Guidelines Consider Use of Targeted Therapies in Colorectal Cancer
The use of targeted therapies in colon cancer has become increasingly important, with several options available for clinicans to choose between. In a review of recent updates incorporating molecularly targeted therapy use in the National Comprehensive Cancer Network guidelines, the evidence for these new recommendations are detailed in support of their use in patients with colon cancer.
WHERE TARGETED THERAPY FALLS IN COLON CANCER GUIDELINES
Treatment of stage I and II colon cancer is focused on surgical therapy with either colectomy or lymphadenectomy.1In some stage II cancers in which cancers has spread to nearby sites, adjuvant chemotherapy, such as folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine plus oxaliplatin (CAPEOX), may be used.2
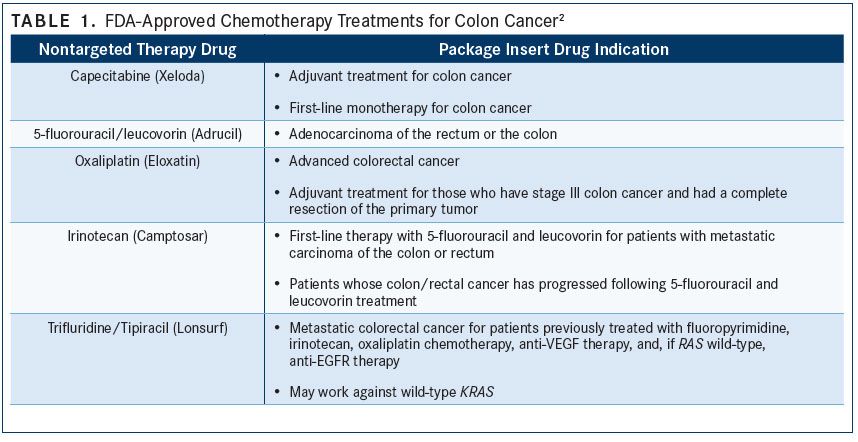
Stage III tumors are generally treated with surgery and adjuvant chemotherapy. Chemotherapeutic regimens may include FOLFOX, folinic acid, fluorouracil, and irinotecan (FOLFIRI), CAPEOX, fluorouracil, leucovorin, and oxaliplatin (FLOX), capecitabine, or 5-fluorouracil plus leucovorin (TABLE 12).
Currently, the use of targeted therapies is limited to patients with stage IV metastatic colon cancer. At this stage, patients who do not benefit from chemotherapy alone may experience an improved response if targeted therapy is added to treatment. However, the treatment choice may depend on whether the cancer is resectable.
Chemotherapeutic regimens in the metastatic setting may include FOLFOX, CAPEOX, FOLFIRI, FLOX, capecitabine, or fluorouracil plus leucovorin.2For patients with unresectable tumors, chemotherapy with or without bevacizumab (Avastin), chemotherapy plus panitumumab (Vectibix), or chemotherapy plus cetuximab (Erbitux) may be considered. Notably, use of EGFR inhibitors, such as panitumumab or cetuximab, is preferable for patients with left-sided tumors with wild-type KRAS or NRAS genes. Selection of EGFR inhibitors should also take into account BRAF V600E mutations, which may limit effectiveness.2
Some patients with unresectable, metastatic tumors may have another option: single-agent immunotherapy. Nivolumab (Opdivo) and pembrolizumab (Keytruda), both PD-1 inhibitors, can be used in this setting for patients with deficient mismatch repair (dMMR) or microsatellite instability-high (MSI-H) tumors.2Patients with advanced or metastatic disease who are not appropriate candidates for intensive therapy also may be considered for immunotherapy if they are positive for dMMR or MSI-H.2Additionally, immunotherapy is an option for biomarker-positive patients in subsequent lines of therapy.2
Universal MMR or MSI testing is recommended for all patients with a personal history of colon cancer to inform therapy decisions throughout the treatment paradigm. Patients with stage II MSI-H tumors may have a good prognosis and would not benefit from 5-FU adjuvant therapy.2
PHASE III TRIALS WITH TARGETED THERAPIES
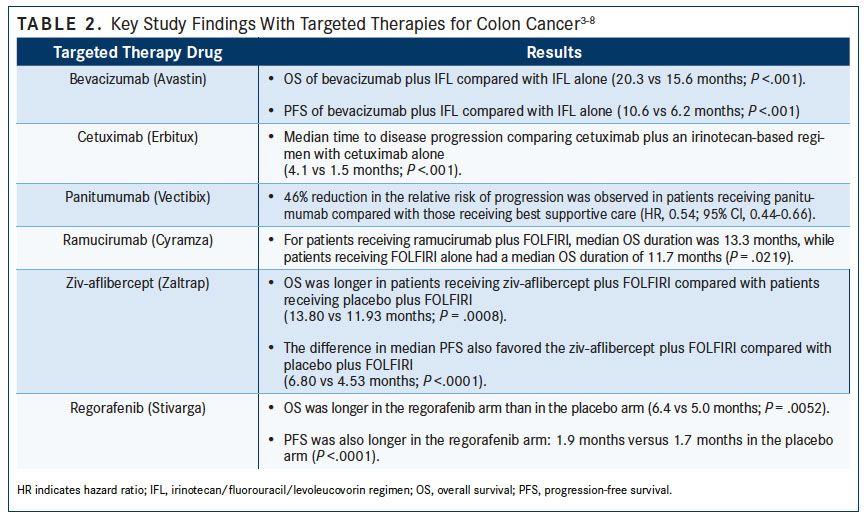
Six targeted therapies are currently used for the management of advanced colon cancer: bevacizumab, cetuximab, panitumumab, regorafenib (Stivarga), ramucirumab (Cyramza), and ziv-aflibercept (Zaltrap). Mechanistically, bevacizumab, ramucirumab, and ziv-aflibercept are anti-VEGF therapies, while cetuximab and panitumumab are anti-EGFR therapies. Unlike other available targeted treatments, regorafenib is a multikinase inhibitor, which inhibits VEGF, among other factors. (TABLE 23-8).
Bevacizumab
Bevacizumab was the first VEGF inhibitor approved for colon cancer. A trial by Hurwitz et al analyzed survival rates in patients receiving bevacizumab with irinotecan, fluorouracil, and leucovorin (IFL), versus IFL alone. Eligible patients included adults aged 18 years or older with a good ECOG performance status (defined as ECOG 0 to 1) and a life expectancy of greater than 3 months. Every 2 weeks, patients received either IFL with bevacizumab 5 mg/kg intravenously (IV), or IFL plus placebo. At the end of the trial, overall survival (OS) was longer in the group receiving bevacizumab plus IFL versus IFL alone (20.3 vs 15.6 months; P <.001). The median duration of progression-free survival (PFS) was improved for patients receiving bevacizumab plus IFL versus IFL alone (10.6 vs 6.2 months; P <.001).3
Cetuximab
Cetuximab is an anti-EGFR targeted treatment approved for use in colon cancer. Cunningham et al evaluated the safety and efficacy of cetuximab used in combination with an irinotecan-based regimen versus cetuximab alone. In this trial, patients with stage IV metastatic colon cancer expressing EGFR, refractory to irinotecan therapy, were randomized in a 2:1 ratio to receive either an irinotecan-based regimen with cetuximab or cetuximab monotherapy. In this trial, the median time to disease progression for the cetuximab and irinotecan combination therapy group was 4.1 months, while for the cetuximab group it was 1.5 months (P <.001).4
Panitumumab
Like cetuximab, panitumumab is an anti-EGFR therapy approved for the treatment of patients with colon cancer. VELOUR, an open-label phase III study, examined panitumumab plus best supportive care versus best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer (mCRC). Although no OS benefit was detected, a significant 46% reduction in the relative risk of progression was observed in patients receiving panitumumab compared with those receiving best supportive care (hazard ratio [HR], 0.54; 95% CI, 0.44-0.66).5
Ramucirumab
Ramucirumab is an anti-VEGF therapy for the treatment of patients with stage IV metastatic colon cancer. RAISE, a phase III study, compared use of ramucirumab plus second-line FOLFIRI versus FOLFIRI alone in patients with mCRC that progressed during or after first-line chemotherapeutic treatment. For patients receiving ramucirumab plus FOLFIRI, median OS duration was 13.3 months, while patients receiving FOLFIRI alone had a median OS duration of 11.7 months (P = .0219).6
Ziv-aflibercept
Ziv-aflibercept, which also is an anti-VEGF therapy, was studied in the VELOUR trial. Ziv-aflibercept plus FOLFIRI versus FOLFIRI alone were evaluated in the second-line treatment of mCRC. Patients had mCRC and failed first-line treatment on a regimen that included oxaliplatin, or had relapsed during or within 6 months of completion of an oxaliplatin-containing regimen. They were randomly assigned to receive either ziv-aflibercept plus FOLFIRI or placebo plus FOLFIRI. At the trial’s end, OS was longer in patients receiving ziv-aflibercept plus FOLFIRI compared with patients receiving placebo plus FOLFIRI (13.80 vs 11.93 months; P = .0008). The difference in median PFS also favored the ziv-aflibercept plus FOLFIRI treatment arm compared with placebo plus FOLFIRI (6.80 vs 4.53 months; P <.0001).7
