Roundtable Discussion: Participants Reflect on Sending Blood- Vs Tissue-Based Tests in NSCLC
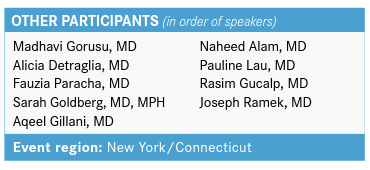
During a Targeted Oncology Case-Based Roundtable event, Grace K. Dy, MD and 9 other physicians discussed molecular testing for patients with non–small cell lung cancer.
Grace K. Dy, MD

During a Targeted Oncology Case-Based Roundtable event, Grace K. Dy, MD, the chief, of Thoracic Oncology, and associate professor of Oncology in Department of Medicine at Roswell Park Comprehensive Cancer Center, and 9 other physicians discussed molecular testing for patients with non–small cell lung cancer (NSCLC).
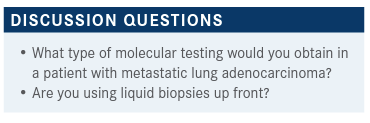
GORUSU: Usually our pathology department does a baseline next-generation sequencing [NGS] for patients with metastatic disease—that’s our routine. If for any reason there was inadequate material to do anything additional, then I have been using the blood-based Foundation Medicine [test], or whichever company. That has been my practice.
DY: Is that a reflex test that your pathology [department] will do when they diagnose adenocarcinoma, or do you have to separately order your NGS?
GORUSU: They do it routinely. DY: What kind of panel—do they routinely send it out to Foundation Medicine?
GORUSU: No, they do the NGS in house. If the pathologist tells me they do not have enough material to do anything other than giving me the diagnosis, then I do the peripheral blood-based [test] as well. I [also] send in for Foundation Medicine on the diagnostic material.
DY: That’s great to know. Would anyone else like to chime in on what their pathology and clinical practice is?
DETRAGLIA: I practice in a small community practice, so we do not have in-house testing and our pathologists are still not routinely sending these unless we request it. So I would agree with the previous speaker that we will try to do it on tissue first. I have to add, I would do Foundation Medicine testing on the biopsy. If there’s not enough tissue, then we would do peripheral blood testing. My understanding is it’s probably best to do peripheral blood testing when the disease is active as opposed to in remission or after you’ve started treatment. Is that the case?
DY: I think the sensitivity is the issue with the circulating tumor DNA [ctDNA] analysis, so yes. Even when you have active metastatic disease, if your disease burden is low the probability is also low. But yes, you’re right on the ball.
PARACHA: We also have the same thing. We have a whole setup in which all the tests are already picked up and it’s automatically done unless [there is not enough] tissue. It was not the case up until recently, but now we do the same thing.
GOLDBERG: Very recently, I started to do something a little differently from what others have said with the blood-based testing. I don’t know how it is at other people’s institutions or if you use send-out molecular testing, but it takes a couple weeks to get our testing back. We do in-house testing but it’s 2 to 3 weeks, I would say, at minimum. If I ask them to rush it, maybe it’s 1 to 2 if I’m lucky. So if it’s already done, I’m happy with that if I get a result. But if by the time I see the patient it’s still not back or if it hasn’t been sent yet, I’ll send blood [test] even then.
I used to do what you all are saying and then, just really in the last month or 2, I’ve started to just send it. I haven’t had an issue with insurance. That’s often what people bring up as issues; you’re getting 2 rounds of testing. But I’ve been able to get it much faster and sometimes you find things in blood that are not in tissue, and [in] tissue that are not in blood. So I’ve found it to be a pretty good way of doing things lately.
DY: Are you guys sending the ctDNA to Foundation Medicine, Guardant Health, Resolution Bioscience, or [somewhere else]?
GOLDBERG: We don’t have our own in-house ctDNA [testing], so we use a commercial assay. I tend to use Guardant Health; it’s just what I started using and I really like their platform. I’ve only ever worked with them. I don’t know others as well, but if you have questions or an issue, or you need a rush, they’re just easy to work with. I’m not trying to advertise for them; I’ve just had a good experience with them. I’m sure other companies are fine as well. I know a lot of physicians use Foundation Medicine too.
