Zenocutuzumab Now FDA-Approved in NRG1+ NSCLC and Pancreatic Cancer
With this approval, zenocutuzumab is the first FDA-approved therapy for patients with NRG1 fusion tumors.
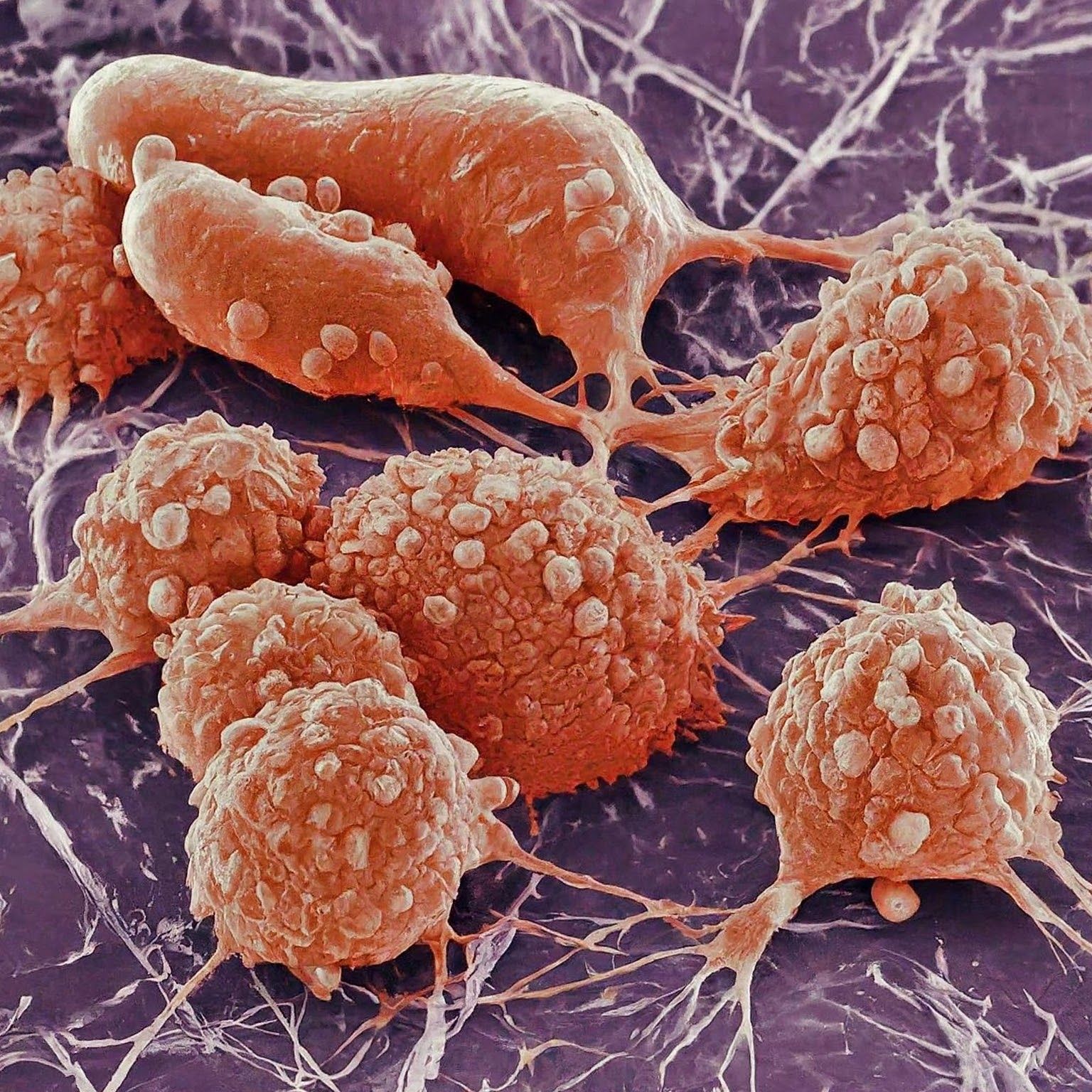
Microscopic image of pancreatic cancer cells - Generated with Google Gemini AI
- The FDA has approved zenocutuzumab (formerly MCLA-128) for the treatment of patients with neuregulin 1 fusion (NRG1+) non–small cell lung cancer (NSCLC) and NRG1+ pancreatic ductal adenocarcinoma (PDAC).
