Tweet Chat Recap: Hamid Evaluates a Basal Cell Carcinoma Case
In an interview with Targeted Oncology following the tweet chat, Omid A. Hamid, MD, discussed the key takeaways from the discussion, including the ways he would treat the patient discussed in the case.

Targeted Oncology was joined on Twitter by Omid A. Hamid, MD, chief of Translational Research and Immunotherapy, director, Melanoma Therapeutics, The Angeles Clinic and Research Institute, for the discussion of an 88-year-old man with infiltrative Basal cell carcinoma (BCC).
In a Twitter poll ahead of the discussion, Targeted Oncology followers shared their thoughts on whether or not they would give cemiplimab (Libtayo) as frontline therapy for this patient with 66.7% voting yes while the other 33.3% voted no.

Hamid however, added his own thoughts, stating that “the approval of cemiplimab is in patients not amenable to local treatment measures [radiation or surgery] and not candidates for hedgehog inhibitors [HHI]. There are multiple neoadjuvant trials to understand the role for early immunotherapy in improving outcomes, [and] remember a switch to HHI in patients with stable disease [SD] in 9 months is part of the label.”
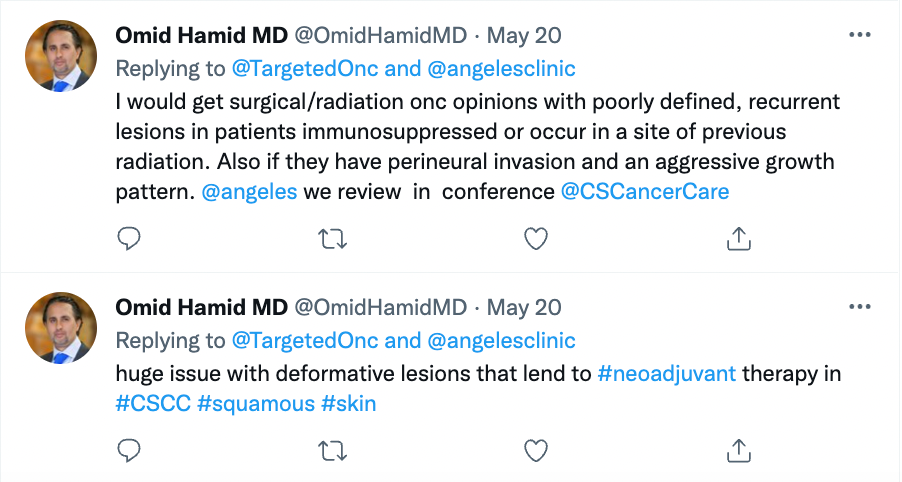
To stratify BCC to determine treatment options, given the patient’s high risk for recurrence, Hamid states that mask areas, including across the center of the face, eyelids, eyebrows, periorbital, postauricular area, temple, ears, nose, and lips, are considered to be high-risk areas. For the limited number of individuals with BCC who end up reporting the occurrence of locoregional or distant metastases, which result in an increased risk for mortality and the need for alternative approaches to therapy, systemic therapy would be considered.
Then, high-risk lesions, which are usually larger than 2cm on the trunk and/or extremities are usually greater than 2 cm in size, or locally advanced lesions and in cheeks, forehead, scalp, neck, and pretibial area which are greater than 1 cm in these sites, would be candidates for surgery or radiation.
Some of the treatment options available include resection, radiation, or even neoadjuvant evaluation and treatment. Along with this, Hamid adds that this patient would be a good candidate to enroll in a clinical trial.
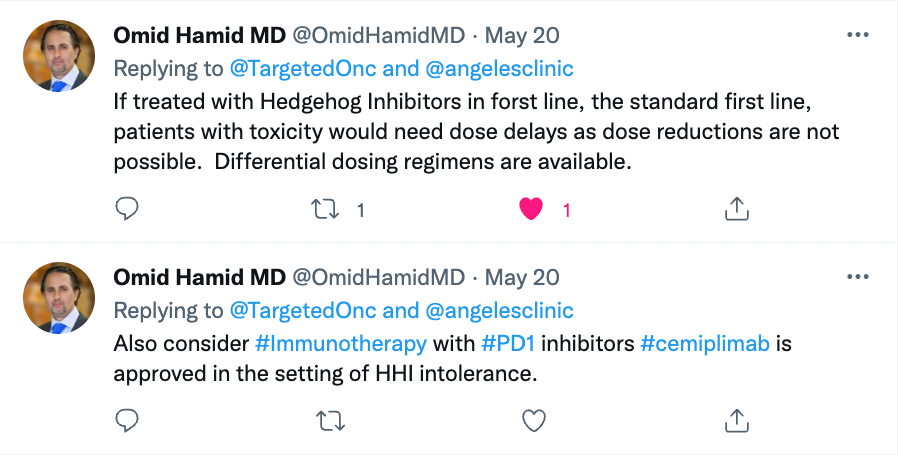
Hamid does not believe that dose reduction would be possible for patients given HHIs as, “[they] have toxicities that are difficult to control. Many regimens with breaks are appropriate but they cannot be dosed in a dose reduction or in alternation day fashion given pharmacokinetics. Consider breaks when toxicity occurs.”
