CART-ddBCMA Achieves 100% Response Rate in RRMM
Matthew J. Frigault, MD, MS, discussed follow-up data on the efficacy and safety of CART-ddBCMA for the treatment of patients with relapsed/refractory multiple myeloma, particularly in later-line settings.
Matthew J. Frigault, MD, MS
Promising efficacy and safety results were observed with CART-ddBCMA when used for the treatment of heavily pretreated patients with relapsed/refractory multiple myeloma (RRMM), according to 1 year or more follow-up data from a phase 1 trial.1
CART-ddBCMA is a modified chimeric antigen receptor (CAR) T-cell therapy that targets BCMA. The agent is manufactured and designed to specifically treat patients with RRMM.
Among heavily pretreated patients who had a median of 4 prior lines of therapy, the overall response rate (ORR) with CART-ddBCMA was 100%, including high rates of complete response (CR) and stringent CR (sCR) at 76% and 92% for very good partial response. Responses deepened over time, with some converting to CR/sCR as late as month 12.
Additional findings showed there to be 86% minimal residual disease (MRD) negativity at 10-5. The median duration of response, progression-free survival (PFS), and overall survival were not reached after 22 months follow-up, and the 6-month, 12-month, and 18-month PFS rates were estimated at 92%, 74%, and 67%, respectively.
Moreover, durable responses were observed even in patients with high-risk features, including extramedullary disease, high bone marrow plasma cells, and high beta-2 microglobulin. The therapy also had a favorable safety profile with manageable cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). No delayed neurotoxicity or Parkinsonian-like symptoms were observed.
Based on these findings, the dose of 115 ± 10 ×106 cells has been recommended for the phase 2 study, and these data support further investigation.
“I believe in this product and I think a lot of other people do, both from an efficacy and a safety standpoint. I hope to be able to move this into at least a later-line setting where we can provide it to patients,” Matthew J. Frigault, MD, MS, told Targeted OncologyTM, in an interview.
In the interview, Frigault, Harvard Medical School, clinical director of the cellular therapy program at Massachusetts General Hospital Cancer Center, discussed follow-up data which highlighted the promising efficacy and safety of CART-ddBCMA for the treatment of patients with RRMM, particularly in later-line settings.
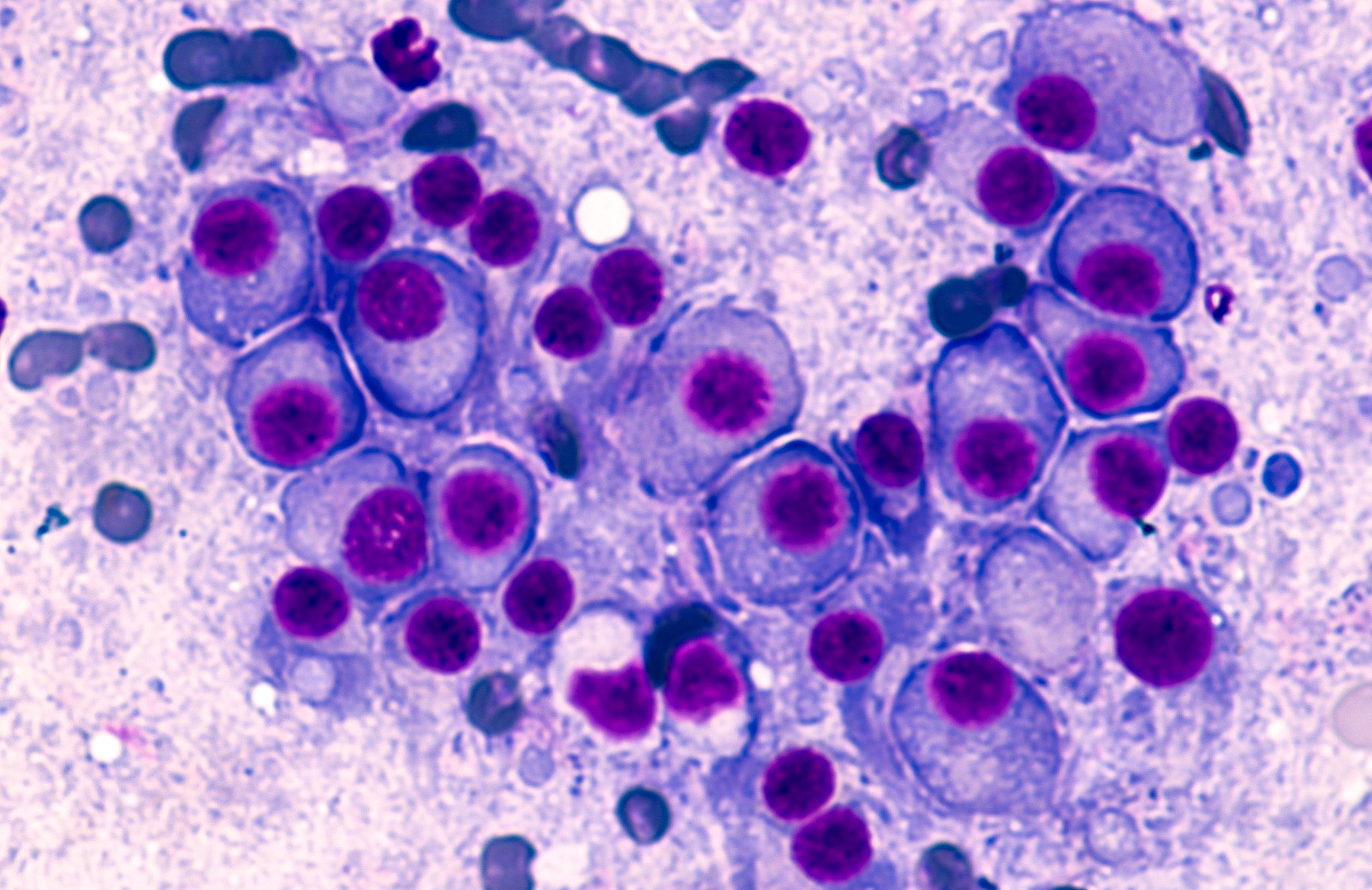
Multiple Myeloma: © David A Litman - stock.adobe.com
