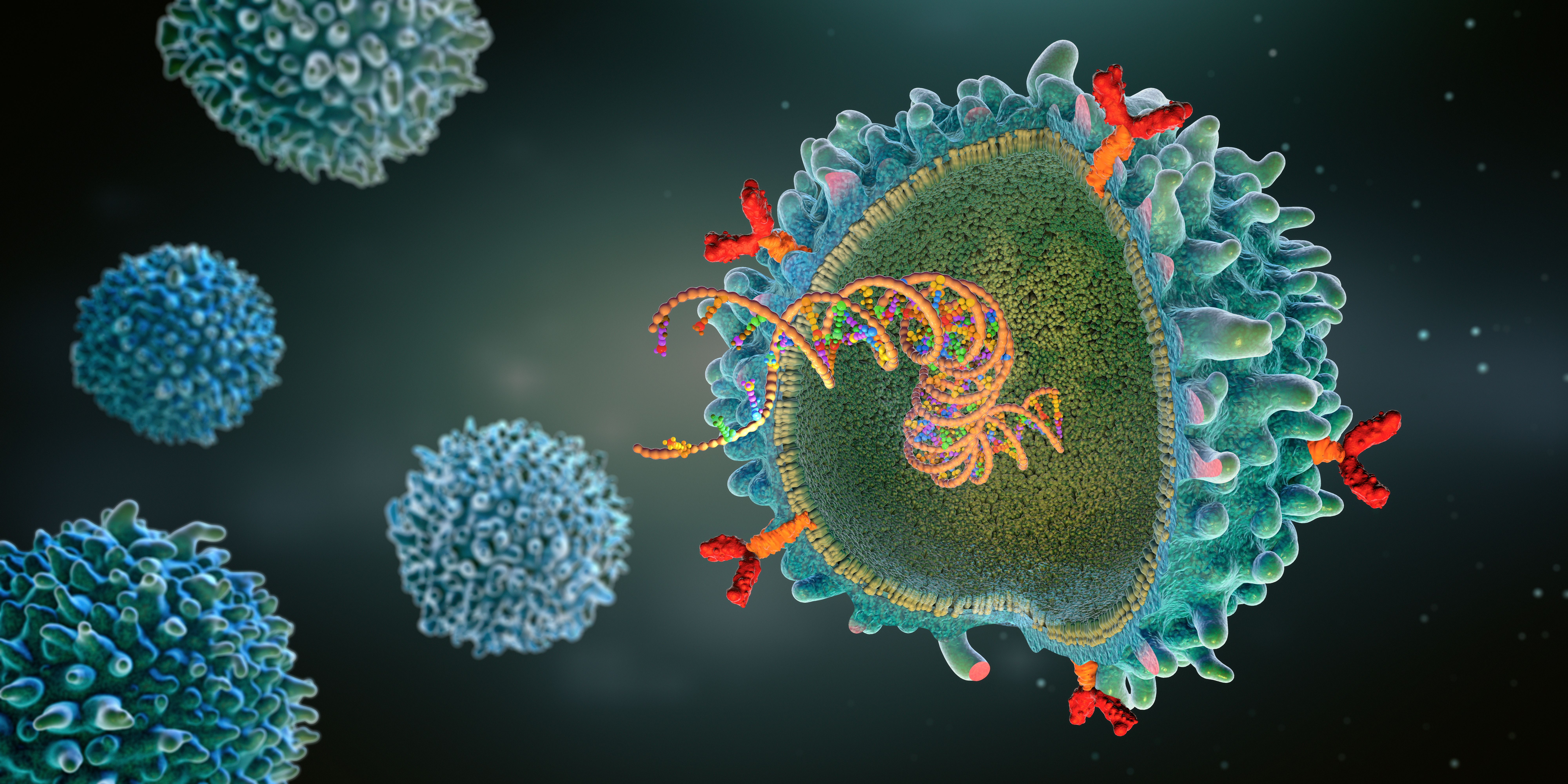
Image Credit: © Christoph Burgstedt [stock.adobe.com]
Treatment with idecabtagene vicleucel (ide-cel; Abecma) led to a significantly prolonged progression-free survival (PFS) and improved response compared with standard regimens in patients with triple-class-exposed relapsed and refractory multiple myeloma (RRMM), according to findings from the phase 3 KarMMa-3 trial (NCT03651128).1
At a median follow-up of 18.6 months, patients given ide-cel had a median PFS of 13.3 months compared with 4.4 months in the standard-regimen group (HR, 0.49; 95% CI, 0.38-0.65; P < .001) and significantly reduced the risk for disease progression by 51%.
The toxicity of ide-cel was also consistent with what has been previously reported.
Ide-cel is a B-cell maturation antigen–directed chimeric antigen receptor (CAR) T-cell therapy. In previous studies, the therapy elicited deep and durable responses in patients with heavily pretreated RRMM. Still, survival rates are poor among this patient population.