GILLANI: [At my practice], we are having this debate with our pathologists; it’s not clear. They were all doing the 7 biomarkers and, honestly, most of the individuals are not familiar with the 7 biomarkers. So we are encouraging them to get testing done in patients with non–small cell lung cancer and make it a reflex regardless of the stage of presentation because I think it gets to be confusing, who gets tested. With the osimertinib [Tagrisso] approval in the adjuvant setting, everybody should have EGFR testing done, but it is not very clear to our pathologists right now and I think we are still having that discussion with them. Could you paraphrase what you said about what your approach was toward liquid biopsy or ctDNA? I don’t know if I completely understood your thought process there.
GOLDBERG: I think of them as complementary tests. There have been some nice studies that tissue can pick up things that blood sometimes misses, and then sometimes you find something on blood that you may have missed on tissue. I’ve had both experiences with patients. I don’t think doing both is wrong, but the way that I typically do it is if I have the results back from tissue by the time I see a patient and it shows me something useful, like a driver mutation, I don’t necessarily send blood. But if the test is pending and I’m worried it’s going to take a while, I typically have been just sending blood up front while I’m waiting for tissue tests. Then I wait for 1 or the other or both to come back to figure out what to treat someone with.
GILLANI: Do you get any pushback from the third-party insurance?
GOLDBERG: I’ve not. That used to be my concern, but I haven’t had the issue. I’m curious whether other physicians have done this and had issues with it, but I haven’t. I’ve talked to others who haven’t either. Some of the companies have nice programs where they will see if there are going to be big co-pays, or insurance isn’t going to pay, and then they’ll let the patient know things like that.
GILLANI: So when you fill out the form, you [do] reflex to liquid testing if the quantity is not sufficient, or something like that, right?
GOLDBERG: I don’t wait for quantity not sufficient. I do it before I even know because they’ll think quantity is sufficient and then they don’t get results, cellularity is low, or whatever it is—or it just takes too long and I don’t want to wait all those weeks. So I just send it. But I don’t know; our pathologist won’t send it because it’s a blood test. We send it straight from the office.
ALAM: We have noticed that Foundation Medicine was taking a little bit longer than usual during the pandemic. So often we will send the liquid also, and we haven’t had any [issues].
DY: I think at least for Guardant Health—I haven’t tried Foundation Medicine for their liquid panel—they have great support so far, but I’m not advertising for Guardant. They don’t balance bill patients. So if the insurance doesn’t cover, to some extent you don’t want insurance to cover, patients may have a co-pay. At least their byline right now for the business is stable, not balance bill. So I have more problems with tissue-based authorization. The delay—some insurances will not cover for the NGS multi-panel. But if I get the answer with Guardant Health, I sometimes even cancel the tissue-based testing.
GILLANI: Aren’t there any studies that show that this [is] cost-effective? How much is the overlap between the 2? What are the kinds of things that won’t pick up on tissue testing that you pick up on ctDNA?
DY: I don’t think there are any formal cost-effective analyses yet. Certainly doing it both at the same time will not be the most cost-effective approach. It will be appropriate in certain settings, and I think you have to factor in disease burden and your degree of likelihood that you’re predicting for patients having something that will come back, based on their disease burden. I don’t think it will be cost-effective.
GOLDBERG: I agree. I factor in that as well. Someone with minimal disease, where I feel it’s fine to wait a couple of weeks and ctDNA is likely to be negative anyway, I would probably not send it. But someone with [multiple] liver metastases, in 2 or 3 weeks terrible things could happen and I’d rather know sooner. Guardant has been turning it around in about a week, so it’s really fast.
GORUSU: When I use the term “liquid biopsy,” I did not exactly mean ctDNA. When I say liquid biopsy, be it Foundation Medicine, Guardant Health, or Tempus, that’s a peripheral blood-based [test]….I thought, please correct me if I’m wrong, the FDA approval was only in the stage II and III colon cancer for the ctDNA. So is insurance approving it when we do the ctDNA?
My other question is, that’s a little bit process involved, right? You need to simultaneously have the blood-based and the tissue for the ctDNA correlation is what I thought.