Regorafenib
Regorafenib is a multikinase inhibitor that affects several signaling pathways; it blocks VEGF signaling. Regorafenib is intended for use after other lines of therapy for colon cancer have already failed. Grothey et al designed a trial to assess the safety and efficacy of regorafenib in patients with mCRC who had progressed after having received standard therapies. Patients were aged 18 years or older, had an ECOG performance status of 0 or 1, and had a life expectancy of at least 3 months. Patients were randomized in a 2:1 ratio to receive either regorafenib orally once a day or placebo. At the end of the trial, OS was longer in the regorafenib arm than in the placebo arm (6.4 vs 5.0 months; P = .0052). PFS was also longer in the regorafenib arm: 1.9 months versus 1.7 months in the placebo arm (P <.0001).8
ASPECCT TRIAL
Few trials in gastrointestinal cancers compare the efficacy and safety of targeted therapies within the same class; ASPECCT is 1 such trial. This noninferiority trial was designed to compare outcomes with panitumumab and cetuximab, 2 anti-EGFR targeted therapies. In this clinical study, limited to patients with chemotherapy-refractory mCRC, panitumumab was shown to be noninferior to cetuximab in all aspects evaluated, including OS, PFS, objective response rate (ORR), and safety outcomes. The median OS times were 10.2 months with panitumumab and 9.9 months with cetuximab (P = .0002 for noninferiority). Median PFS time was 4.2 months with panitumumab and 4.4 months with cetuximab. Finally, ORRs with panitumumab and cetuximab were 22% and 19.8%, respectively. Additionally, the safety profiles of the 2 medications were found to be similar.9
COMPARATIVE COST EFFECTIVENESS
Panitumumab Versus Cetuximab
An economic analysis using data from the original ASPECCT trial was performed to determine if there were cost benefits in using panitumumab versus cetuximab, as the medications proved to be noninferior to each other. The researchers concluded that panitumumab was superior to cetuximab in projected drug acquisition costs, mode of administration, and safety outcomes, for patients with wild-type KRAS who have mCRC. Panitumumab was also found to have better outcomes in terms of projected life-years (1.072 vs 1.051 life-years), and a larger gain in quality- adjusted life-years (QALYs) (0.736 vs 0.726 QALYs). The projected cost savings per patient was $9468.10
Although these findings seem to support use of panitumumab over cetuximab, several limitations of the economic analysis must be addressed prior to forming that conclusion. This analysis was based on the results of ASPECCT, a noninferiority trial.10In the ASPECCT trial, patients were required to have an ECOG score of 0 to 2, and to have adequate renal and hepatic function, which is not representative of many patients with mCRC.9Furthermore, the analysis is based on a semi-Markov model in which simulated groups of patients continually transition across different health states. These simulated outcomes may not reflect the actual patient outcomes or cost savings. Importantly, there was only a marginal difference of 0.01 QALY between agents (0.736 for panitumumab versus 0.726 for cetuximab).10Finally, the adverse effect profile included in the costs was largely focused on infusion reactions, which are known to vary across treatment centers and may detract from the universality of study findings.