To further examine safety and efficacy of the agent compared with standard regimens for patients with RRMM, a total of 386 were enrolled and randomized in the international, open-label, phase 3 KarMMa-3 trial. Those enrolled included patients who had previously received 2-4 regimens, including immunomodulatory agents, proteasome inhibitors, and daratumumab (Darzalex), and those who had disease refractory to the last regimen.
Patients were randomly assigned in a 2:1 ratio to receive either ide-cel at a dose ranging from 150 × 106 to 450 × 106 CAR-positive T cells, or 1 of 5 standard regimens.
Patients aged 18 years and older with RRMM who have received at least 2 but no more than 4 prior MM regimens, prior treatment with daratumumab, a proteasome inhibitor- and an immunomodulatory compound-containing regimen for at least 2 consecutive cycles, and who achieved a response to at least 1 prior treatment regimen were included in the study. Additionally, patients with an ECOG performance status of 0-1 with adequate vascular access for leukapheresis and recovery to grade 1 or baseline of any non-hematologic toxicities due to prior treatments were included.
Investigators evaluated the primary end point of PFS and secondary end points of overall response, overall survival, event-free survival, minimal residual disease (MRD), complete response, duration of response (DOR), time to response, adverse events (AEs), quality-of-life, time to next anti myeloma treatment, PFS after next line therapy, and pharmacokinetics.2
A total of 386 patients were enrolled and randomized between May 2019 and April 2022 at 49 sites in 12 countries, including 254 patients to receive ide-cel and 132 to a standard regimen. In total, 66% of the patients had triple-class-refractory disease, and 95% had daratumumab-refractory disease.1 In the standard-regimen group, 43 patients were randomized to receive daratumumab, pomalidomide (Pomalyst), and dexamethasone, 30 received carfilzomib (Kyprolis) and dexamethasone, 30 to elotuzumab (Empliciti), pomalidomide, and dexamethasone, 22 were randomized to ixazomib, lenalidomide (Revlimid), and dexamethasone, and 7 to daratumumab, bortezomib (Velcade), and dexamethasone.
At baseline, characteristics of the patients were generally balanced in the 2 groups, except for Black race (7% of the patients in the ide-cel group vs 14% of patients in the standard-regimen group). In the ide-cel group, 107 patients (42%) had high-risk cytogenetic abnormalities vs 61 (46%) in the standard-regimen group, the median time since diagnosis was approximately 4 years in both groups, and the median time to progression during the last previous anti myeloma therapy was approximately 7 months. Further, patients received a median number of 3 previous regimens (range, 2-4) in each group.
In the intention-to-treat population, which included the 29 patients in the ide-cel group and 6 patients in the standard-regimen group who did not receive the assigned therapy, PFS was significantly longer among those given ide-cel compared with patients given the standard-regimen group. At 6 months the PFS was 73% in the ide-cel group vs 40% in the standard-regimen group, and at 12 months, PFS rates were 55% and 30%, respectively. The progression-free survival benefit with ide-cel therapy was consistently observed across prespecified subgroups.
A total of 71% of patients in the ide-cel group and 42% of patients in the standard-regimen group had a response with treatment (P < .001), and 39% and 5%, respectively, achieved a complete response. At this time, data on overall survival were immature.
Among patients in the ide-cel arm, the median time to response was 2.9 months (range, 0.5-13.0) vs 2.1 months (range, 0.9-9.4) for those in the standard-regimen group. The median DOR was 14.8 months (95% CI, 12.0-18.6) with ide-cel and 9.7 months (95% CI, 5.4-16.3) with the standard-regimen. MRD-negative status within 3 months before the occurrence of at least a complete response was confirmed in 51 patients (20%) who received ide-cel and 1 patient (1%) given the standard-regimen.
Looking at safety, AEs that were grade 3 or 4 were seen in 93% of the patients who received ide-cel and in 75% of patients in the standard-regimen group. The most common hematologic AEs consisted of neutropenia (78% of the patients in the ide-cel group vs 44% in the standard-regimen group), anemia (66% vs 36%), and thrombocytopenia (54% vs 29%), respectively. Of patients in the ide-cel group who had grade 3 or 4 thrombocytopenia or neutropenia that persisted beyond 1 month, the median time to recovery was 1.9 months (95% CI, 1.5-2.1) after thrombocytopenia and 1.7 months (95% CI, 1.5-1.9) after neutropenia.
Serious AEs were seen in 130 patients (52%) in the ide-cel group vs 48 patients (38%) in the standard-regimen group. Grade 5 treatment-related AEs were observed in 6 of 225 patients (3%) treated with ide-cel group and 1 patient (1%) in the standard-regimen group. The most frequent treatment-related AE was sepsis, seen in 5 patients (2%) in the ide-cel group and 1 patient (1%) in the standard-regimen arm, respectively. The incidence of second primary cancer was similar in the ide-cel group and the standard-regimen group (6% and 4%, respectively). Of the 225 patients given ide-cel, 88% had cytokine release syndrome, and 5% of these patients had an event of grade 3 or higher. Additionally, investigator-identified neurotoxic effects were reported in 15% of these patients, with 3% having an event of grade 3 or greater.