ESMO Collaborative Group Sets Standard for Defining MSI and Implementing Testing
Microsatellite instability has been an FDA-indicated biomarker for immunotherapy since 2017, when the PD-1 inhibitor pembrolizumab was approved for patients with solid tumors found to be mismatch repair deficient or MSI high. Other approvals since then, such as for the combination of ipilimumab and nivolumab in patients with MSI-H/dMMR metastatic colorectal can­cer, have established the relevance of cancer thera­pies for tumors with this biomarker specifically rather than tumor histology alone.
Aldo Scarpa, MD, PhD

Aldo Scarpa, MD, PhD
Microsatellite instability (MSI)has been an FDA-indicated biomarker for immunotherapy since 2017, when the PD-1 inhibitor pembrolizumab (Keytruda) was approved for patients with solid tumors found to be mismatch repair deficient (dMMR) or MSI high (MSI-H).1Other approvals since then, such as for the combination of ipilimumab (Yervoy) and nivolumab (Opdivo) in patients with MSI-H/dMMR metastatic colorectal can­cer,2have established the relevance of cancer thera­pies for tumors with this biomarker specifically rather than tumor histology alone.
Recently, the European Society for Medical Oncology (ESMO) Translational Research and Precision Medicine Working Group published consensus recommendations for best practices for the detection of dMMR tumors in clinical practice. This document defines important terms related to MSI/dMMR, details testing methods, and clarifies relationships among MSI, tumor mutation­al burden (TMB), and PD-L1 expression.3
MSI is a diagnostic test for screening for the broad spectrum of Lynch syndrome[associated] cancers, but it is also a prognostic test for gastrointestinal cancers and a predicative marker for immunotherapy,”Aldo Scarpa, MD, PhD, director of Applied Research on Cancer-Network Research Centre for Applied Research on Cancer and chair of the Department of Pathology and Diagnostics at the University and Hospital Trust of Verona, Italy, said during a presentation of the working group’s data at the ESMO Immuno-Oncology Congress 2019, held December 11 to 14, 2019, in Geneva, Switzerland.4
Tumors that are dMMR accumulate mutations in regions of DNA called microsatellites, which are prone to mismatch errors; the result is the condition known as MSI. A hallmark of Lynch syndrome, MSI can occur in a variety of cancers, including colorectal, endome­trial, and gastric.
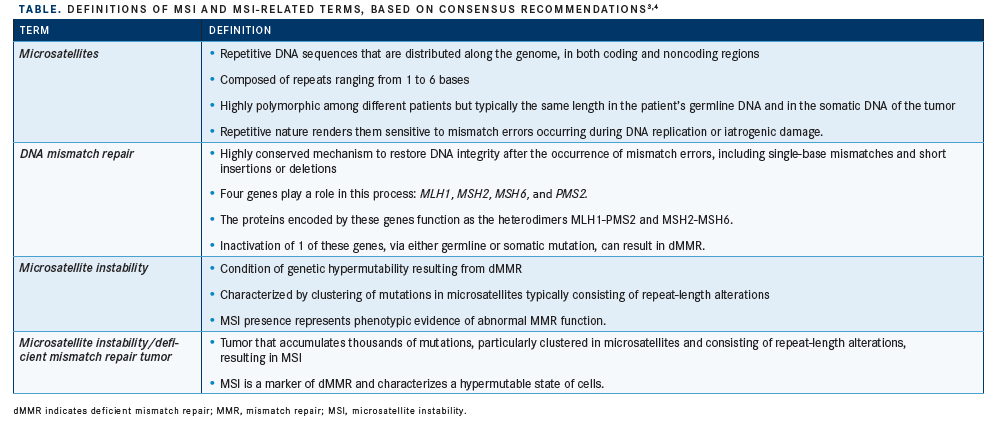
To promote the use of clear and consistent terminol­ogy in future research, the collaborative group estab­lished standardized definitions for MSI-related terms from a systematic review of 18 articles related to MSI. These definitions are outlined in theTABLE.3,4
Testing for MSI
To better understand the rationale behind testing methodologies, the collaborative group examined the mechanisms underlying DNA mismatch repair (MMR) across different solid tumors.
The MMR proteins form heterodimers consisting of MLH1 and PMS2 or MSH2 and MSH6. MLH1 and MSH2 are considered the “obligatory partners” in these protein pairs; alterations in them interfere with dimerization and result in proteolytic degradation of both proteins in the heterodimer. However, the same is not necessarily true of the “secondary partners,” PMS2 and MSH6, because other proteins may sub­stitute for them in the heterodimer. Therefore, func­tional heterodimers may be present despitePMS2orMSH6mutations.
For the spectrum of cancers associated with Lynch syndrome, immunohistochemistry (IHC) of all 4 MMR proteins is the first line of testing. Subsequently, MSIpolymerase chain reaction (PCR) molecular testing of specific microsat­ellite loci is indicated for cases in which IHC results are indeterminate, such as the loss of only 1 heterodimer subunit.
“When you have an alteration of a secondary partner, you may have an immunohistochemis­try [result that] is not informative because you do not have the loss of both partners,” Scarpa said. “This is because PMS2 may be substituted for PMS1 or MLH3, and MSH6 may be substitut­ed for MSH3. Alterations of secondary proteins may be compensated by other partners, and so the machinery is working.”
