Tweet Chat Recap: Sequencing Strategies for a Post-Docetaxel Patient with Metastatic Castration-Resistant Prostate Cancer
In an interview with Targeted Oncology, following a tweet chat on prostate cancer, Tian Zhang, MD, discussed the key takeaways from the tweet chat discussion and highlighted both the role of molecular testing and the impact of the recent FDA approvals in prostate cancer.
Tian Zhang, MD

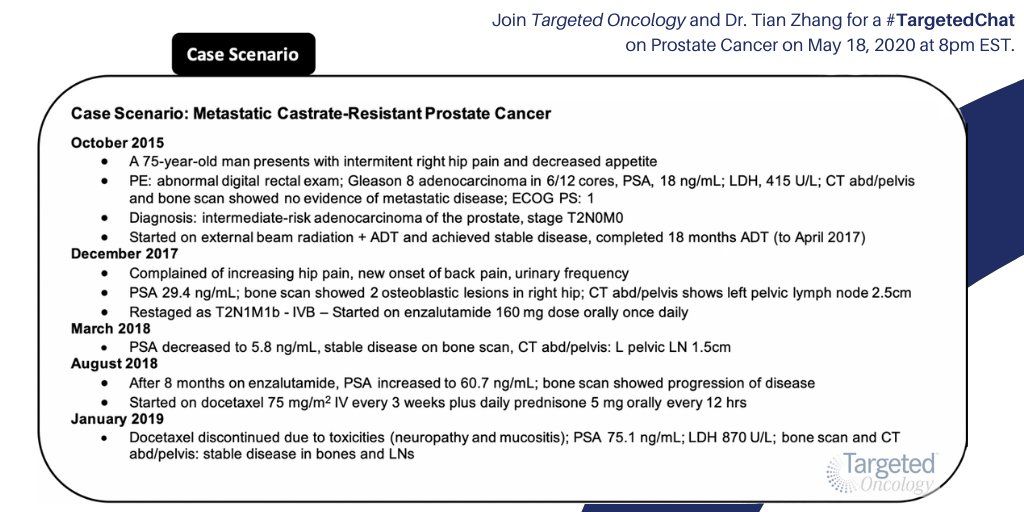
Targeted Oncology was joined by Tian Zhang, MD, of the Duke Cancer Institute, for the discussion of a 75-year-old man with metastatic castration-resistant prostate cancer (mCRPC) in a recent tweet chat. In this case scenario, the patient had already received docetaxel treatment, which was discontinued due to toxicities. According to Zhang, this is a common scenario in the clinic.
In a Twitter poll ahead of the discussion, Targeted Oncology followers shared their thoughts on what might be the next best line of therapy for this patient. Overall, 45.2% voted for treatment with cabazitaxel (Jetvana), while 25.8% voted for abiraterone acetate (Zytiga) plus prednisone and 25.8% for radium-223 (Xofigo). Only 3.2% had opted for carboplatin plus docetaxel as the next best line for this patient.
The decision to use cabazitaxel in the next line for this patient is supported by data from the phase II CARD trial. In this study, 255 patients with mCRPC previously treated with docetaxel were randomized to receive either cabazitaxel or abiraterone or enzalutamide (Xtandi). Findings demonstrated a median radiographic progression-free survival (PFS) of 8.0 months with cabazitaxel versus 3.7 months with either abiraterone or enzalutamide (HR, 0.54; 95% CI, 0.40-0.73; P <.001). According to a pre-planned analysis of the CARD trial, which was recently presented in the American Urological Association (AUA) Virtual Experience platform for the 2020 AUA Annual Meeting, better patient-reported outcomes were also observed in the cabazitaxel arm versus either abiraterone or enzalutamide. The agent also demonstrated a manageable safety profile with less cardiac disorders than seen in the control arm.
In the tweet chat, Zhang noted the grade >3 toxicities observed in the CARD trial, highlighting the observations of febrile neutropenia, which occurred in 3.2% of patients in the cabazitaxel arm who were given prophylactic granulocyte-colony stimulating factor (G-CSF) in each cycle.
While the majority appeared to agree that cabazitaxel would be the next best line of therapy, patients may prefer not to use an immune-suppressing chemotherapy agent during the coronavirus disease 2019 (COVID-19) pandemic.
