A Little STING May Enhance the Immune System Against Cancer
Despite their promise, checkpoint inhibitors are not effective in every patient, and research suggests the STING (stimulator of interferon genes) pathway may hold important clues as to why some tumors fail to respond.
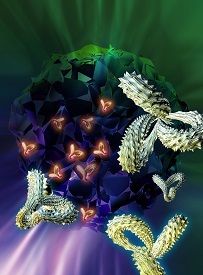
Immune Cells
Checkpoint inhibitors have generated a lot of excitement in oncology for the remarkable tumor responses they produce in some patients. Checkpoint inhibitors essentially let the immune system off the leash so that it goes after the cancer cells more effectively and with less toxicity than traditional chemotherapy. Despite their promise, checkpoint inhibitors are not effective in every patient, and research suggests the STING (stimulator of interferon genes) pathway may hold important clues as to why some tumors fail to respond.1,2
Woo et al have shown that innate activation of the STING pathway through detection of cytosolic DNA (DNA outside the cell nucleus)3initiates a natural immune response against tumors, which starts with the production of type I interferons (IFNs) and ends with the release of killer T cells primed to target specific tumor antigens.1When researchers implanted highly immunogenic tumors in mice without the gene that produces STING, the tumors grew and progressed. The same tumors were rejected in wild-type mice.2
Woo et al found that mice bred without the gene that produces STING had impaired T-cell responses, possibly due to insufficient expression of cytokines, chemokines, and other T-cell costimulatory factors.1They also found that checkpoint blockade therapies were ineffective in the STING-deficient mice but not in the wild-type mice, underscoring the probable role of STING in mounting an effective immune response.
A different study has shown that STING mediates the antitumor effects of high-dose radiotherapy (RT) in mice, with the resultant DNA damage triggering an immune response.4The antitumor effects were only observed in mice capable of producing STING, however; the null mice had no IFN production, a blunted T-cell response, and no tumor response. When the researchers treated the tumors in wild-type mice with cyclic guanosine monophosphate-adenosine monophosphate (cGAMP) to enhance STING activation after RT, the response was even more robust, with 70% of the mice rejecting the tumors.
Although some people mount a spontaneous T-cell response in response to cancer, it is typically insufficient to eliminate the tumor. Both studies suggest that mechanisms for boosting STING activation might improve the innate immune response to cancer. STING agonists might also allow some patients unresponsive to immunotherapies to achieve a response or increase the effectiveness of these agents.
The potential for harnessing the STING signaling pathway to improve the effectiveness of anticancer immune therapies is behind Novartis’ recently announced collaboration with Aduro Biotech.5 Arduro has been working to develop small-molecule cyclic dinucleotides that target the STING pathway.
“Immunotherapy is one of the exciting frontiers in oncology today. Current approaches with checkpoint inhibitors and T-cell modulation are potent but only in select tumor types. STING agonists have the potential to fully activate the immune system to attack a broader range of tumors,” said Mark Fishman, president of Novartis Institutes for Biomedical Research, in a press release announcing the partnership.5Novartis also announced it had hired Glenn Dranoff, MD, formerly from the Dana Farber Cancer Institute, to lead a new research group focused on developing cancer immunotherapies.
Novartis already has a number of immunotherapies in the pipeline, including checkpoint inhibitors and chimeric antigen receptor T-cell (CAR-T) therapies. The drug CTL019, an investigational CAR-T agent, is currently being evaluated in phase II clinical trials, and trials for other investigational therapies may launch later this year.
As the data suggest, enhancing STING activation has the potential to make current immunotherapy agents more effective, but a recent letter to the editor that appeared in the New England Journal of Medicine warns of the possibility that combining immunotherapies could be too effective too quickly in some patients.6Chapman et al from Memorial Sloan Kettering Cancer reported the case of a 49-year-year-old woman being treated for metastatic melanoma in a clinical trial that combined the approved immunotherapy drugs ipilumumab and nivolumumab (NCT02186249). The woman had a large mass under her left breast. Three weeks after receiving the first dose of combined therapy, her tumor was completely goneand in its place was a large cavity. The tumor disappeared faster than the new tissue could regenerate. The authors warned that “an overly vigorous response” in a place like the small bowel or myocardium in a patient with melanoma “could have grave consequences.”6
As the frontier of immunotherapy continues to broaden and more immunotherapies are available to treat different types of cancers, careful consideration will be required before combining them. At the same time, reaching a place where the main concern is not whether a drug can eradicate a patient’s cancer but instead how to avoid eradicating the cancer too quickly is not the worst place to be.
References
- Woo SR, Leung M, Furdyna M, Gajewski TF. Innate immune sensing of a growing tumor in vivo occurs via the host sting pathway and involves mitochondrial DNA transfer from cancer cells to DCs.J Immunother Cancer. 2013;1(Suppl1):O19.
- Woo SR, Fuertes MB, Corrales L, et al. STING-dependent cytosolic DNA sensing mediates innate immune recognition of immunogenic tumors. Immunity. 2014;41(5):830-842.
- Eastin J. Every step you take: STING pathway key to tumor immunity. The University of Chicago Medicine & Biological Sciences website. http://sciencelife.uchospitals.edu/2014/11/20/every-step-you-take-sting-pathway-key-to-tumor-immunity. Published November 20, 2014. Accessed April 23, 2015.
- Deng L, Liang H, Xu M, et al. STING-dependent cytosolic DNA sensing promotes radiation-iInduced type I interferon-dependent antitumor immunity in immunogenic tumors.Immunity. 2014;41(5):843-852.
- Novartis accelerates cancer immunotherapy efforts with Aduro Biotech alliance and launch of new immuno-oncology research group [press release]. http://www.novartis.com/newsroom/media-releases/en/2015/1907119.shtml. Published March 30, 2015. Accessed April 22, 2015.
- Chapman PB, D’Angelo SP, Wolchok JD. Rapid eradication of a bulky melanoma mass with one dose of immunotherapy [letter to the editor]. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMc1501894. Published April 20, 2015. Accessed April 23, 2015. .