Conventional Views May Not Apply to All Triple-Negative Breast Cancers
Clinicians need to consider the inherent heterogeneity of each case of triple-negative breast cancer during diagnosis and treatment planning, said Stuart J. Schnitt, MD, because not all cases present the same way. During the 2018 Lynn Sage Breast Cancer Symposium, Schnitt reviewed the conventional views of TNBC and emphasized that they may not fit all cases of TNBC.
Stuart J. Schnitt, MD
Clinicians need to consider the inherent heterogeneity of each case of triple-negative breast cancer (TNBC) during diagnosis and treatment planning, said Stuart J. Schnitt, MD, because not all cases present the same way.
Schnitt, chief of breast oncologic pathology at the Dana-Farber/ Brigham and Women’s Cancer Center, reviewed the conventional views of TNBC and emphasized that they may not fit all cases of TNBC during a presentation at the 2018 Lynn Sage Breast Cancer Symposium.1
“Clinicians should view TNBC as an umbrella term rather than a specific diagnosis,” he said.
TNBC, which comprises about 15% of breast malignancies, is more common among young women and African American women. The disease cannot be managed with endocrine therapy or HER2-targeted therapy and is often associated withBRCA1germline mutations and somatic inactivation.
Compared with other types of breast cancer, TNBC is more likely to be high grade and less likely to involve the lymph nodes, Schnitt said. Patients with TNBC face a greater risk for brain and lung metastases. They also have worse breast cancerspecific survival and overall survival rates, even after adjusting for age, stage, race, grade, and adjuvant chemotherapy.
According to Schnitt, TNBC was initially thought of as a surrogate for basal-like breast cancers identified by gene expression profiling. “However, we’ve learned that not all TNBCs are basal like, and not all basal-like breast cancers are triple negative,” he said. “What’s more, TNBCs are a heterogeneous group, since we have used RNA and DNA profiling to identify additional molecular subtypes.”
There are 4 such stable subtypes: luminal androgen receptor (AR), mesenchymal, basal-like immune suppressed, and basal-like immune activated. According to Schnitt, the TNBC subtypes have different response rates to neoadjuvant chemotherapy. Treatments that may preferentially benefit various subtypes in clinical trials include AR antagonists, immune checkpoint inhibitors, and CDK4/6 inhibitors.
Importantly, physicians now know that there are low-grade forms of TNBC, including adenoid cystic carcinoma, secretory carcinoma, acinic cell carcinoma, and low-grade metaplastic carcinoma. Low-grade metaplastic carcinoma is further divided into low-grade adenosquamous and low-grade fibromatosis-like types (TABLE).1
“Some [types] are histologically low grade and have a more indolent clinical course than conventional TNBC,” Schnitt said.
The low-grade forms of TNBC cluster in basal-like or claudin-low groups by gene expression profiling and are all relatively rare. Adenoid cystic carcinoma and secretory carcinoma are underpinned by distinctive, recurrent genetic alterations, Schnitt said.
Unfortunately, decisions regarding appropriate local and systemic therapy must be made based on limited data, as most of the literature consists of small, retrospective series and case reports. Furthermore, data from the large national registries, like the Surveillance, Epidemiology, and End Results Program, usually do not include pathology review, rendering them less useful in these cases.
Patients who develop adenoid cystic carcinoma, a rare form of the disease that comprises only about 0.1% of all breast carcinomas, are usually in their 50s or 60s. Approximately half of these masses are located in the subareolar or central region of the breast. These carcinomas may be detected mammographically or clinically, and they are often tender or painful. They show a variety of histological patterns and contain a dual cell population of epithelial cells and myoepithelial cells.
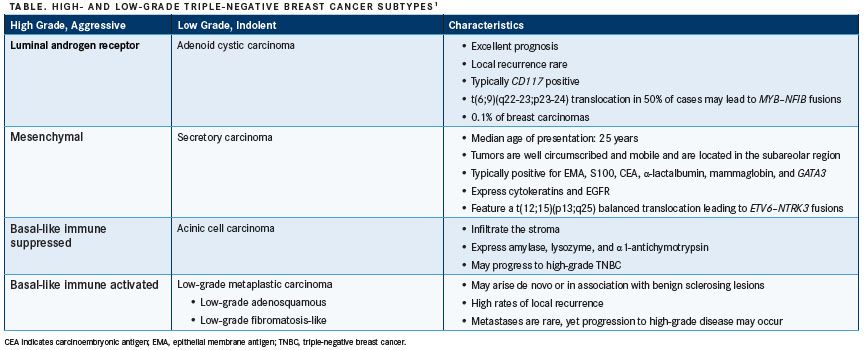
Adenoid cystic carcinomas are usually triple negative, although rare cases have been estrogen receptor positive, said Schnitt. They are typicallyCD117(c-KIT) positive. A characteristic feature that occurs in about 50% of cases is a t(6;9)(q22-23;p23-24) translocation, which consistently results inMYBNFIBfusions.2
“Deregulation and overexpression of MYB and its target genes is a key oncogenic event in this tumor type, regardless of origin site,” Schnitt said. Patients with adenoid cystic carcinoma have an excellent prognosis, although rare cases of local recurrence, lymph node involvement, and distant metastases have been reported.
Formerly known as juvenile breast cancer, secretory carcinoma makes up <0.15% of all breast cancers. The median age of patients at presentation is 25 years, although secretory carcinoma can occur at any age. Masses are typically well circumscribed and mobile and are in the subareolar region. These tumors are typically positive for epithelial membrane antigen, S100, carcinoembryonic antigen, a-lactalbumin, mammaglobin, and GATA binding protein 3. They also express basal cytokeratins and EGFR.
Secretory carcinomas feature a t(12;15)(p13;q25) balanced translocation leading toETV6NTRK3fusions. Patient outcomes are favorable overall, especially in children and young adults, although secretory carcinoma may be more aggressive in older patients. Late recurrences, or those happening more than 20 years later, have been recorded.
Acinic cell carcinomas infiltrate the stroma in a haphazard, microglandular pattern. Cells can have clear to finely granular or coarsely granular cytoplasm and express amylase, lysozyme, and α1-antichymotrypsin. Patients have a favorable outlook, although these carcinomas may progress to high-grade TNBC in some cases.
Low-grade metaplastic carcinomas may arise de novo or in association with benign sclerosing lesions. These are histologically bland tumors, said Schnitt, with high rates of local recurrence. Metastases are rare, although these tumors may progress to higher-grade metaplastic carcinomas.
References:
- Schnitt, SJ. All triple negative breast cancers are not created equal. Presented at: 20th Annual Lynn Sage Breast Cancer Symposium; October 11-14, 2018; Chicago, IL.
- Persson M, Andrén Y, Mark J, Horlings HM, Persson F, Stenman G. Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck. Proc Natl Acad Sci U S A. 2009;106(44):18740-18744. doi: 10.1073/pnas.0909114106.
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More