Role of Immunotherapy in Head and Neck Cancer
Some HNSCCs are characterized by exclusion of immune cells, and the presence of indoleamine-dioxygenase and myeloid-derived suppressor cells indicates a suppressive tumor microenvironment. The PD-1–directed antibodies pembrolizumab and nivolumab and the PD-L1–directed antibodies durvalumab, and atezolizumab have demonstrated single-agent activity in HNSCC, leading to multicenter phase Ib, II, and III trials defining new standards of care in recurrent/ metastatic HNSCC.
cell carcinoma (HNSCC) can be an immunogenic cancer. Expression of the immunosuppressive ligand PD-L1 is identified in approximately 85% of cases, with expression highest in human papillomavirus (HPV )associated cancers, and tumor infiltrating lymphocytes may be present within or surrounding the tumor. Tumor mutational burden can be elevated because of mutation in DNA repair and tumor suppressor genes or in signatures related to expression of the gene-editing protein apolipoprotein B mRNA editing enzyme, catalytic polypeptide-like (APOBEC) 3B, particularly in HPV-associated cancers. Viral antigens are present in HPV-associated oropharynx cancer and Epstein-Barr virus–associated nasopharynx cancer. However, some HNSCCs are characterized by exclusion of immune cells, and the presence of indoleamine 2,3-dioxygenase and myeloid-derived suppressor cells indicates a suppressive tumor microenvironment. The PD-1–directed antibodies pembrolizumab (Keytruda) and nivolumab (Opdivo) and the PD-L1–directed antibodies durvalumab (Imfinzi), and atezolizumab ( Tecentriq) have demonstrated single-agent activity in HNSCC, leading to multicenter phase Ib, II, and III trials defining new standards of care in recurrent/ metastatic HNSCC.
The KEYNOTE-012 and KEYNOTE-055 trials established that pembrolizumab can lead to durable responses in cisplatin-refractory and cisplatin- and cetuximab-refractory HNSCC and indicated that response was more likely when PD-L1 was expressed on tumor cells or tumor-associated immune cells.1 A phase III trial (CheckMate 141) comparing nivolumab with investigator’s choice of standard-of-care (SOC) therapy (weekly cetuximab, docetaxel, or methotrexate) for platinum-refractory disease demonstrated a significant and durable overall survival (OS) advantage for nivolumab.2 KEYNOTE-040 was a phase III trial of pembrolizumab compared with investigator’s choice of SOC therapyoffering a menu of the same agents, although docetaxel was given on an every-3-week schedule, and a higher proportion of patients on the SOC arm received docetaxel. Again PD-1 blockade was superior to SOC.3
The phase III EAGLE trial compared the PD-L1 agent durvalumab, or a combination regimen of durvalumab with the CTLA-4directed antibody tremelimumab, with SOC in a similar population. Here the addition of tremelimumab did not improve response or survival. Median OS for durvalumab monotherapy was 7.6 month compared with 8.3 months for SOC, with crossing of the curves at 9 months and an HR for OS of 0.88 not significantly in favor of durvalumab. A landmark analysis among patients surviving >3 months favors durvalumab, raising a concern about our inability to accurately identify patients at risk for early progression with durvalumab. Thus, to date, the evidence for use of immunotherapy in cisplatin-refractory disease is strongest for PD-1–directed antibodies.4
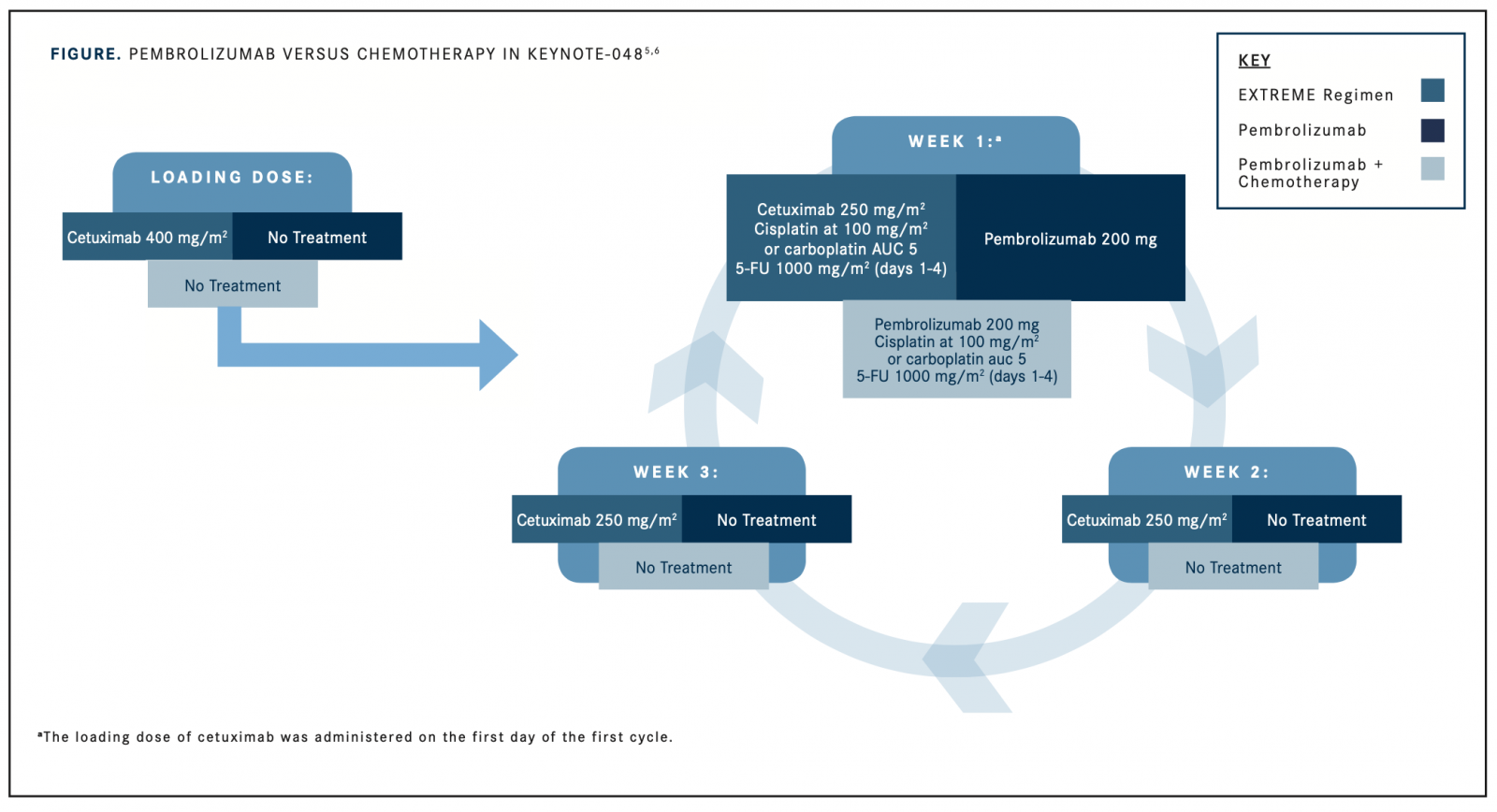
The KEYNOTE-048 trial was a 3-arm, randomized phase III trial evaluating first-line treatment of metastatic/recurrent HNSCC not amenable to curative local therapy, comparing pembrolizumab mono-therapy or the combination of pembrolizumab plus a platinating agent and 5-fluorouracil with standard chemotherapy and cetuximab. This trial assessed the primary end point of OS in both biomarker-enriched and unselected patient populations. Biomarker enrichment employed 22C3-antibody staining for PD-L1 on tumor specimens. A combined positive score was generated by the number of PD-L1positive cells ([tumor cells plus immune cells plus macrophages]/[total tumor cells counted] × 100) and given a score of <1%, >1%, or >20%. For patients expressing PD-L1, pembrolizumab monotherapy was found to be superior to SOC, with a median OS of 14.9 versus 10.7 months among the approximately 45% of patients with high PD-L1 expression and 12.3 versus 10.3 months in those (approximately 85% of all enrolled patients) with any PD-L1 expression.5For the entire population, pembrolizumab was noninferior to the 3-drug regimen, with a median OS of 11.5 versus 10.7 months (HR, 0.83;P= .0199). Median progression-free survival (PFS) was shorter for pembrolizumab, with curves crossing at 7 months, and substantially more patients were progression free at 2 years with pembrolizumab treatment than with SOC chemotherapy and cetuximab (9.5% vs 6.1%). Response proportion was higher for chemotherapy and cetuximab than for pembrolizumab monotherapy, but for patients responding to pembrolizumab, duration of response exceeded 20 months. Grade >3 toxicity was reduced for pembrolizumab alone compared with the combination regimen.6
Pembrolizumab plus chemotherapy led to superior OS compared with chemotherapy plus cetuximab in all analyses: 14.7 versus 11.0 months for highPD-L1 expressers, 13.6 versus 10.4 months for any PD-L1 expression, and 13.0 versus 10.7 months for the entire population. Survival benefits in all analyses hold across 3 years of follow-up. PFS and response rates were comparable to those of the 2 approaches, as was toxicity. Thus, pembrolizumab represents a new SOC for first-line treatment of recurrent or metastatic HNSCC. The addition of chemotherapy to pembrolizumab is safe and improves response proportion and thus is likely to be most used in patients with a higher symptom burden from disease (TABLE).5,6
