From ABVD to Nivolumab-AVD: New Treatment Strategies in Hodgkin Lymphoma
The field of Hodgkin lymphoma is undergoing significant advancements, with new drugs entering the frontline and personalized treatment approaches emerging.
Stephen M. Ansell, MD, PhD

As discussed at 2024 Society of Hematologic Oncology (SOHO) Annual Meeting, the focus of treating patients with Hodgkin lymphoma has shifted towards optimizing treatment strategies, considering individual risk profiles.
Historically, ABVD (doxorubicin hydrochloride [Adriamycin], bleomycin, vinblastine sulfate, and dacarbazine) chemotherapy and escalated BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine [Oncovin], procarbazine, and prednisone) were the primary regimens. However, recent studies have shown that nivolumab (Opdivo)-AVD (doxorubicin, vinblastine, and dacarbazine) chemotherapy and BrECADD (brentuximab vedotin [Adcetris], etoposide, cyclophosphamide, doxorubicin, dacarbazine, and dexamethasone) are more effective and have better tolerability profiles.
In an interview with Targeted OncologyTM, Stephen M. Ansell, MD, PhD, chair of the Division of Hematology at Mayo Clinic in Rochester, Minnesota, discussed how to manage patients with advanced-stage Hodgkin lymphoma.
Targeted Oncology: Can you discuss the session you were a part of at SOHO 2024?
Ansell: It is an interesting time in Hodgkin lymphoma, and that is because in advanced stage Hodgkin lymphoma. New drugs have now moved into frontline therapies, and comparative randomized trials are being done that are kind of moving the field forward. The key question now becomes how best to manage patients, looking at low-risk patients right through to high-risk patients, and [determining] which of the patients need which regimen? The session [talked] about, what is the current frontline therapy? How do we sequence treatment in the second line and in subsequent lines? But specifically, what [do we do] for the patients that are low-risk, medium-risk, and high-risk?
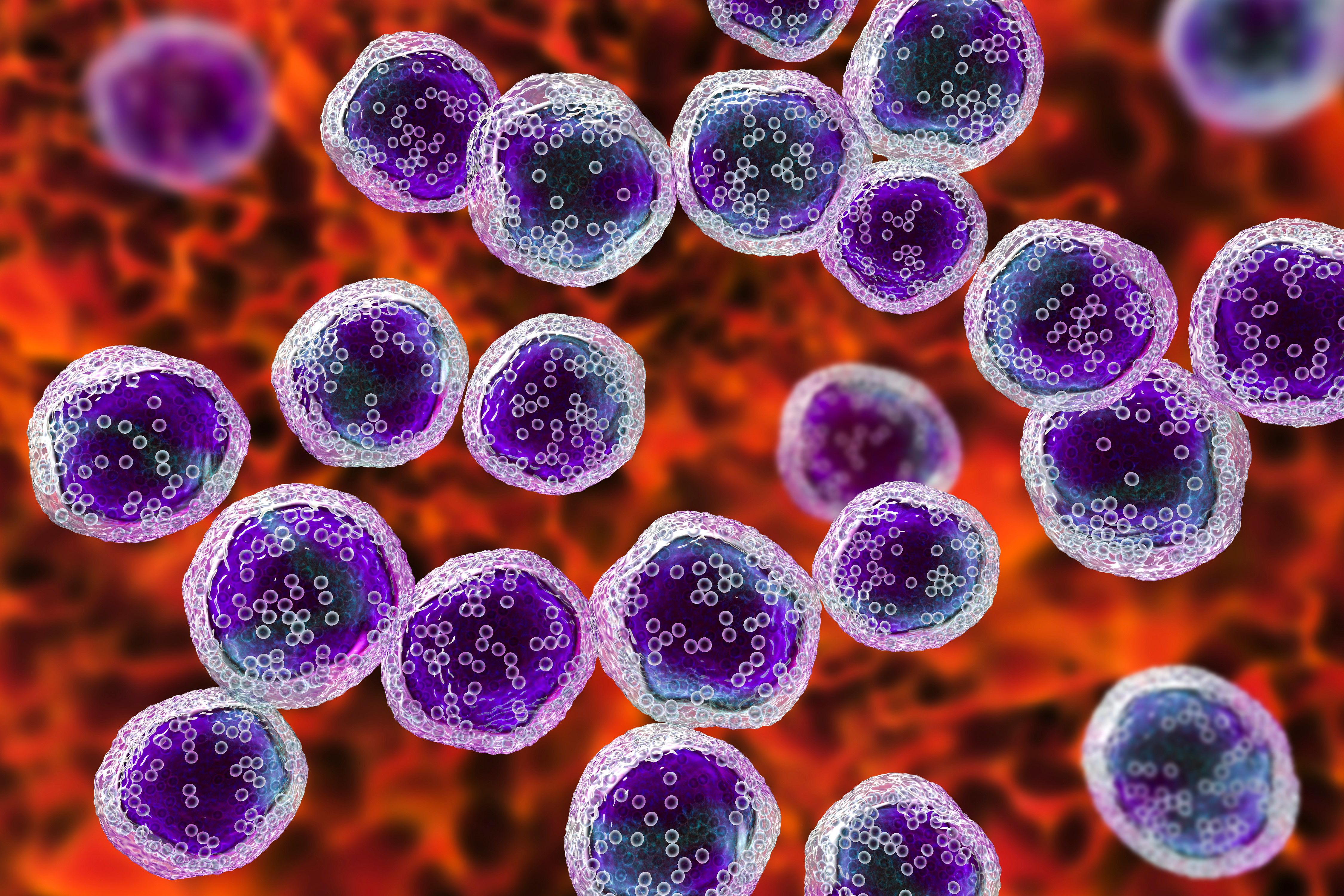
Lymphoma cells: © Dr_Microbe - stock.adobe.com
What is the current role of the 2 primary regimens?
Historically, ABVD chemotherapy was a standard, but it was low intensity with a plan to escalate if needed. In contrast, escalated BEACOPP was a much more intense regimen with a goal to de-escalate by fewer cycles of treatment. One had a little less efficacy, but less toxicity. The other had more efficacy, but more toxicity. Over time, ABVD chemotherapy has now already been replaced by nivolumab-AVD chemotherapy, and escalated BEACOPP is being replaced by BrECADD. The discussion is about what to do with the old ABVD—and I think, in many cases, we are kicking that to the curb—and what to do about escalated BEACOPP. In many cases, BrECADD has replaced that.
What are some of the main challenges or limitations associated with these regimens?
Each of those regimens brings additional and different toxicities. Starting with ABVD chemotherapy, which used to be the standard, it is pretty well tolerated. But the B part, the bleomycin, had significant lung toxicity. One has to really be careful about that. Escalated BEACOPP was a high-intensity regimen with a lot of hematological toxicity, a lot of long-term fatigue problems, and an increase in second malignancies.
Now, the 2 new regimens in the middle, the nivolumab-AVD chemotherapy, that does bring some immune toxicities, because nivolumab is a PD-1–blocking antibody, and the BrECADD, with the brentuximab vedotin added, does bring some additional neuropathy problems. But the intensity of treatment has been diminished, so therefore the hematological toxicity is better.
What are some of the promising new therapies and treatment approaches that are emerging?
The 2 that are front and center have not been compared to each other, and that is clearly what is needed in the future. This is the addition of nivolumab, a PD-1 antibody, to AVD chemotherapy, the nivolumab and AVD combination, and then the addition of brentuximab vedotin to a modified, escalated BEACOPP, the BrECADD regimen. Both of these are highly effective. What is not clear is which regimen should be used for which patient. I think in the future, those 2 regimens are going to need to be compared in a randomized trial. The 2 trials that just established these 2 as the winners are just reading out right now, so while there are discussions, those trials have not really been formulated just yet.
How is immunotherapy being integrated into treatment for advanced-stage Hodgkin lymphoma?
One of the regimens, nivolumab and AVD chemotherapy, has an immune checkpoint blocking antibody. The nivolumab is right in the combination. But I think more broadly, PD-1 blockade and agents such as pembrolizumab [Keytruda] and nivolumab have been broadly used in patients with Hodgkin lymphoma. Many [have been] in the posttransplant relapse setting and then subsequently, in the salvage treatment combinations before going to a transplant. As I mentioned, in the frontline therapy, the advantages are you can see benefits [to] patients in each of these scenarios. In fact, interesting data suggests that using a PD-1–blocking antibody before intensive treatment like a stem cell transplant results in significantly greater benefit, suggesting that we are doing something immunological when we do that kind of treatment.
How do you think the treatment for these patients is becoming more personalized?
I think in many respects, the personalization is focused on the patient's frailty vs robustness to tolerate treatment. One of the things that has been interesting is that nivolumab-AVD chemotherapy is very well tolerated in elderly patients. One of the problems with Hodgkin lymphoma is that [older] patients have been difficult to treat, purely because of the challenges they have tolerating these treatments. But the use of nivolumab and AVD has shown that regimen can be well tolerated. Similarly, using brentuximab with AVD, by doing the brentuximab alone first and then the rest of the regimen, has also shown that you can give that to [older] patients. The personalization is not personalized to the point of understanding the tumor biology. It is more personalized to the understanding of the patient and their needs.
For a community oncologist, what are the key takeaways from your session?
The key takeaways are that this is a field that is moving fast. I think within the US, there is a greater kind of embracing of the nivolumab and AVD chemotherapy regimen. I certainly would say that it has advantages, because one can use it in almost any population with good results. Comparisons of in the [younger] patients and comparisons in the [older] patients, compared with brentuximab and AVD shows benefit for the nivolumab and AVD. I think a takeaway for a community oncologist is that this is probably going to become the standard of care.
Speaking of community oncologists, there [were] a number of discussions [at SOHO 2024] about how to integrate immunotherapies, not so much now in Hodgkin lymphoma, but in other lymphomas like low-grade lymphomas and large cell lymphoma, particularly bringing bispecific antibodies to the community. Those are agents that are highly effective, but with some toxicity in the first month. How to use that in a community setting in a safe and effective way is one of the things being discussed. I certainly think it is one of those things that we will get it worked out, and it will be usable and useful across the board.
REFERENCE:
Ansell SM. Advanced Stage Hodgkin Lymphoma, the End of ABVD and BEACOPP? Presented at: 2024 SOHO Annual Meeting; September 4-7, 2024; Houston, Texas.
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen










