Targeted Biopsies Detect More High-Risk Prostate Cancers Than Standard Biopsies
In many cases, prostate cancer grows slowly and causes few symptoms; thus, many men remain unaware that they have the disease.
1Unlike many solid tumors, which are identified through diagnostic imaging, prostate cancer screening relies on prostate-specific antigen (PSA) testing and a digital rectal examination. When a PSA test shows elevated PSA levels (typically >4.0 ng/mL) and a digital rectal examination indicates an abnormality, patients often undergo a standard extended-sextant biopsy (ie, standard biopsy) for suspected prostate cancer.2
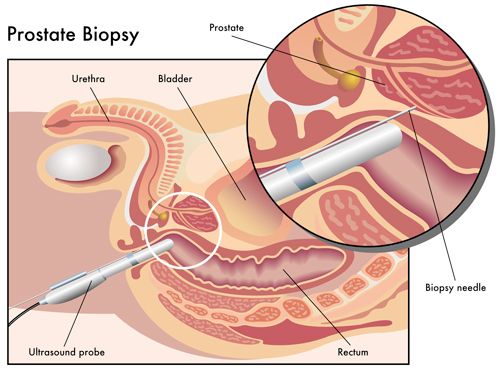
Standard biopsy involves taking between 6 and 14 random samples from the prostate.2Without the use of imaging to guide sampling, this process has been called “a shot in the dark.”3Up to 20% of prostate cancers are missed using this technique, and another 20% are more aggressive than initially detected.2
A new study published in JAMA, however, showed that prostate cancer detection can be significantly improved when biopsies are guided with imaging that fuses magnetic resonance imaging (MRI) with ultrasonography (ie, targeted biopsies).4
In many cases, prostate cancer grows slowly and causes few symptoms; thus, many men remain unaware that they have the disease.
The study investigators, led by Mohummad Minhaj Siddiqui, MD, assistant professor of surgery at the University of Maryland School of Medicine and director of urologic robotic surgery at the University of Maryland Marlene and Stewart Greenebaum Cancer Center, Baltimore, MD, reported that targeted biopsies identified 30% more high-risk prostate cancers and 17% fewer low-grade prostate cancers compared with standard biopsy.
"With fusion technology, we now have a tool to help us differentiate high-risk cancers from low-risk ones that may require minimal or no treatment," said Siddiqui in a University of Maryland Medical Center press release.5“There is a concern that we over-diagnose and over-treat low-risk cancers that are unlikely to be terminal, and this technology enables us to make a more reliable diagnosis than the current standard practice,” he added.
MRI/ultrasound fusion electronically superimposes images from multiparametric MRI onto transrectal ultrasound images in real time, enabling urologists to progress from blind biopsies to those that are mapped, targeted, and tracked.6 Previous studies have shown that targeted biopsies in combination with standard biopsies is a superior approach to standard biopsy alone, but these studies have also led to questions about the necessity of also performing the standard biopsy when a targeted biopsy was already being undertaken.4,6
Siddiqui and colleagues’ prospective cohort study sought to shed light on these questions by comparing targeted biopsies with standard biopsies in identifying intermediate- to high-risk prostate cancers in 1003 men undergoing concurrent targeted and standard biopsies over a 7-year period (2007-2014) at the National Cancer Institute. All patients had elevated PSA levels, an abnormal digital rectal examination, or both, with most patients having previously received negative biopsy results.
In the study, targeted biopsies diagnosed 461 cases of prostate cancer and standard biopsy diagnosed 469 cases, with exact agreement between the two modalities occurring in 690 cases (69%). Targeted biopsy identified 30% more high-risk cancers compared with standard biopsy (173 vs 122 cases;P<.001) and 17% fewer low-risk cancers (213 vs 258 cases;P<.001). Adding standard biopsy cores to the targeted approach identified another 103 cases of prostate cancer (22%), most of which where low risk (83% low risk, 12% intermediate risk, and 5% high risk).
In addition, the predictive ability of targeted biopsy to differentiate between low-, intermediate-, and high-risk disease in 170 men with whole-gland pathology after prostatectomy was greater than that of standard biopsy or of the 2 approaches combined (area under the curve, 0.73, 0.59, and 0.67, respectively;P<.05 for all comparisons).
“While these findings could translate into substantial benefit to patients, this study is preliminary with regard to clinical endpoints such as recurrence of disease and prostate cancer-specific mortality," said Siddiqui, noting that randomized clinical trials are needed to determine the impact of targeted biopsies on clinical outcomes.
Siddiqui is taking steps to undertake such a clinical trial. He plans to assess the ability of MRI/ultrasound fusion to identify and biopsy suspicious areas within the prostate and use the findings to guide treatment.4
In low-risk cases, he will use this technology to perform more reliable active surveillance, enabling fewer biopsies to be taken. In intermediate-risk disease (ie, disease that requires treatment but is not widespread), he will use focal brachytherapy to irradiate only the tumor and protect the surrounding tissue, sparing these patients from experiencing the side effects associated with prostatectomy or whole prostate gland irradiation. In high-risk cases, he plans to use MRI/ultrasound fusion to guide more aggressive options, such as robotic surgery. No announcement has yet been made as to when Siddiqui’s trial will start enrolling patients.
References
- American Cancer Society. What are the key statistics about prostate cancer? http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-key-statistics. Last Revised January 5, 2015. Accessed January 25, 2015.
- Prostate mapping. Prostate biopsy. http://www.prostatemapping.com/prostate-biopsy.aspx. Accessed January 25, 2015.
- McCallum J. Chapter 16...in which the author ponders the lessons of prostate cancer, offers tentative advice, and breaks bread with his prostatectomy pal.The Prostate Monologues: What Every Man Can Learn From My Humble, Confusing, and Sometimes Comical Battle With Prostate Cancer. New York, NY: Rodale Books; 2013:181-198.
- Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/Ultrasound Fusion-Guided Biopsy With Ultrasound-Guided Biopsy for the Diagnosis of Prostate Cancer.JAMA. 2015;313(4):390-397.
- New research in JAMA: targeted MRI/ultrasound fusion technique more effective than standard biopsy to detect high-risk prostate cancer [news release]. Baltimore, MD: University of Maryland Medical Center; January 27, 2015. http://umm.edu/news-and-events/news-releases/2015/mri-ultrasound-fusion-technique-more-effective. Accessed January 29, 2015.
- Marks L, Young S, Natarajan S. MRI-ultrasound fusion for guidance of targeted prostate biopsy.Curr Opin Urol. 2013;23(1):43-50.