Prior to the chat, the FDA had approved rucaparib (Rubraca) as treatment of patients a deleterious BRCA mutation (germline and/or somatic)-associated mCRPC who have been treated with androgen receptor (AR)-directed therapy and a taxane-based chemotherapy. Following the chat, the FDA also approved olaparib (Lynparza), another PARP inhibitor, for the treatment of patients with mCRPC who have a deleterious or suspected deleterious germline or somatic homologous recombination repair gene mutation and had progressed on prior treatment with a new hormonal agent.
To conclude the tweet chat, Zhang highlighted the importance of molecular testing in prostate cancer. Its role continues to evolve, and the importance of both tissue-based testing and molecular testing in patients with prostate cancer is underscored by these 2 approvals.
Zhang spoke to both the pros and cons of liquid biopsy and tissue biopsy. With liquid biopsy, results can be accessed in “more real-time” and could be more indicative of driver oncogenic changes, she said. Liquid biopsies can be used multiple times after the disease progresses, but the tests may not cover all of the genes that can be found in a tissue-based test. Zhang said that tissue biopsies remain the “gold standard of genomic sequencing” and include panels of actionable mutations. However, she noted that archival specimens may not be retrievable or representative of current driver mutations in a patient, and tumors may not be “biopsy-able” for patients with bone predominant disease as the bone may have minimal tumor to test.
In an interview with Targeted Oncology, following the tweet chat, Zhang discussed the key takeaways from the tweet chat discussion and highlighted both the role of molecular testing and the impact of the recent FDA approvals in prostate cancer.
TARGETED ONCOLOGY: What were your first impressions of this patient case?
Zhang: It was a 75-year-old man who had mCRPC progressing after 1 line of AR-targeted therapy and he also couldn’t tolerate the toxicities of docetaxel after about 3 cycles. We were thinking about next line sequencing and management for him. It is a situation that we are faced with not uncommonly. It is pretty often that we have this type of scenario in our clinics and the question of what to do next or what treatment to sequence is 1 that arises very often.
TARGETED ONCOLOGY: The majority in our poll had opted for cabazitaxel as the next best line of therapy for this patient. Do you agree with this choice, and why or why not?
Zhang: Cabazitaxel post-docetaxel is certainly a good treatment option. We have data from the CARD trial that shows in this population post-docetaxel that randomized patients to either cabazitaxel or the other AR-targeted therapy, either enzalutamide or abiraterone, cabazitaxel improved benefit in terms of better PFS and responses. I do think, although it was a phase II trial, it was a prospective evidence for what we are seeing clinically and through retrospective studies that abiraterone after enzalutamide or enzalutamide after abiraterone does not get us the clinical benefit we need with a second AR-targeted strategy. It did allow patients who were coming off of docetaxel for toxicity. This patient had some high-risk features with his elevated LDH levels, so I do think in that population, treatment with cabazitaxel is warranted. I do agree that in a physically fit and well 75-year-old that cabazitaxel is a good option.
The 1 caveat, of course, which we mentioned in the tweet chat, was during COVID-19, risk depending on geographic differences may be higher or lower, but our elderly population certainly has higher mortality and complications from COVID-19, so we would take that into consideration when starting a chemotherapy agent like cabazitaxel. There is febrile neutropenia risk, as well as regular neutropenia risk, so having that candid discussion with a patient about potential risks and benefits would be warranted.
TARGETED ONCOLOGY: Is there anything else to note about the CARD trial for this particular patient case?
Zhang: This is the same patient population, and this patient would have been a candidate for the CARD trial. Cabazitaxel has activity and is better in terms of PFS and controlling disease for longer than either abiraterone or enzalutamide given sequentially. I think that it provides a lot of support for sequencing the chemotherapy after docetaxel.
TARGETED ONCOLOGY: Besides the increased concerns during the COVID-19 pandemic, what other toxicities should physicians be mindful of when treating with cabazitaxel?
Zhang: It has a different toxicity profile than docetaxel for sure. It does have some more diarrhea, for example, as well as the febrile neutropenia risk. The risk is less of the peripheral neuropathy, which is good for our patients who have chronic baseline neuropathy. I think that when we look at these patients, we just have to compare and contrast the agents in terms of what the toxicities are and have them expect those [toxicities]. We are able to manage them better if they can catch them earlier.
TARGETED ONCOLOGY: During the chat, you mentioned that chemotherapy can “reset the tumor.” Could you elaborate more on this event and how it plays a role in switching from docetaxel to cabazitaxel?