An interesting observation from all these trials is that the impact of PD-1 inhibition on OS exceeds its impact on PFS. These data imply a lasting modulation of the tumor microenvironment and immune response to HNSCC. Even among patients who experience hyperprogression upon initiation of immune checkpoint inhibition, response to subsequent chemotherapy may be robust, and hyperprogression was not associated with shorter survival in a retrospective review from 4 French centers.
Thus, appropriate management among patients with disease progression on first-line immune checkpoint inhibition will be an important topic of study. Recent data demonstrating activity for the antiangiogenic antibody bevacizumab (Avastin) in recurrent/metastatic HNSCC,7extensive preclinical evidence supporting synergy between antiangiogenic therapies and immune checkpoint inhibition, and favorable early-phase trial data with the combination of lenvatinib (Lenvima) and pembrolizumab8 point to such agents alone, with chemotherapy, or potentially with continued immune checkpoint inhibition as important tools meriting clinical trial in the immunotherapy-failure setting.
The unique biology of HP-associated oropharynx cancer, the observation that PD-L1 expression is more likely and richer in HPV-associated cancers, and the possibility of targeting viral antigens have led to interesting trials employing HPV vaccines in this setting. ADXS11 is an HPV 16 E7 construct presented in the context of listeriolysin O in attenuatedListeria9; ISA101, a synthetic long-peptide HPV 16 vaccine inducing HPV-specific T cells, led to an objective response rate of 33% and an OS of 17.5 months in unresectable HPV-associated cancer10; and a variety of HPV vaccines and cell therapies directed at viral antigens are currently under study.
The Cancer Genome Atlas analyses demonstrated that methylation patterns are markedly different between HPV-associated and non-HPVassociated cancers.11This led to exploration of the demethylating agent 5-azacitidine in the pretreatment window setting in curable-stage HNSCC (NCT02178072). Activity is seen with a single 5-day course of therapy, with dramatic alteration in cell death, immune infiltration, and APOBEC activity confined to HPV-associated cancers. This early experience justifies the study of demethylating therapy in combination with immune checkpoint inhibition both in the window setting and for patients with metastatic or recurrent HNSCC.
These remarkable successes have led to numerous studies incorporating immunotherapy with definitive therapy. Recently completed randomized trials explored addition of pembrolizumab or avelumab (Bavencio) to chemoradiation. EA3161 is a trial for high-risk HPVassociated diseaseie, HPV-associated disease with higher T or N stage or in smokers—suitable for definitive chemoradiation with randomization to postradiation nivolumab or observation (NCT03811015). The possible utility of immune checkpoint inhibitors in the minimal residual disease setting is also employed after surgical salvage in EA3191, a trial of pembrolizumab versus pembrolizumab plus radiation versus radiation plus cisplatin in patients who have undergone salvage resection and have high-risk features. Novel agents including HPV-directed therapeutic vaccines, investigational agents with novel immunoregulatory targets such as B7-H3 and TIM-3, STING agonists, and combinations with targeted therapies and antiangiogenics all hold promise and remain the subject of ongoing studies.
References
- The Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumors.Nature.2012;490:61-70. doi: 10.1038/nature11412.
- Lefebvre C, Bachelot T, Filleron T, et al. Mutational profile of metastatic breast cancers: a retrospective analysis.PLoS Med.2016;13(12):e1002201. doi: 10.1371/journal.pmed.1002201.
- Cohen EEW, Soulières D, Le Tourneau C, et al; KEYNOTE-040 investigators. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study [erratum in Lancet. 2019;393(10167):132. doi:10.1016/S0140-6736(18)33261-6].Lancet.2019;393(10167):156- 167. doi: 10.1016/S0140-6736(18)31999-8.
- Licitra LF, Haddad RI, Even C, et al. EAGLE: a phase 3, randomized, open-label study of durvalumab (D) with or without tremelimumab (T) in patients (pts) with recurrent or metastatic head and neck squamous cell carcinoma (R/M HNSCC).J Clin Oncol.2019;37(suppl 15; abstr 6012). doi: 10.1200/ JCO.2019.37.15_suppl.6012.
- Burtness B, Harrington KJ, Greil R, et al. KEYNOTE‐048: phase III study of first‐line pembrolizumab (P) for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC).Ann Oncol. 2018;29(suppl 8; abstr LBA8_PR). doi: 10.1093/annonc/ mdy424.045.
- Rischin D, Harrington KJ, Greil R, et al. Protocol-specified final analysis of the phase 3 KEYNOTE-048 trial of pembrolizumab (pembro) as first-line therapy for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC).J Clin Oncol. 2019;37(suppl 15; abstr 6000). doi: 10.1200/JCO.2019.37.15_suppl.6000.
- Argiris A, Li S, Savvides P, et al. Phase III randomized trial of chemotherapy with or without bevacizumab in patients with recurrent or metastatic head and neck cancer [published online October 16, 2019].J Clin Oncol. doi: 10.1200/JCO.19.00555.
- Taylor MH, Rasco DW, Brose MS, et al. A phase 1b/2 trial of lenvatinib plus pembrolizumab in patients with squamous cell carcinoma of the head and neck.J Clin Oncol. 2018;36(suppl 15; abstr 6016). doi: 10.1200/JCO.2018.36.15_suppl.6016.
- NCI drug dictionary: live-attenuated Listeria monocytogenes cancer vaccine ADXS11-011. National Cancer Institute website. cancer.gov/publications/dictionaries/cancer-drug/def/live- attenuated-listeria-monocytogenes-cancer-vaccine-adxs11-001. Accessed October 18, 2019.
- Massarelli E, William W, Johnson F, et al. Combining immune checkpoint blockade and tumor-specific vaccine for patients with incurable human papillomavirus 16-related cancer: a phase 2 clinical trial.JAMA Oncol. 2019;5(1):67-73. doi: 10.1001/ jamaoncol.2018.4051.
- Parfenov M, Pedamallu CS, Gehlenborg N, et al; Cancer Genome Atlas Network. Characterization of HPV and host genome interactions in primary head and neck cancers.Proc Natl Acad Sci U S A. 2014;111(43):15544-15549. doi: 10.1073/ pnas.1416074111.