Targeted Oncology: Can you provide an overview on the study that focused on the follow-up of CART-ddBCMA therapy in RRMM?
Frigault: This was a phase 1 study of a CAR called CART-ddBCMA, a dose-escalation study with an expansion cohort that looked at 2 doses, 100 million and 300 million cells, in relapsed/refractory multiple myeloma that had to be exposed to all 3 classes, have a minimum of 3 prior lines of therapy, and have no measurable disease at the time of infusion. What we found is that we treated around 38 patients, we enrolled 42 patients, 2 of whom unfortunately couldn't get treated because they had issues prior to cell infusion. But of those 38 patients, we had a response rate of 100%. So all comers, everyone had a response. When you look across different high-risk groups, no individual group stuck out as having inferior outcomes. It was impressive to see in a phase 1 study.
What was the primary end point of the study and how does it contribute to the understanding of CART-ddBCMA?
The primary end point for any phase 1 study is always going to be safety, looking for the recommended phase 2 dose, looking for any [dose-limiting toxicities] or the [maximum tolerated dose]. What we found is that we tested both those levels, 100 and 300 million cells, and we ended up electing to go for dose level 1 at 100 million. Safety-wise, they were almost comparable. There was 1 episode of grade 3 or higher CRS at dose level 2. In both cohorts at dose level 1 and dose level 2,there was 1 case of grade 3 or higher ICANS or neurotoxicity. Looking at the kinetics of expansion of the cells, everything is similar, which is why we elected to go with the 100 million cell dose. Then we proceeded forward with the expansion cohort.
Who was included in the trial?
These [were patients with] relapsed/refractory myeloma [who had] 3 prior lines of therapy at a minimum. They had to have been exposed to at least 3 main classes of [immunomodulatory drugs and proteasome inhibitors, and an anti-CD38 antibody]. All of these patients were triple refractory, meaning that they were refractory to at least 1 of the major drug classes with the majority of the patients also being penta-exposed, if not penta-refractory. They exhausted all prior therapies. They had to have appropriate renal function and organ function for a phase 1 study and [they] had to have measurable disease by IMWG in order to proceed forward with screening.
What was the duration of follow-up? Why is longer term follow-up important for assessing this therapy?