- The approval is supported by the phase 1/2 eNRGy trial (NCT02912949).
- This is the first and only approved targeted therapy for NRG1+ lung and pancreatic cancer.
The FDA has approved zenocutuzumab, making it the first and only approved targeted therapy for patients with NRG1+ NSCLC and PDAC.1
Previously, the biologics license application of zenocutuzumab was granted priority review in May 2024, and the agent was granted breakthrough therapy designation in July 2023.
The phase 1/2 eNRGy trial investigating the safety and antitumor activity of zenocutuzumab supports this approval. The major efficacy outcome measures were confirmed overall response rate (ORR) and duration of response (DOR), determined by blinded independent central review according to RECIST v1.1. For patients with NSCLC, the ORR was 33% (95% CI, 22%-46%). The median DOR was 7.4 months in these patients (95% CI, 4.0 -16.6). For those with pancreatic adenocarcinoma, the ORR was 40% (95% CI, 23%-59%) and the DOR was 3.7 months to 16.6 months.
For safety, the most common adverse events (≥10%) included diarrhea, musculoskeletal pain, fatigue, nausea, infusion-related reactions, dyspnea, rash, constipation, vomiting, abdominal pain, and edema. Grade 3 or 4 laboratory abnormalities (≥10%) most commonly seen were increased gamma-glutamyl transferase, decreased hemoglobin, decreased sodium, and decreased platelets.
Data from this trial were also presented at the American Society of Clinical Oncology (ASCO) Annual Meeting in 2021 and 2022, as well as at the European Society for Medical Oncology (ESMO) 2023 Congress.
According to data presented at ASCO, zenocutuzumab led to an objective response rate (ORR) of 34% (95% CI, 24%-46%) by investigator assessment and RECIST v1.1 criteria at a median follow-up of 6.3 months in 79 patients with previously treated advanced NRG1+ cancers.2 Additionally, the median time to response (TTR) was 1.8 months, and the median duration of response (DOR) was 9.1 months (95% CI, 7.4-not reached).
“Zenocutuzumab is highly effective in pretreated NRG1 fusion-positive pancreatic cancer, with rapid and durable responses,” said Alison M. Schram, MD, lead study author and medical oncologist at Memorial Sloan Kettering Cancer Center in New York, New York, during a presentation of the data. “There is activity across multiple NRG1 fusion-positive cancer types and an extremely well-tolerated safety profile.”
Data presented at ESMO showed that zenocutuzumab delivered an ORR of 37.2% (95% CI, 26.5%-48.9%) and a clinical benefit rate (CBR) of 61.5% (95% CI, 49.8%-72.3%) in patients with NRG1+ NSCLC.
About the Phase 1/2 eNRGy Trial
eNRGy is an open-label, multicenter, dose-escalation study of zenocutuzumab in patients with solid tumors with a NRG1 fusion.3 The primary end points are ORR and DOR. Secondary end points include CBR, TTR, safety, tolerability, pharmacokinetics, overall survival, and progression-free survival.
Patients with at least 1 measurable lesion, an ECOG performance status of 0 to 2, an estimated life expectancy of at least 12 weeks, resolved toxicities from prior therapies, and adequate laboratory levels were eligible for participation in the trial. Patients who were pregnant or lactating, had a known HIV or hepatitis infection, had leptomeningeal metastases, or had a previous or concurrent malignancy were not eligible for enrollment in the study.
The recommended phase 2 dose is 750 mg, which was administered every 2 weeks in patients with both NSCLC and PDAC.







