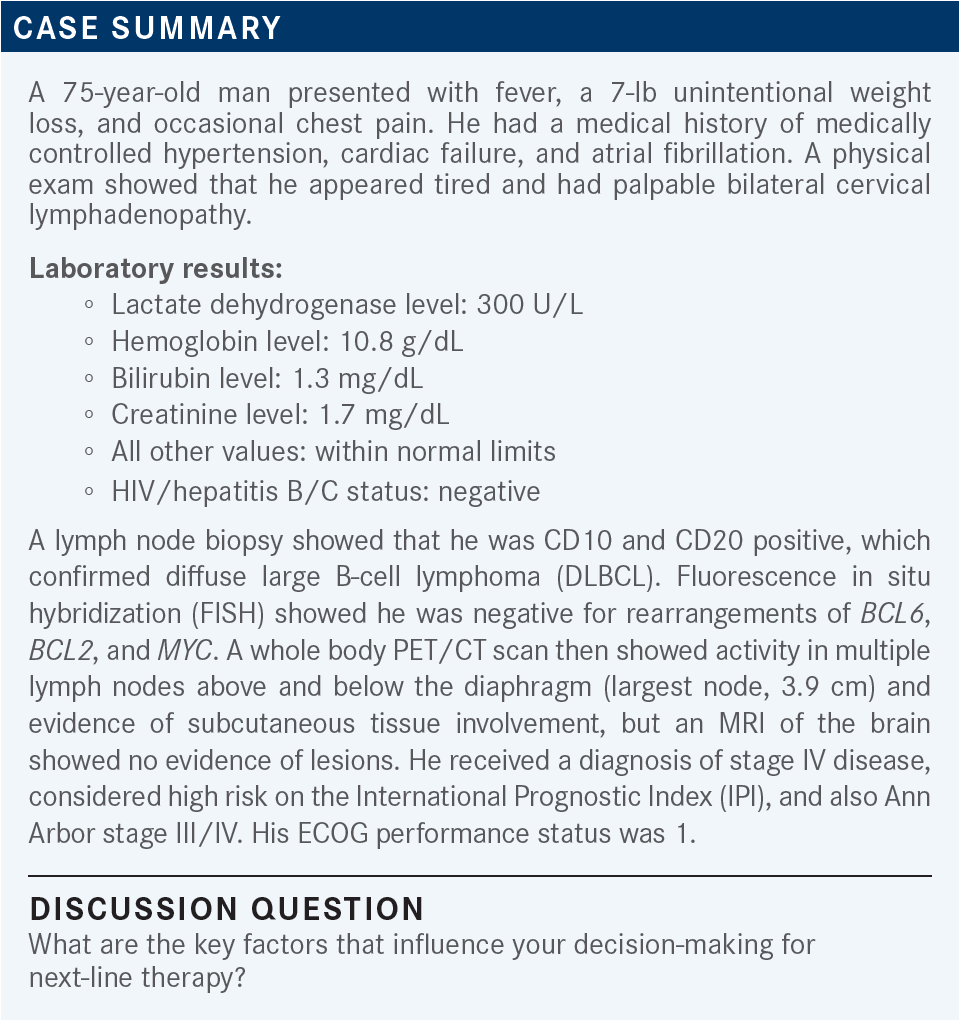
Roundtable Discussion: Torka Assesses the Evidence for New and Emerging Treatment Approaches in DLBCL
During a Targeted Oncology case-based roundtable event, Pallawi Torka, MD, discussed with participants the use of novel therapies for patients with diffuse large B-cell lymphoma.
Pallawi Torka, MD (Moderator)
Assistant Professor of Oncology
Lymphoma Section, Department of Medicine
Roswell Park Comprehensive Cancer Center
Buffalo, NY

UNGER: I think performance status and goals of care for the patient are critical. This is an older gentleman with high-risk factors [and an imperfect] performance status. Many of the options are things that I have not used, so I don’t have a good handle on some of these things, such as CAR [chimeric antigen receptor] T-cell therapy, in terms of how rigorous that is for a patient at this age.
TORKA: Absolutely, the goals of care are important, especially when the toxicities could be great. Anybody else?
GEORGES: I think all those factors are important and need to be considered. Patients who are not eligible for stem cell transplant could still be eligible for CAR T-cell [therapy], so they should be at least offered that to see if it’s something that they’re interested in.
I live about an hour and 20 minutes away from a CAR T-cell center. A lot of patients don’t jump on that option right away and they need to be monitored closely afterward and need to be close to that center, so it’s not their preferred option. But it is a good option for the right patient, because it is potentially a [curative] therapy, so it’s a [matter of] preference for the patient. [The choice should be based on] how aggressive they want to get [as well as on] what their performance status is and what their insurance allows. I think they need to factor all that into consideration [regarding CAR T-cell treatment].
KAPPEL: I think the point here that needs to be stressed is the difference between the community setting and the academic setting and the coordination between the 2. One of the key things that has happened over the last 10 or 20 years is that with some of these newer drugs, not necessarily CAR T-cell therapy but with azacitidine [Vidaza], decitabine [Dacogen], and others, the community didn’t give them at first and now the community gives them routinely.
For this, you want to coordinate the therapy with the transplant center or CAR T-cell center, which may be the same. You don’t want to give a therapy that’s going to get a patient excluded from a clinical trial or from one of these [other] therapies. So it’s a chess game, and you’ve got to think a couple steps ahead, and when you have a situation like this, I feel it’s important to communicate with your academic center that the patient should be referred there early on rather than later.
TORKA: Does the timing of relapse [influence] your decision at all, [if, for example,] the patient relapsed soon after R-CHOP [rituximab (Rituxan), cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate (Oncovin), and prednisone]?
KAPPEL: The timing of relapse is important in terms of how sick the patient is and their risk of disease progression and their odds of response to the initial therapies. But the community setting, for these relapsed patients, is not necessarily the correct place. I strongly believe that 95% of cancers can be taken care of in the community setting, but this [population of relapsed patients may represent] that 3% or 4% that need to be in the academic setting, and I don’t care when they relapse; if they relapse, they need that academic referral.
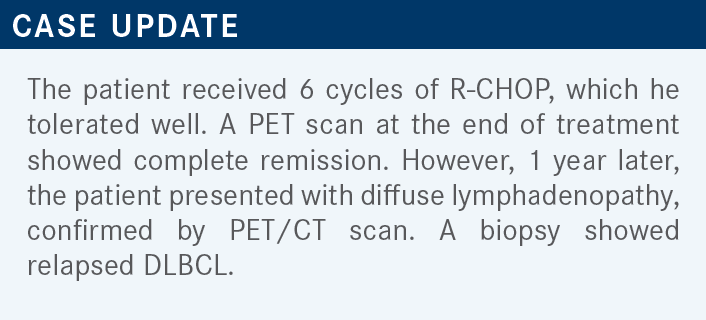
TORKA: [Having a majority of my patients on CAR T-cell therapy] is something that has been hard [for me] to achieve, even at an academic center. So I would like to know how someone can get a majority of patients in.
ISUFI: I work at Yale, and [on the basis of] the recent data, we’ve already started to take CAR T-cell therapy patients who would otherwise have gone for transplant, so I think that’s where we’re going. If most academic centers [have been taking] 50% of relapsed patients [for autologous stem cell transplant], …those patients are probably going to [have] CAR T-cell therapy now. Clearly, the cutoff criteria are much more lenient for CAR T-cell therapy, so I think more patients will qualify. What’s going to make it difficult is that with the referrals from the community, when we were taking those patients for transplant, there was some time to arrange everything because [they] were getting bridging therapy with R-ICE [rituximab, ifosfamide, carboplatin, and etoposide phosphate] or R-DHAP [rituximab, dexamethasone, cytarabine, and cisplatin].
I think what we’re seeing now is that if patients are primary refractory and you’re considering them for CAR T-cell therapy right away, then you don’t have much time. If you don’t want to give the patients second-line therapy, you need to get insurance approval and collect [the T cells]. That’s challenging, but I think we’re going to see more and more patients getting CAR T-cell therapy in place of transplant, [based on] the recent data.
With transplant, primary-refractory patients and early-relapse patients, like this one, do not have good outcomes; moreover, the cure rate is less than 30% if they fail a rituximab-containing regimen. I think patients like this would benefit from CAR T-cell therapy, even at the age of 75. At Yale, and in clinical trials, we’ve treated patients in their 80s, so I think it’s doable, but you just have to make sure that they have social support and don’t have any major comorbidities. I anticipate that we’re probably going to treat [51% to 75% of patients eventually].
TORKA: You bring up a good point: that a retrospective analysis of older adults vs younger adults who got CAR T-cell therapy [showed that despite] an increased risk of immune effector cell–associated neurotoxicity syndrome [in the older group], the rate of cytokine release syndrome was the same [between groups].1 The complete response and overall response rates were also higher [in the older group]. We should not discount people from CAR T-cell therapy just because of their age, but you have to select [patients on the basis of] fitness and such factors.
KIM: The way I look at it is that we have many treatment options here, and I try to preserve patients’ performance status and quality of life, and scheduling more tafasitamab [can be a struggle]. It’s a weekly regimen and [so it was] hard for the patients to come in for the treatments in the middle of COVID-19. Polatuzumab vedotin [can also cause] peripheral neuropathy. [My goal is] to preserve quality of life, and I think about the adverse event [AE] profile, the disease burden, and scheduling, and I think we can have the patients do one thing at a time and have them live longer and improve their quality of life.
PREET: The patients we see in my practice, [which] is basically in downtown Brooklyn, New York, have a lot of complications. Sometimes they have HIV and other problems as well. So for me, the cytopenias are a big deal. With polatuzumab [vedotin] and rituximab, that can be a problem. I don’t have much clinical experience with loncastuximab [tesirine] or with tafa-len. I would like to use one of these as soon as I get a [suitable] patient, and I think loncastuximab might be preferable because it’s a single drug.
TORKA: Do you have trouble using lenalidomide because of the paperwork [required] with Celgene, insurance issues, and needing to go through a specialty pharmacy?
PREET: No, [but] using lenalidomide requires a lot of steps. And then we have to keep reminding [our patients] to take their surveys and sometimes we have to bring them [in to] our clinic to get them to do the survey. Sometimes you can [avoid these struggles], but because of the population we have, [including] a lot of patients with myeloma, we have a lot of patients on lenalidomide.
ISUFI: We have to look at the patient’s individual situation in terms of their comorbidities and organ function. Something to keep in mind with lenalidomide is that it does increase the risk of arterial and venous thrombosis.2 For example, in patients with cardiac comorbidities or ones who have a history of deep vein thrombosis or stroke, lenalidomide may not be the best choice. Also, for patients who have renal insufficiency, you’re never going to be able to use the high doses. In practice, when you combine lenalidomide with an anti-CD20 therapy, patients become neutropenic and they require significant dose reductions.
That’s something to keep in mind with lenalidomide. If a patient has severe peripheral neuropathy, I would not consider pola-BR because the dose-limiting toxicity of polatuzumab is peripheral neuropathy. I would use tafa-len in patients [who have had] only 1 line of therapy [From the Data3]. I would use it early on, in patients who are not transplant eligible, who have failed their up-front regimen, and who are frail. I prefer pola-BR [for patients who have] relapsed after transplant or have had more than just 1 line of therapy. For loncastuximab [tesirine], someone who has bad DLBCL with, for example, pleural effusions, might not be a good [candidate for that drug] because of the AEs of effusions. I just don’t think we have enough data.
There are some limited data [that show] that patients who received CAR T-cell therapy responded to loncastuximab [tesirine], and so in the post CAR T-cell setting, if the patient is still CD19 positive, I would give them loncastuximab because it’s a single agent. I’ve tried tafa-len and pola-BR after CAR T-cell therapy, but you have to do dose reductions.
It’s tough because the patients have a lot of cytopenias, so that’s usually what I’m thinking about when I decide between these regimens. I look at the trial [data] that led to the approvals and at the patient populations [that were studied in each]. I ask myself: Does my patient fit into [1 of those] categories? And what organ dysfunction or toxicity from prior therapy might preclude the use of [a given regimen] in my patient?
ROSENBERG: Can I just add, from a practical standpoint, that a regimen that requires an [infusion] every week for months is a little bit of a problem for an older, frailer population, so that would factor into my choice.
TORKA: Yes. If the patients do respond, the response lasts for a long time, which is the strength of the regimen, but logistically it is difficult.
REFERENCES
1. Lin RJ, Lobaugh SM, Pennisi M, et al. Impact and safety of chimeric antigen receptor T-cell therapy in older, vulnerable patients with relapsed/ refractory large B-cell lymphoma. Haematologica. 2021;106(1):255-258. doi:10.3324/haematol.2019.243246
2. Revlimid. Prescribing information. Celgene Corporation; 2022. Accessed September 11, 2022. https://bit.ly/3UzdraH
3. Duell J, Maddocks KJ, González-Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021;106(9):2417-2426. doi:10.3324/ haematol.2020.275958