D-VRd Enhances MRD Negativity and Survival Rates in Multiple Myeloma
Paula Rodríguez Otero, MD, PhD, discussed the deepening of response and minimal residual negativity during maintenance in the PERSEUS study for patients with multiple myeloma.
Paula Rodríguez Otero, MD, PhD

Deep responses and sustained minimal residual disease (MRD) negativity at both 10-5 and 10-6 levels were observed among patients with transplant-eligible multiple myeloma treated with an induction regimen of of daratumumab (Darzalex) and hyaluronidase-fihj in combination with bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone (D-VRd) followed by a maintenance regimen of daratumumab plus lenalidomide, according to findings from the phase 3 PERSEUS study (NCT03710603).1
Data presented at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting also showed that in the D-VRd arm, higher rates of complete response at the end of consolidation were seen (44.5%) vs in the VRd arm (34.7%), as well as maintenance (87.9% vs 70.1%). Rates of MRD negativity at 10-6 increased over time and were consistently higher in the D-VRd vs VRd arm at 12, 24, and 36 months with rates being 43.9% vs 20.9% (P =.0001), 57.7% vs 27.4% (P =.0001), and 63.9% vs 30.8% (P =.0001), respectively.1
Higher rates of sustained MRD negativity at 10-6 for at least 12 months were seen in the D-VRd arm at 47.3% compared with in the VRd arm at 18.6% (P <.0001). At 48 months, the progression-free survival (PFS) rates were 84.3% and 67.7% in the D-VRd and VRd arms, respectively (HR, 0.42; 95% CI, 0.30-0.59; P <.0001).
“This is the newest standard but, in the future, will be challenged with [chimeric antigen receptor (CAR) T’s], bispecifics, and more,” said Paula Rodríguez Otero, MD, PhD, in an interview with Targeted OncologyTM.
In the interview, Rodríguez Otero, University Clinic of Navarra, Pamplona, Spain, further discussed the deepening of response and MRD negativity during maintenance in the PERSEUS study.
Targeted Oncology: Can you discuss the design of the PERSEUS study?
Rodríguez Otero: PERSEUS is a phase 3, randomized study that enrolled patients with newly diagnosed multiple myeloma that were eligible for transplant with an age between 18 to 70 years. The study had a 1:1 randomization. Patients that were allocated to the standard arm received VRd induction, 4 cycles, followed by single transplant, and then 2 cycles of consolidation, then maintenance until disease progression. For patients allocated to the experimental arm, they receive D-VRd 4 cycles, single transplant, 2 cycles of consolidation and D-R maintenance for at least 2 years with the possibility of having a response adapted therapy. For patients that were MRD-negative, they could have stopped data and continued with lenalidomide until disease progression. Patients that were MRD-positive continued on D-R.
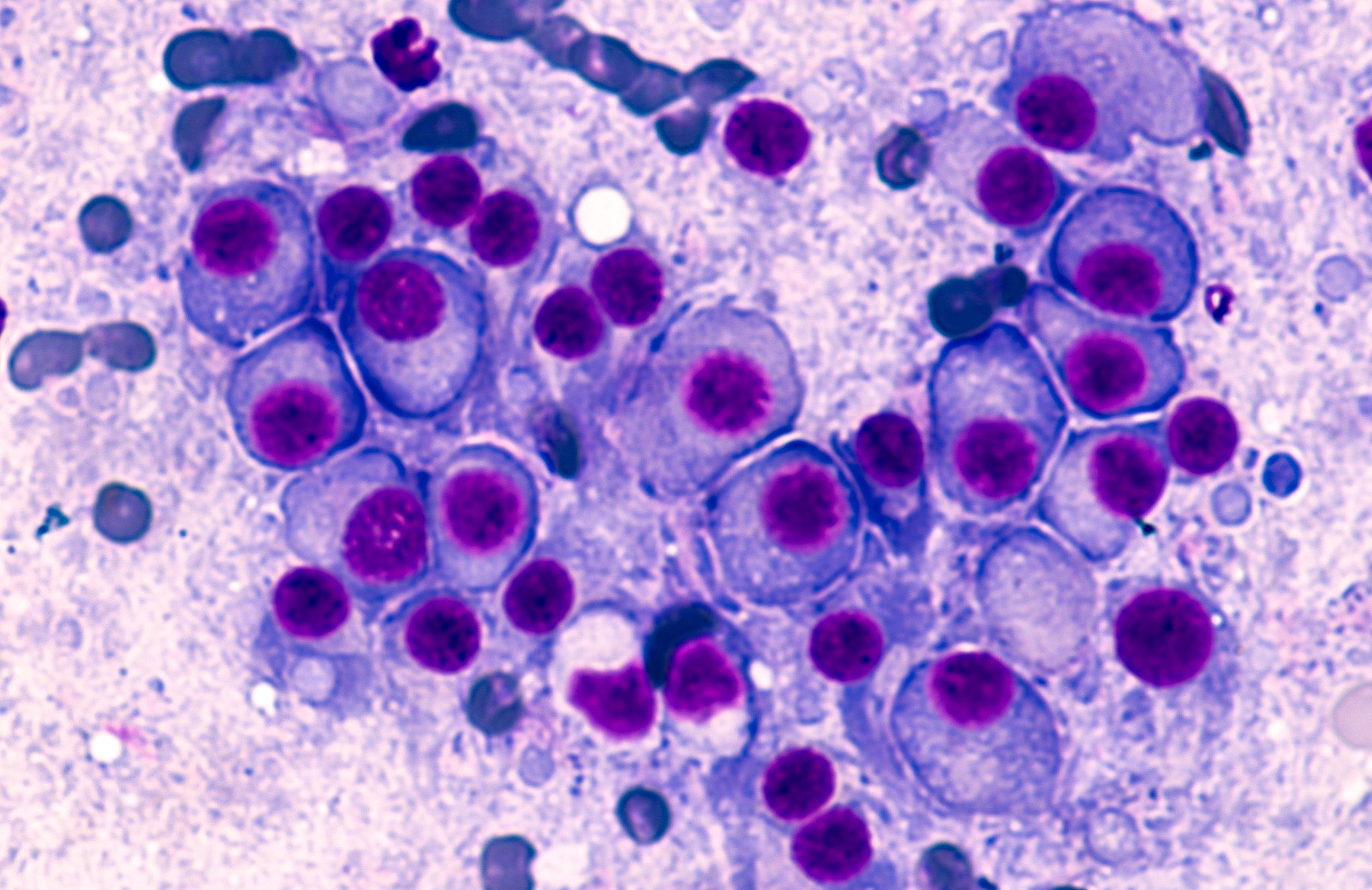
Multiple Myeloma: © David A Litman - stock.adobe.com
What previous data from the study can you share?
The trial was first presented at the last [American Society of Hematology Annual Meeting] meeting, and the the summary of the results was that D-VRd, the induction consolidation and maintenance, was associated with a significant improvement in progression-free survival with a 58% reduction in the risk of progression or death for patients treated with the daratumumab-containing arm, and that D-VRd also was associated with an increase in the depth of response and the proportion of patients that achieve MRD negativity or sustained MRD negativity.
What were the updated findings presented at ASCO 2024?
We [focused] on the maintenance part and most importantly, the minimal residual disease negativity data. In summary, the key takeaways of the presentation are that D-VRd induction consolidation and D-R maintenance increased the proportion of patients that achieved MRD negativity, both at 10-5 and at 10-6 as compared with VRd followed by lenalidomide alone. We do see a clear deepening of the responses throughout the treatment, and more importantly, during the maintenance phase. This deepening of the response is higher in the daratumumab-containing arm as compared with the VRd plus lenalidomide arm. We also see a higher proportion of patients that achieved sustained MRD negativity, both lasting for 12 months or longer, and also 18 months or longer, both 10-5 and 10-6, and this is higher in the daratumumab-containing arm.
For MRD rates and sustained MRD negativity, if we analyze the subgroup data, we do see consistent PFS benefit in favor of D-VRd across all different subgroups of patients, including older age or high-risk disease. There is also the presentation that has been focused on the high-risk patient population that here is defined as deletion 17p translocation 14 or translocation 16. And again, we see that patients that were treated with D-VRd induction, consolidation and maintenance achieved a higher proportion of MRD-negative rates, both 10-5 and more importantly, also 10-6. Also, patients with high-risk disease treated with that daratumumab and VRd had a higher rate of sustained MRD negativity. This translated into a benefit in progression-free survival.
Finally, and I think that this is an important piece of information, the proportion of patients that were able to convert from being MRD-positive at the end of consolidation to MRD-negative or sustained MRD negativity was also higher for patients treated with D-VRd induction, consolidation, and D-R maintenance as compared with patients treated in the standard arm. All this data highlights this new platform, so D-VRd induction, consolidation, and D-R maintenance, as the new standard of care for the management of these transplant-eligible, newly diagnosed [patients with] myeloma.
What are the next steps for this research and beyond?
We need longer follow-up to see if we have this potential for cure. We know that achieving sustained MRD negativity, particularly if we go for a deeper threshold like 10-6, may identify patients that may be potentially cured. I think that longer follow-up in this study will show how many of these patients are able to sustain MRD negativity for more than 5 years. We can have more information about some subgroup analysis and in future congresses, we will know more data about high-risk populations. This is the newest standard, but in the future will be challenged with CAR Ts, bispecifics, and more.
REFERENCE:
Rodríguez-Otero P, Moreau P, Dimopoulos MA, et al. Daratumumab (DARA) + bortezomib/lenalidomide/dexamethasone (VRd) in transplant-eligible (TE) patients (pts) with newly diagnosed multiple myeloma (NDMM): Analysis of minimal residual disease (MRD) in the PERSEUS trial. J Clin Oncol. 2024;42(suppl 16):7502. doi:10.1200/JCO.2024.42.16_suppl.7502
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More