Normal cells with increased turnoversuch as mucosal cells, lymphocytes, and stromal cells— must serve as an internal positive control for IHC testing. Determinant IHC findings include positive results, in which tumor and control cells exhibit nuclear staining of comparable intensity, and negative results, in which control cells have nuclear staining but tumor cells do not. However, cases with negative staining of controls or weaker staining of tumor cells compared with controls require verification by MSI-PCR, which has the highest specificity and sensitivity.
For cancers not associated with Lynch syn­drome, the consensus group touted the advan­tages of next-generation sequencing (NGS), which can couple analyses of MSI and TMB.3In a study analyzing sequence data from 5930 can­cer samples, investigators found MSI-H tumors in 14 of the 18 cancer types studied, with inci­dences ranging from about 30% for endometrial cancer to <1% for thyroid carcinoma.5In a sim­ilar study, MSI was detected in 27 of 39 cancer types analyzed, mostly at low proportions; only 4 types had an MSI-H frequency >5%.6
“We cannot imagine [developing] these tests to analyze all these cases unless we use NGS,” Scarpa said. “In [cancers of] other organs out­side Lynch syndrome, we do not understand how to work with immunohistochemistry [to determine] the real partners of MMR. [With NGS], you can analyze several dozen genes to get information about mutations, loss, amplifi­cations, and copy-number alterations. Moreover, you have the mutational spectrum, which [refers to] the types of combinations of mutations that may happen through different mechanisms.”
PD-L1 Expression
From the 18 articles selected for systematic review, the collaborative group attempted to identify associations with immunotherapy response among 3 biomarkers: high TMB PD-L1 expression on tumor cells, and MSI. In total, 4186 patients were positive for at least 1 of the biomarkers, with the simultaneous presence of all 3 in 2.9% of cases (FIGURE).3 Significantly higher (P<.05) rates of positivity for all 3 biomarkers were observed in patients with colorectal and esophagogastric adenocar­cinomas, at 12.8% and 14.6%, respectively.3
Notably, the majority of patients with col­orectal cancer who had MSI also had high TMB, and vice versa. Positivity for both bio­markers (but not PD-L1) accounted for 31.4% of patients, indicating a high concordance between the 2 indices. Patients with MSI alone or high TMB alone accounted for just 1.7% and 8.7%, respectively, of patients with colorectal tumors. Patients with PD-L1 expression alone made up 43.6% of the population.3
Investigators observed similar concordance in patients with esophagogastric adenocarci­nomas, with 13.1% of tumors exhibiting both high TMB and MSI (but not PD-L1). High TMB or MSI alone was observed in 3.7% and 5.1% of patients, respectively. In total, 14.6% of patients in this population expressed all 3 biomarkers simultaneously.
In endometrial cancer, high TMB was almost always accompanied by MSI; however, the inverse correlation was not observed. Among patients with this cancer, 25.8% expressed both biomarkers (but not PD-L1), 19.9% had MSI only, and 4.9% had high TMB only. In 12.8% of patients, the tumors expressed all 3 biomarkers.
MSI was absent in melanoma cases and present in only a small number of cases of nonsmall cell lung cancer.
In all cancer types studied, PD-L1 expression was not found to necessarily co-occur with other biomarkers, and it was the most frequently occurring biomarker in most tumor types.
Practical Applications
The consensus group concluded that clinicians should perform first-line MSI testing using IHC for all 4 MMR-associated proteins for the cancer types frequently associated with Lynch syndrome, which include endometrial, intes­tinal, gastric, and ovarian cancers, as well as esophageal adenocarcinoma and glioblas­toma. In cases of indeterminate IHC results, second-line testing should be performed using a molecularly based assay, with MSI-PCR as the preferred method. For rare cancer types and those not associated with Lynch syn­drome, MSI testing should be performed using NGS. The group also noted that although cor­relations with TMB and PD-L1 may be useful for future prognostication, MSI-H tumors do not need to express either of these biomarkers to necessitate use of immunotherapy.
Ongoing research advancing the role of MSI as a biomarker for immunotherapy responses and clarifying its relationship with other bio­markers will continue to elucidate the role of MSI in the treatment of solid tumors.
References
- FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication. FDA website. bit.ly/35PW6zI. Updated May 30, 2017. Accessed January 13, 2020.
- FDA grants accelerated approval to ipilimumab for MSI-H or dMMR metastatic colorectal cancer. FDA website. bit.ly/2FL0G7F. Updated July 11, 2017. Accessed January 13, 2020.
- Luchini C, Bibeau F, Ligtenberg MJL, et al. ESMO recommendations on microsatellite instability testing for immunotherapy in cancer, and its relationship with PD-1/PD-L1 expression and tumor mutational burden: a systematic review-based approach.Ann Oncol. 2019;30(8):1232-1243. doi: 10.1093/annonc/mdz116.
- Scarpa A. Consensus on MSI/MMR determination to select patients eligible for anti-PD1 therapies. Presented at: European Society for Medical Oncology Immuno-Oncology Congress 2019; December 11-14, 2019. Geneva, Switzerland. bit.ly/2Rdq1MX.
- Hause RJ, Pritchard CC, Shendure J, Salipante SJ. Classification and characterization of microsatellite instability across 18 cancer types [erratum in Nat Med. 2018;24(4):525. doi: 10.1038/nm0418-525a] [erratum in Nat Med. 2017;23(10):1241. doi: 10.1038/nm1017-1241a].Nat Med. 2016;22(11):1342-1350. doi: 10.1038/nm.4191.
- Bonneville R, Krook MA, Kautto EA, et al. Landscape of microsatellite instability across 39 cancer types [published online October 3, 2017].JCO Precis Oncol. doi: 10.1200/PO.17.00073.
