Extended Survival Observed in Patients With Solitary Brain Metastasis From RCC
Although patients who develop brain metastases from renal cell carcinoma typically have poor outcomes, investigators from Yale University have identified a subset of patients who demonstrated extended survival.<sup>1</sup>Those patients with a single metastasis were less likely to develop central nervous system\ recurrence after local therapy. This is an encouraging development because these patients have historically been excluded from participating in clinical trials and receiving aggressive treatment regimens.
Alfredo Suarez-Sarmiento, Jr, MD

Alfredo Suarez-Sarmiento, Jr, MD
Although patients who develop brain metastases (BMs) from renal cell carcinoma (RCC) typically have poor outcomes, investigators from Yale University have identified a subset of patients who demonstrated extended survival.1Those patients with a single metastasis were less likely to develop central nervous system (CNS) recurrence after local therapy. This is an encouraging development because these patients have historically been excluded from participating in clinical trials and receiving aggressive treatment regimens.
“There are no guidelines for screening and surveillance for brain involvement, so we sought to document our single institution experience,” said lead author Alfredo Suarez-Sarmiento, Jr, MD, an associate research scientist at Yale University School of Medicine during the 2018 American Urological Association Annual Meeting.
Suarez-Sarmiento and colleagues reported that the median overall survival after diagnosis of RCC BM was 8.5 months with a 3-year survival of 28.2%. Median survival after diagnosis of RCC BM was similar between individuals who presented, recurred, or progressed. The median CNS recurrence-free survival (RFS) was 8.5 months for the whole cohort; however, those with 1 and >1 lesion had a median RFS of 12.4 and 6 months, respectively (P<.001). Overall survival and CNS RFS were calculated using Kaplan-Meier and Cox-hazard proportion ratio tests.
Brain metastasis is a relevant complication in the course of renal cancer progression because it is a major cause of morbidity and mortality in patients with RCC. Treatment of metastatic RCC is challenging because most RCCs are resistant to radio- and chemotherapy.2The median survival time after the diagnosis of BMs in patients with metastatic RCC is only approximately 10 months.3
The investigators reviewed clinical notes, patient demographics, comorbidities, tumor histology, CNS treatments, systemic therapy, and outcomes for 160 patients in the Yale New Haven Hospital database who were undergoing evaluation for RCC BM from 1987 to 2017.
Among the total number of patients, 95% had clear cell histology and 90% had extracranial metastases at diagnosis. A total of 36 patients (62.5%) had RCC BMs at the time of diagnosis, 85 (62.5%) had metastatic disease that progressed to the brain, and 15 (11%) had CNS involvement at the time of recurrence after nephrectomy.
Clinical symptoms were noted in 80% of patients. “The number of lesions and not size of the largest lesion was found to correlate with symptoms,” said Suarez-Sarmiento. The median size of lesions was 9 mm and the median number of lesions was 2 per patient with 90 patients having more than 1 lesion and 60 patients having only 1 lesion.
Patients with a solitary lesion were more likely to receive a craniotomy (15% vs 5%), while patients with >1 lesion were more likely to receive radiosurgery (32.4% vs 19.7%). After receiving treatment for RCC BMs, 55% of individuals received systemic therapy. Patients with more than 1 lesion were more likely to receive systemic therapy (83.3% vs 54.3%;P<.0001), than those who had only 1 lesion (TABLE).
TABLE. Treatment Options for Patients with Brain Metastases From Renal Cell Carcinoma
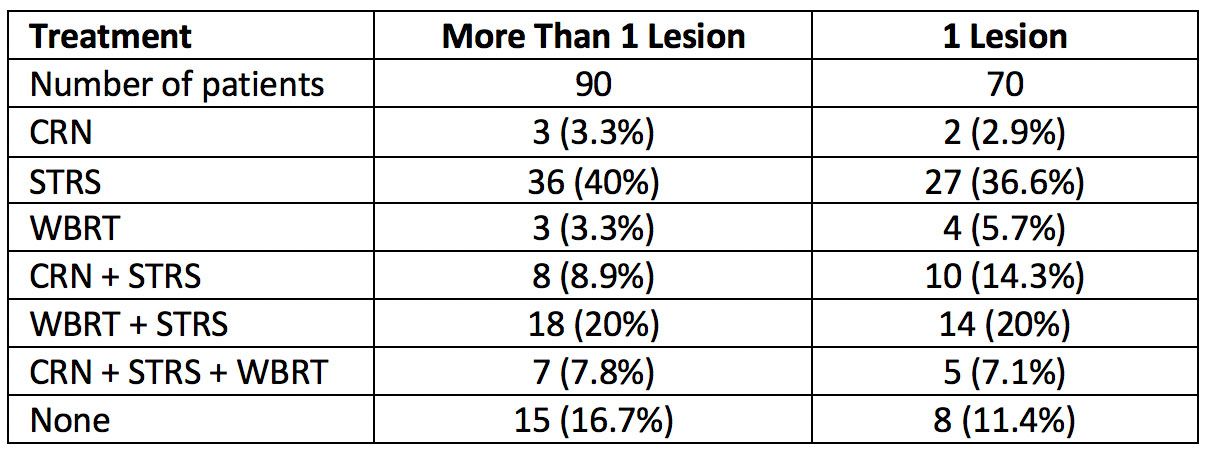
CRN indicates craniotomy; STRS, stereotactic radiosurgery; and WBRT, whole brain radiotherapy.
“The majority of patients in our cohort progressed to the brain while undergoing treatment for metastatic disease,” said Suarez-Sarmiento.
Besides initial screening, periodic surveillance is warranted to allow detection of asymptomatic disease, said Suarez-Sarmiento. The investigators concluded that those patients with a solitary RCC BM are less likely to develop CNS recurrence after local therapy and are ideal candidates for enrollment into aggressive clinical trials.
References:
- Suarez-Sarmiento A, Nguyen KA, Nolte A, Amirkhlz KG, Cheng M, Shusch B. Brain metastasis from renal cell carcinoma: an institutional study. Presented at: 2018 American Urological Association Annual Meeting; May 18-21, 2018; San Francisco, CA. Abstract MP66-0
- Motzer RJ, Bander NH, Nanus DM. Renal-cell carcinoma.N Engl J Med. 1996;335(12): 865-875. doi: 10.1056/NEJM199609193351207.
- Shuch B, La Rochelle JC, Klatte T, et al. Brain metastasis from renal cell carcinoma: presentation, recurrence, and survival.Cancer. 2008;113(7):1641-1648. doi: 10.1002/cncr.23769.
Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen




