Superior Outcomes Seen With Fixed-Duration Ibrutinib/Venetoclax in CLL
In the phase 3 GLOW study, ibrutinib plus venetoclax significantly improved progression-free survival and other outcomes in patients with chronic lymphocytic leukemia, across most genomic subgroups.
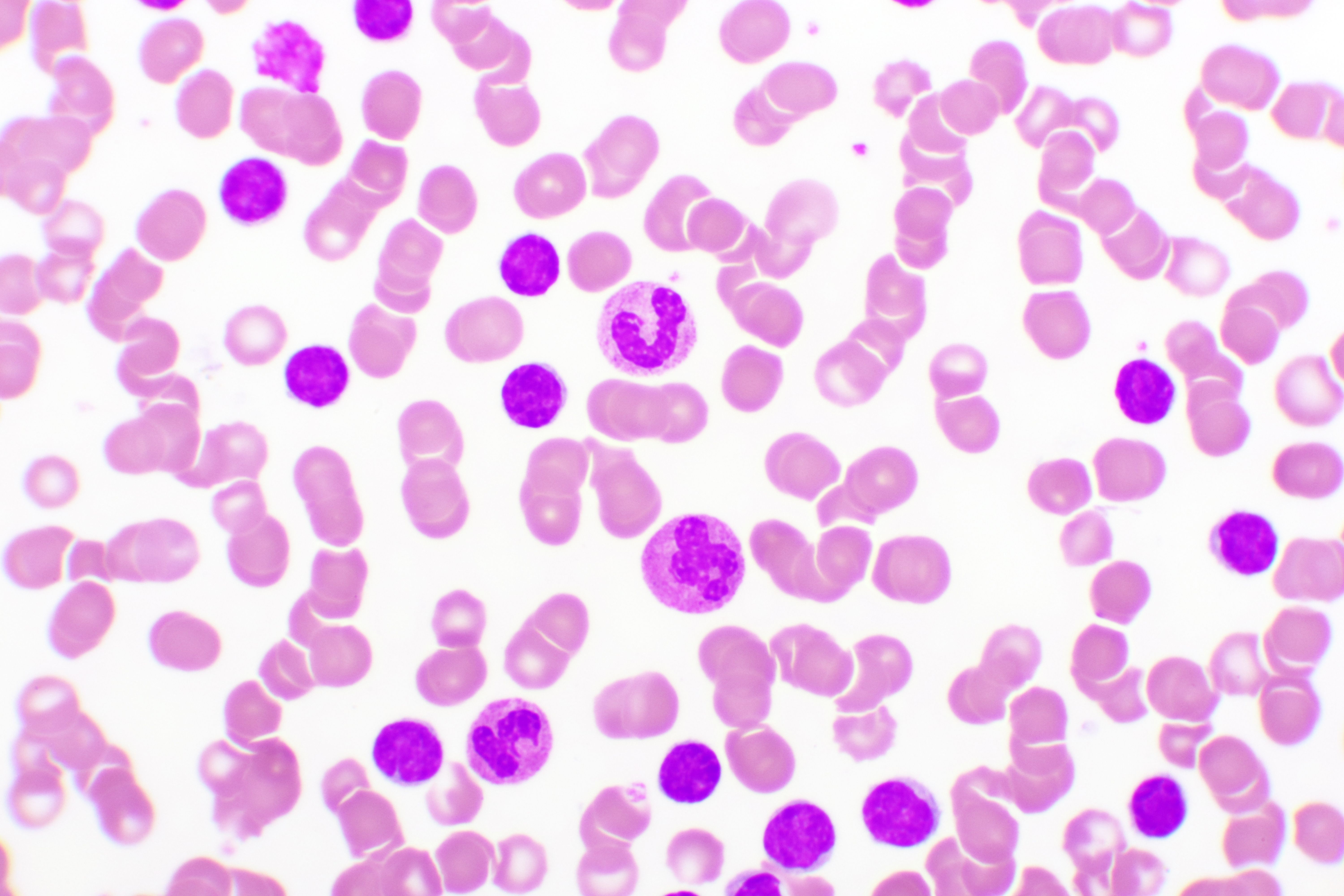
chronic lymphocytic leukemia © jarun011 - stock.adobe.com
Patients treated with fixed-duration ibrutinib (Imbruvica) plus venetoclax (Venclexta) achieved higher undetectable minimal residual disease (uMRD), progression-free survival (PFS), and overall survival (OS) rates compared with chlorambucil plus obinutuzumab (Gazyva) across most genomic subgroups of chronic lymphocytic leukemia (CLL).1
Findings come from the phase 3 GLOW study (NCT03462719) in which data were presented at the 11th Annual Meeting of the Society of Hematologic Oncology (SOHO 2023). Patients treated with ibrutinib and venetoclax achieved a higher uMRD rate at 3 months (54.7%) after the end of treatment compared with patients treated with obinutuzumab and chlorambucil (39.0%), except patients with trisomy-12, IGLL5 mutation, and mutated immunoglobulin heavy-chain variable (mIGHV).
Additionally, a median follow-up of 46 months, PFS rates were significantly improved among patients treated with ibrutinib and venetoclax vs obinutuzumab and chlorambucil (HR, 0.214; 95% CI, 0.138-0.334; P <.0001).
Investigators on the GLOW study sought to evaluate the impact of baseline genomic alterations on response, uMRD, and PFS among patients treated with ibrutinib with venetoclax and chlorambucil with obinutuzumab. The randomized, open-label, phase 3 trial enrolled patients aged ≥ 65 or 18 to 64 years with cumulative illness rating scale score of > 6 or creatinine clearance of < 70 mL/min, an ECOG performance status of 0, 1, or 2, and measurable nodal disease.2
Patients in the study were randomized 1:1 and stratified by del(11q) and IGHV status. In the experimental arm, patients were treated with ibrutinib 420 mg daily for 3 cycles and venetoclax from 20 mg to 400 mg over 5 weeks beginning at cycle 4. This combination will be given for 12 cycles. In the active comparator arm, patients were given obinutuzumab 1000 mg intravenously on days 1, 8 and 15 of cycle 1, and on day 1 of cycles 2 to 6 and chlorambucil 0.5 mg/kg body weight, on days 1 and 15 of cycles 1 to 6.
Baseline genomic alterations were balanced across treatment arms.1 Incidences of baseline genomic alterations based on Döhner hierarchy were 18.5% for del(11q), 22.3% for +12, and 44.1% for del(13q). Unmutated IGHV (uIGHV) was observed in 58.8% of patients vs mIGHV in 31.8%. Gene mutations most frequently seen included NOTCH1-ICD, SF3B1, ATM, XPO1, and RPS15.
According to findings, significantly higher rates of complete responses were observed among patients with del(11q), normal karyotype, del(13q), NOTCH1-ICD, SF3B1, ATM, PCLO, mIGHV, and uIGHV in the ibrutinib/venetoclax arm (42.5%) vs obinutuzumab/chlorambucil arm (12.4%).
For del(13q), patients treated with the experimental combination also had higher uMRD rates (presence, 66.7% v absence, 49.3% and uIGHV, 59.7% v mIGHV 40.6%), and lower rates for +12 (42.1% v absence 57.5%) and NOTCH1-ICD (mutated 38.9% v wild-type 58.0%), however differences were not statistically significant.
uMRD rates at 3 months after end of treatment + 3 in peripheral blood also trended higher for +12 (50.0% vs absence 36.1%), and lower for SF3B1 (mutated, 26.3% vs wild-type, 41.9%) and ATM (mutated, 28.6% vs wildtype, 40.7%). Again, differences were not statistically significant. Further, patients with uIGHV had significantly lower uMRD vs patients with mIGHV.
In the experimental arm, PFS was improved for patients in the experimental arm vs active comparator arm across all chromosomal and genomic subgroups. This excluded +12 (HR, 0.58), mutated NOTCH1-ICD (HR, 0.42), and IGLL5 (HR, 0.15), which each trended in favor of ibrutinib and venetoclax, but were not statistically significant.
Additionally, patients treated with ibrutinib and venetoclax had improved OS rates vs with obinutuzumab and chlorambucil (HR, 0.487; 95% CI, 0.262-0.907; nominal P =.0205).
Overall, findings showed that with median follow-up of nearly 4 years, uIGHV status and presence of +12 correlated with shorter PFS rates in the GLOW study among patients treated with fixed-duration ibrutinib and venetoclax.
REFERENCES:
Kater A, Hodkinson B, Moreno C, et al. Genomic alterations and outcomes with fixed-duration ibrutinib + venetoclax: results from the phase 3 GLOW study in patients with previously untreated chronic lymphocytic leukemia.Presented at: 11th Annual Meeting of the Society of Hematologic Oncology (SOHO 2023). September 6-9, 2023. Houston, TX.CLL-584
A study of the combination of ibrutinib plus venetoclax versus chlorambucil plus obinutuzumab for the first-line treatment of participants with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) (GLOW). ClinicalTrials.gov. Updated August 30, 2023. Accessed September 13, 2023. https://tinyurl.com/24u34an4