Although findings from this analysis may suggest that panitumumab is more cost effective, more research is required before reaching this conclusion universally.10
Bevacizumab Versus Cetuximab
Several trials, including the KRK-0306 study, have compared bevacizumab and cetuximab. In the KRK-0306 trial, investigators evaluated outcomes in patients with KRAS-mutated tumors receiving either bevacizumab plus FOLFIRI or cetuximab plus FOLFIRI. ORRs were 44% in the FOLFIRI plus cetuximab combination therapy group versus 48% in the FOLFIRI plus bevacizumab combination therapy group. The median PFS duration was 7.5 months in patients receiving cetuximab versus 8.9 months in patients receiving bevacizumab. The median OS duration was 22.7 months with cetuximab and 18.7 months with bevacizumab. Although it is known that cetuximab is not effective in mutated KRAS tumors, from this trial it was clear that bevacizumab does not perform any better than cetuximab in this patient group. Researchers reported a greater incidence of acneiform exanthema in patients receiving cetuximab, and a higher rate of grade 3/4 hypertension among those receiving bevacizumab.11
A similar study evaluated bevacizumab versus cetuximab in combination with chemotherapy as first-line treatment in Chinese patients with metastatic colon cancer, and cetuximab and bevacizumab were found to have similar efficacy. The median PFS rates were 10.6 and 8.7 months in the bevacizumab and cetuximab groups, respectively (P = .316). The median OS was 27.7 months with bevacizumab versus 28.3 months with cetuximab (P = .510). The ORR for cetuximab versus bevacizumab was also not significantly different (53.5% vs 43.1%; P = .108).12In a trend, however, patients receiving cetuximab-based triplet therapy had a higher conversion rate to resectability compared with patients receiving bevacizumab-based triplet therapy (46.3% vs 28.8%; P = .058). In addition, in patients with peritoneal metastasis, bevacizumab proved superior to cetuximab in both PFS (9.6 vs 6.1 months; P <.001) and OS (26.3 vs 12.7 months; P = .006).12
In a third study, FIRE-3, which compared FOLFIRI in combination with either bevacizumab or cetuximab in patients with mCRC, rates of PFS were found to be similar between the 2 treatment arms: 10.0 and 10.3 months for patients treated with cetuximab plus FOLFIRI and bevacizumab plus FOLFIRI, respectively (P = .55). Median OS rates were also found to be similar between the 2 treatment arms (28.7 vs 25.0 months in the cetuximab and bevacizumab arms, respectively; P = .017). However, in an analysis limited to patients with wild-type RAS, there was an advantage in OS with cetuximab compared with bevacizumab (33.1 vs 25.6 months, P = .011).13
In the fourth and final study comparing bevacizumab and cetuximab in patients with wild-type KRAS colorectal cancer, median OS was 30.0 months in patients receiving cetuximab plus chemotherapy and 29.0 months in patients receiving bevacizumab plus chemotherapy (P = .08).14 Rates of median PFS times were also similar between the cetuximab and bevacizumab groups, with durations of 10.5 months and 10.6 months, respectively (P = .45). Finally, the respective response rates for cetuximab and bevacizumab were 59.6% and 55.2% (P = .13).14
CONCLUSION
Targeted therapy includes a novel group of treatments that may help improve outcomes for patients with metastatic colon cancer as monotherapy and, in some cases, when used in combination with chemotherapy. Targeted therapies are different from chemotherapy in that they target specific receptors that may promote cancer growth and survival. Because these drugs are reserved for patients with advanced cancer, few head-to-head trials have been performed. However, it is important to recognize the available evidence and possible differences among treatments both across and within treatment classes.