These are therapies that are given in basically a 1-month treatment period with infusion follow-up of those first 30 days. These are therapies that theoretically can have years, if not more, of ongoing clinical benefit. Initially, we had reported shorter term follow-up and now we have around 26.5 months median follow-up. We're following patients for an extended period of time. Importantly, at that 26.5-month time point, we haven't reached our median PFS, so more than half of the patients are still in an ongoing response, progression-free, and alive at that time point. We can reliably tell patients that 2 years out, more than half of the patients are still benefiting from something they received 2 years prior, which is why more follow-up matters.
We also have more information on safety. With that median follow-up of the 26.5 months, we haven't seen atypical neurotoxicities, movement disorders, Parkinsonism, cranial nerve neuropathies, things that we're starting to see in the real-world with things like [ciltacabtagne autoleucel (cilta-cel; Carvykti)]l and in some cases, [idecabtagene vicleucel (ide-cel; Abecma)]. It emphasizes that with long-term follow-up, we still have an efficacious and safe product to provide to patients.
What were the key findings and outcomes observed during this follow-up period?
The key outcomes that are important to take home are 1, with a median follow-up of 26.5 months, we have not met our median PFS. That includes all high-risk subgroups. Patients with high-risk cytogenetics, patients with extramedullary disease, patients over the age of 65, patients with high tumor burden: Everyone seems to be benefiting from this product, regardless of what kind of high-risk features they may have coming in. When you look at the overall projected estimated PFS based on Kaplan Meier curves, it's looking like it's going to ffall around 28 months, but those data are still relatively early and evolving, so that could prolong. Additionally, every patient had a response with this. We had around an 89% MRD negativity rate down to 10-5 or lower, and it was safe without any atypical neurotoxicity signal popping up at any later time point.
Are there any safety data that you could share?
So far in terms of safety for the dose level 1, which was basically the dose level we're using in the phase 2 study, the iMMagine-1 study [NCT05396885], we only had 1 case of grade 3 or higher ICANS. We had no case of grade 3 or higher CRS, [and] typical cytopenias through day 30. As we've seen in all CAR T-cell studies, as I mentioned, there's no sign or signal of any atypical movement disorders.
Based on these follow-up data, what are the potential implications for incorporating this therapy into clinical practice?
We are excited to get an approval, if we could, and move it into clinical management. I believe in this product and I think a lot of other people do, both from an efficacy and a safety standpoint. I hope to be able to move this into at least a later-line setting where we can provide it to patients. Clinically, we do still have a significant manufacturing bottleneck, especially if we're talking about using CAR T cells in earlier lines. The more highly effective and safe therapies we have to offer to patients, the better. I look forward to seeing if we can move this into early lines of therapy as well.
What are the next steps for this research?
We currently are enrolling in the iMMagine-1study, which is the pivotal phase 2 study for the approval of [anitocabtagene autoleucel (anito-cel; Arcelix)] for late-stage multiple myeloma. I look forward to moving this into earlier lines as conversations are ongoing.
In the myeloma space as a whole, what have been some of the most impactful updates?
We have highly effective therapies across multiple different classes, and that's exciting for patients. One of the big take homes is that what we're seeing across class of drug, whether it be a T-cell engager, a CAR T-cell, any kind of monoclonal antibody, or a kind of quad-based upfront regimen, minimal residual disease-negative is 1 of the best prognostic factors for who's going to have a durable response. The duration of MRD-negativity predicts a prolonged and durable progression-free survival.
When I look across different classes, this is a theme that we're seeing. I am excited to see that CAR T cells have a high MRD negativity rate and can have a sustained MRD negativity for a prolonged period of time. I think we're starting to see the incorporation of newer therapies. I think we're seeing more upfront combinations of therapies, and so what that means is that moving CAR T cells to earlier lines makes a lot of sense, because patients are going to get exposed to more agents sooner in their treatment, meaning that they're going to be refractory potentially sooner. In that setting, we need an early-line CAR T.
REFERENCE:
Frigault MJ, Bishop MR, Rosenblatt J, et al. Phase 1 study of CART-ddBCMA for the treatment of subjects with relapsed and refractory multiple myeloma. Blood Adv. 2023;7(5):768-777. doi:10.1182/bloodadvances.2022007210
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More