Zhang: Sometimes we see patients when we use a cytotoxic agent and eliminate the AR-resistant clones that are growing. If we are able to target those and try to eliminate all the cancer clones, then sometimes in the post-chemotherapy timeframe, we are “resetting” the clock, and they might be more sensitive to another line of AR-targeted treatment. I think we all have clinical experiences where we have patients like that, where we sequence multiple lines of therapies and try another AR-targeted strategy. However, it is hard to tell. I think using biomarkers and molecular sequencing can sometimes help us determine which patients will actually benefit from either AR-targeted strategies or even other agents. We just had the approval of rucaparib and then olaparib was approved as well. Eventually, these PARP inhibitors can be layered into our sequencing strategies as well.
TARGETED ONCOLOGY: How do these approvals underscore the importance of molecular testing in prostate cancer?
Zhang: The FDA approved rucaparib for BRCA1/2-mutated patients who are post-taxane chemotherapy and post-abiraterone or post-enzalutamide. That is a somewhat limited population. The olaparib approval is for any homologous recombination gene mutation, and that is a bucket of maybe about 10 genes. It allows for post-abiraterone or post-enzalutamide, and it does not require prior chemotherapy, so the label there is a little broader. In that context, I think it is important to find the genetic mutations when they are present. We think that in mCRPC, this exists in about 10% to 15% of patients. If we do not look, we will not find it. We have to do molecular sequencing.
We have incorporated a lot of germline testing in our clinical pathway and workup for metastatic prostate cancer, but also somatic testing, and these mutations can sometimes arise because of the treatments we have applied. Based on treatment pressure, some of the resistance mutations can occur. I think obtaining those types of molecular testing would be important, especially for our bone-predominant metastases; those patients may not have targetable lesions to biopsy, and if that is the case, sometimes we are left with sending circulating tumor DNA (ctDNA) tests as a way to capture that. If it is present, I certainly think that an approved PARP inhibitor as the next line of treatment would be appropriate.
TARGETED ONCOLOGY: During the discussion, you highlighted the pros and cons of liquid biopsy versus tissue-based testing. Is there anything else you would like to add in?
Zhang: There are pros and cons of each, and sometimes it is not prudent to get sequential biopsies, especially for our patients with prostate cancer who often have bone metastases. I had a patient who has gone through so many lines of treatment and we signed him up for several of our own trials. One of the trials required a bone biopsy, which he happily did, but at the end of the day, there was not enough tumor tissue, and once the bone is decalcified and processed, unfortunately there is very little there. Sometimes even for the pathologists in the clinical read, there is no tumor available to give a diagnosis. If that is the case, there is limited utility of sequencing those tissues. That is the biggest limitation I have seen of tissue-based testing, so ctDNA help us avoid subjecting a patient to a biopsy. However, tissue is still the golden standard, so we get them when we can, and when we can’t, ctDNA is a good substitute.
TARGETED ONCOLOGY: During the discussion, you mentioned some upcoming data we will see at the 2020 American Society of Clinical Oncology (ASCO) Virtual Annual Meeting that might be useful in this particular patient case. Would you like to elaborate more on this?
Zhang: For this particular instance where we are talking about a post-docetaxel treated patient, the study that stood out to me is the TheraP trial where the Australian and New Zealand group took patients in this population and treated them with either the PSMA targeted lutetium versus cabazitaxel. We will see the data next week, but it sounded pretty promising that the PSMA-targeting strategy with lutetium had clinical activity in this population. We have participated in the phase III VISION study of the PSMA-targeted agent, lutetium. That is a little farther from clinical reports and the data coming out, but so far, I have only seen promising data, so I am excited to see that trial being highlighted at ASCO.
TARGETED ONCOLOGY: What is your key takeaway from our tweet chat?
Zhang: In general, I think sequencing is a very common question that we face in the clinics. With the new approvals of rucaparib and olaparib, it is very important to phase in molecular testing for these patients. When the time is right, we can use a chemotherapy agent, and if patients progress or cannot tolerate docetaxel, then it does seem that cabazitaxel is a good alternative.
The only piece that we did not talk about was that there are 2 doses of cabazitaxel approved, and the efficacy seems to be similar between the 20 mg/m2 and 25 mg/m2 doses. If in doubt and when trying to limit toxicities, oncologists choose to sue the 20 mg/m2 dose every 3 weeks to try to limit toxicities.