Further, patients where hedgehog inhibitors are contraindicated due to toxicity, Hamid would use cemiplimab as first-line therapy as he is a proponent of immunotherapy as a single agent or combination as an expanding first-line option.
There are still many unmet needs which need to be filled in this space, including understanding surveillance regimen, sequencing therapy, combination therapy and its benefits, the role of newer medications such as CTLA4/PD1 combinations, oncolytics, and local therapy, adjuvant clinical trials, and molecular indicators of response and recurrence.
In an interview with Targeted OncologyTM following the tweet chat, Hamid, discussed the key takeaways from the discussion, including the ways he would treat the patient discussed in the case.
Targeted Oncology: What did you think of those poll results? Do you agree with the overall response?
Hamid: I agree with the overall response. Hedgehog inhibitors, while they make a lot of sense and they targeted the hedgehog pathway very well and mutations in smooth Indian patch, what we found is a difficulty and tolerability and for an extended period of time, given the severe disfigurement, morbidity and mortality of locally advanced or metastatic Basal cell carcinoma, we've been forced to utilize these drugs. They come with significant side effects, a frequent dose hold, and we've been throwing our hands up in the air. What you are seeing now is a therapy that makes sense. Basal cell carcinoma has the highest mutational burden of any solid tumor and therefore it indicates a high chance of response to immunotherapy with immunotherapy showing greater duration of response and persistence than targeted therapy. And our familiarity with immunotherapy through PD one inhibitors and other solid tumors. It just makes sense.
How do you stratify Basal cell carcinoma to determine treatment options?
I look at those patients who are at a high risk for recurrence and discuss with them clinical trials that are available. I failed to mention, and I should mention that there are adjuvant clinical trials. In Basal cell carcinoma, there’s one being run now by Regeneron, for high-risk lesions, those with nodal involvement perineural involvement. And those will help us to understand the role of adjuvant therapy. This is a paradigm that’s being utilized in other solid tumors where we’ve seen responses to immunotherapy, including renal cell carcinoma and melanoma. So, it just makes sense. Those who have recurred multiple times post radiation and surgery, that are the ones that even if they’re amenable to surgery, are going to recur again. So those are ones where you would initiate an earlier systemic therapeutic option.
Considering that the patient we discussed has a high risk for recurrence, what would be some of the available treatment options?
Either neoadjuvant approach has been looked at in clinical trials with hedgehog pathway inhibitors, and we’ve seen a high response rate in disease control. I think that's one way you think about decreasing the morbidity of surgery. So, neoadjuvant approaches, whether they be with hedgehog pathway inhibitors or immunotherapy with checkpoint inhibitors, look to decrease the morbidity of a surgical procedure or radiation. They're completely indicated in places where surgery would be reformative. They're completely indicated in places where you don't think that you can give radiation or surgery; those are usually near the area of the eye, where they may lead to difficulties with vision etc. And they make sense in a scientific manner, which is to say that if I had a patient like this, I'd look for a clinical protocol where the disease is biopsied, treatment is given, and the response is noted. And we can look through the pre and post biopsies, blood and other looking for predictive or prognostic markers that may help us to be able to fashion you know, bespoke therapies for our locally advanced and metastatic patients, I think the low incidence for these patients with Basal the low incidence is important to understand going forward and that you have every opportunity to get more for these patients.
During the tweet chat, you discussed immunotherapy being an option for these patients. After this, do you think it is okay if the patient undergoes radiotherapy?
To clarify, Basal cell carcinomas and Basal cell carcinomas have high tumor mutational burden, so they are keys to treatment with immunotherapy. Radiation has been shown to be tolerable with immunotherapies. In this situation, if you're not getting optimal benefit, you can bring in radiation to see if there is something like a synergy of response and we've seen that in our patients with Basal cell carcinoma.
Can you expand on the unmet needs in this space? What ongoing efforts are there to improve care for these patients?
We don't have a lot of information in regards to predictive markers. We don't have a lot of information in regards to prognostic markers. We don't have enough adjuvant and new adjuvant trials to help us we've seen that these nonmelanoma skin cancers have high tumor mutational burden and I utilize my thought process for Basal and squamous cell carcinoma is the same, that they can be used rate patients for combinatorial therapies to increase response rate and increased durability of response.
What would you consider to be the main takeaways of the tweet chat?
I think it's a great option to utilize a platform to bring these patients in. When we did the trials with hedgehog inhibitors, patients who had never seen a medical oncologist came out of the woodwork. These were patients who received significant disfiguring surgeries and radiation in a multitude fashion over and over again. They were getting disfigured surgeries, or radiation was failing them, and they have now come in, not to the loss of the utilization of radiation and surgery, but into a pathway that has multidisciplinary care available for these patients.
Atlas Examines Tolerability of Hedgehog Pathway Inhibitors and Transition to IO in mBCC
October 16th 2024During a Case-Based Roundtable® event, Jennifer L. Atlas, MD, discussed treatment for a patient with basal cell carcinoma who reported challenging adverse events with hedgehog pathway inhibitor.
Read More
Tawbi Discusses the Role of Brain Metastases and PD-L1 Status in Melanoma
September 11th 2024During a Case-Based Roundtable® event, Hussein A. Tawbi, MD, PhD, and participants look at benefits of nivolumab combinations for brain metastases and PD-L1 positivity in the metastatic melanoma population in the second article of a 2-part series.
Read More