GOLDBERG: I was using the terms synonymously, of liquid biopsies and ctDNA. So liquid biopsy meaning a blood-based test to assess the mutation status, and what you’re looking at is the ctDNA. I think physicians have maybe typically used those interchangeably.
In terms of whether this will be covered in the future, I don’t really know. It is approved as of now. I’m not sure I’m so up on my exact FDA approvals on this. But it is sufficiently covered that I’m not having a problem getting it for my patients for stage IV disease.
In terms of will it be available in the future, will someone crack down on it? Maybe. There are studies that show that you find things in 1 that you don’t find in the other, and when you do both you have an increased chance of finding an alteration. I think that this is so important. It’s the foundation of everything we do, because we need to know those results to be able to choose the best treatment. I don’t know what’s going to happen in the future. I know that right now we’re able to do both. I don’t do it in all patients, but I’m increasingly doing it when I don’t have tissue testing and someone needs results quickly.
DY: Yes, all good points, and the correlation between tissue and blood is fairly high. But, as Dr Goldberg mentioned, sometimes you can pick up 1 that you don’t see in the other. Particularly since this is liquid based, you might find, let’s say, a KRAS mutation; it may or may not be a reflection of the lung cancer, because what if you have some other disease process that is RAS mutated, for example? We’ve had instances of synchronous malignancies, for example, where [tests] detect a BRAF mutation in the blood, but then they turned out to have a hematologic malignancy that was the BRAF. Then you test the tissue [and] it’s a completely different alteration.
GOLDBERG: There’s so much [data] now. We don’t have any head-to-head comparison trials, so we don’t really know which [agents] are best. You can have a 2-hour conversation with every patient with first-line lung cancer about the different options; there’s just so much. So I think any of the [available choices] are reasonable.
We’ve had a lot of the ipilimumab [Yervoy]/nivolumab [Opdivo] trials open, so I’ve used that regimen a lot [for patients] on trials. I find it tough; I almost feel like the toxicity [data] underestimate what I see in clinic. You can look at percentages, but it doesn’t entirely capture how long someone’s on steroids for their pneumonitis or that they needed to be hospitalized because they had recurrent colitis.
I think it’s a great potential option, but because I think we don’t know the benefit over chemotherapy/pembrolizumab [Keytruda], I tend to err toward chemotherapy/ pembrolizumab, with maybe the exception of the patients who are otherwise healthy with very good performance status. Those are the ones I think of for the nivolumab/ ipilimumab regimen. It can be tough.
DY: I completely second the motion, and especially if they’re older. So, if you look at the [data], older patients, probably because they’re frailer, have more comorbidities…a lot of our lung cancer patients are elderly. As Dr Goldberg mentioned, [with] the chemoimmunotherapy with ipilimumab/nivolumab as the immunotherapy backbone, I would be more selective because of the concerns about toxicity. It’s still manageable at everybody’s comfort level, but I tend to avoid it unless [the patient has PD-L1 expression of] less than 1%.
GUCALP: We are discussing studies, but when you get to the real life, 85% to 90% of patients don’t fit the studies. You must make decisions based on a gut feeling or prior experience. What factors influence my decision-making: Degree of their PD-L1 positivity, comorbidities like interstitial lung disease, or [needing] disease-modifying drugs; that will put me away from the immunotherapy to go to the chemotherapy base. ECOG performance status and frailty of the patient [are also] involved in the decision tree.
Carboplatin/pemetrexed [Alimta]/pembrolizumab is standard at this moment. We must really use judgement, because studies, as good as they are, don’t represent the patient population we treat.
ALAM: Ipilimumab/nivolumab, if it’s [used] appropriately, can be tolerated. I agree that the adverse events [AEs] are there, but…if you select your patient population, it’s manageable.
[We] do see the toxicity, but we monitor them very closely. There are those patients [who] will get colitis and [other toxicity], but you see that with pembrolizumab. But if you watch them carefully, and hopefully catch them before it gets worse, it’s doable.
DY: Let’s say the patient is in their 60s, not too frail, great performance status, and not a lot of comorbidities. If you have the choice, and patients say, “Doctor, you decide for me,” which one would you choose if they can be candidates for both the ipilimumab/nivolumab and pembrolizumab?