References:
- National Comprehensive Cancer Network (NCCN). NCCN guidelines for patients. Colon cancer. Version 1.2017. NCCN website. www.nccn.org/patients/guidelines/colon/files/ assets/common/downloads/files/colon.pdf. Updated June 6, 2017. Accessed October 2017.
- National Comprehensive Cancer Network (NCCN). Clinical practices in oncology (NCCN guidelines). Colon cancer. Version 2.2017. NCCN website. www.nccn.org/professionals/ physician_gls/pdf/colon.pdf. Published March 13, 2017. Accessed October 2017.
- Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335-2342. doi: 10.1056/NEJMoa032691.
- Cunningham D, Humblet Y, Siena S, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351(4):337-345. doi: 10.1056/NEJMoa033025.
- Van Cutsem E, Peeters M, Siena S, et al. Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy- refractory metastatic colorectal cancer. J Clin Oncol. 2007;25(13):1658-1664. doi: 10.1200/JCO.2006.08.1620.
- Tabernero J, Yoshino T, Cohn AL. Ramucirumab versus placebo in combination with second-line FOLFIRI in patients with metastatic colorectal carcinoma that progressed during or after first-line therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine (RAISE): a randomised, double-blind, multicentre, phase 3 study. [Correction to Lancet Oncol. 2015;16:499-508]. Lancet Oncol. 2015;16(6):e262. doi: 10.1016/S1470- 2045(15)70273-1.
- Van Cutsem E, Joulain F, Hoff PM, et al. Aflibercept plus FOLFIRI vs. placebo plus FOLFIRI in second-line metastatic colorectal cancer: a post hoc analysis of survival from the phase III VELOUR study subsequent to exclusion of patients who had recurrence during or within 6 months of completing adjuvant oxaliplatin-based therapy. Target Oncol. 2016;11(3):383- 400. doi: 10.1007/s11523-015-0402-9.
- Grothey A, Van Cutsem E, Sobrero A, et al; CORRECT Study Group. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):303- 312. doi: 10.1016/S0140-6736(12)61900-X.
- Price T, Kim TW, Li J, et al. Final results and outcomes by prior bevacizumab exposure, skin toxicity, and hypomagnesaemia from ASPECCT: randomized phase 3 non-inferiority study of panitumumab versus cetuximab in chemorefractory wildtype KRAS exon 2 metastatic colorectal cancer. Eur J Cancer. 2016;68:51-59. doi: 10.1016/j. ejca.2016.08.010.
- Graham CN, Maglinte GA, Schwartzberg LS, et al. Economic analysis of panitumumab compared with cetuximab in patients with wild-type KRAS metastatic colorectal cancer that progressed after standard chemotherapy. Clin Ther. 2016;38(6):1376-1391. doi: 10.1016/j.clinthera.2016.03.023.1016/j.clinthera.2016.03.023.
- Stintzing S, Fischer von Weikersthal L, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer-subgroup analysis of patients with KRAS: mutated tumours in the randomised German AIO study KRK-0306. Ann Oncol. 2012;23(7):1693-1699. doi: 10.1093/annonc/ mdr571.
- Bai L, Wang F, Li ZZ, et al. Chemotherapy plus bevacizumab versus chemotherapy plus cetuximab as first-line treatment for patients with metastatic colorectal cancer: results of a registry-based cohort analysis. Medicine (Baltimore). 2016;95(51):e4531. doi: 10.1097/MD.0000000000004531.
- Heinemann V, von Weikersthal LF, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as firstline treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15(10):1065-1075. doi: 10.1016/S1470-2045(14)70330-4.
- Venook AP, Niedzwiecki D, Lenz HJ, et al. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wildtype advanced or metastatic colorectal cancer: a randomized clinical trial. JAMA. 2017;317(23):2392-2401. doi: 10.1001/jama.2017.7105.