ALAM: I’m comfortable using ipilimumab/nivolumab. Right now, we don’t have the ability to be able to predict who gets the immune-related AEs. I feel that patients tolerate it better if they don’t get into the immune-related issues. Sometimes I feel they tolerated it better than carboplatin/pemetrexed/ pembrolizumab. Future trials will tell us which way it’s going to go, but I feel that people tolerate it, and if they are going to get those immune-related AEs, they are. That can happen with pembrolizumab.
GORUSU: I totally agree. With ipilimumab at 1 mg, I have seen patients tolerate far better than the chemoimmunotherapy; at least that has been my experience. One of my patients who had renal cell carcinoma had partial nephrectomy and creatinine level of 1.4 or 1.5. It is an adenocarcinoma, and the PD-L1 expression was there, not less than 1%, definitely high enough. I opted to start her on the combination of ipilimumab/nivolumab because I was more worried about how she would tolerate chemotherapy rather than this.
In general, when I have put patients on ipilimumab/ nivolumab, they [do] very well for the most part. So I’m comfortable using the combination immunotherapy.
RAMEK: My experience with ipilimumab/nivolumab is that it’s not toxic at all. Rare cases of autoimmune problems emerge, but overall I think it’s much better tolerated than chemotherapy. In particular, I see no problem in the elderly population at all. In fact, I would prefer to use ipilimumab/nivolumab in older patients than chemotherapy. I really don’t understand why the patient’s age should make us more worried about using ipilimumab/nivolumab. I’d be more worried about using chemotherapy in that population.
DY: Would you choose ipilimumab/nivolumab more often or would you incorporate chemotherapy the first 2 cycles?
RAMEK: These patients are all going to die of lung cancer, so the question really is how not to squander their remaining time and not to add to their misery. I think that double immunotherapy gives us the best chance of a durable remission for a certain percentage of patients without practicing the weird homeopathy that chemotherapy traditionally has been, where we superimpose suffering on suffering. I’m happy to avoid chemotherapy.
DY: So you would preferentially do ipilimumab/nivolumab only versus adding the chemotherapy if I’m understanding correctly?
RAMEK: Yes. I think doing an early PET scan and seeing what’s going on can be helpful, also. I think it’s clear [when] patients are responding or not responding. I think at the 1 mg/kg dose, I don’t see the toxicity. As a matter of fact, today, for example, I had an 85-year-old woman getting the combination. Her daughter happens to be a professor of oncology at the University of Chicago. She’s monitoring things, looking over my shoulder, [the patient] is tolerating this exceedingly well. The experience of many people speaking tonight is that this is a highly toxic regimen, but to me ipilimumab/nivolumab is very much what I remember an anesthesiologist telling me about his profession. He said it was hours of boredom and seconds of terror. In a way, ipilimumab/nivolumab’s the same thing. It’s like nothing happens, there is no toxicity. We don’t give them premedications. How often do you have patients coming into the infusion room where you give no premedication?
GOLDBERG: The ipilimumab [we use] is stronger in Connecticut, I think is the issue. It’s helpful to hear all of your comments and your experience with it. I’ve seen pretty significant toxicity with the combination, and I don’t think of it as an age issue; I think of it as if I think a patient can tolerate grade 3 or 4 pneumonitis, pericarditis, or myocarditis. I’ve seen several patients recently with myocarditis from ipilimumab/nivolumab, a myositis. There’s been some significant toxicity. So I don’t think of it as an age cutoff, I think of it more like if I don’t think they’re going to tolerate a significant toxicity, I might be more concerned, especially when we don’t know that there’s a benefit of ipilimumab/nivolumab versus single agent immunotherapy or chemoimmunotherapy. I think it is a very reasonable option. I think the data in the less than 1% [PD-L1], whether it’s for ipilimumab/nivolumab alone, or ipilimumab/nivolumab/chemotherapy, is the most compelling to me, where the benefit is most clear, which is why it’s interesting that that wasn’t what was approved. But I have caution with it. I use it, I just am careful with who I select.